Circulation and Coagulation
Why Vitamin K Cannot ‘Over-Clot’ Your Blood
This page will describe the circulatory system, which keeps blood circulating through the body and the coagulation system, which ensures that blood will properly coagulate and form a clot, if an injury has occurred. This review will cover the primary elements of these very complex systems, as they would take place in a healthy person. Both of these systems depend on sufficient amounts of vitamin K being available. Vitamin K does not initiate the formation of a blood clot, nor does it resolve or dissolve a clot. However, vitamin K does improve the functioning of both these systems. The key role of vitamin K in making sure these systems work effectively, and the research behind it will be reviewed and explained.
The following is the peer reviewed research behind vitamin K and its role in these systems.
CIRCULATORY SYSTEM
The circulatory system is enormous, containing approximately 60,000 miles of blood vessels, arteries and veins. It’s charged with delivering nutrients and oxygen to every cell and on the return trip, it removes waste products from the lungs, kidneys, spleen, and liver. Blood is the medium that makes all this possible with help from the heart.
Blood is a liquid that circulates throughout the body in every artery, vein and capillary. Blood flows freely, yet at the same time, it contains the capability of engaging instantaneously, in the formation of a lifesaving clot, within a matter of seconds, localized to the area of need, while the rest of the blood continues to flow through the body, undisturbed.
This delicate balance is achieved because the body has chemical elements that are anti-coagulant most of the time, maintaining the circulating blood in a fluid state, and chemical elements that are pro-coagulant, and prepared to clot when needed. This ‘dance’ is accomplished by an interactive and highly regulated network of proteins contained in the blood that maintain the flow, yet which can coagulate in seconds.
Our blood has two main parts, blood cells and plasma. The plasma is the liquid part of the blood. It is mainly water. It contains proteins, fats, salt, and other substances. Those proteins are sent into the bloodstream, typically from the liver, to circulate around the body, in an inactive form, ready for action at any time, poised to participate in blood coagulation upon tissue insult or injury. Some of the proteins work to form a clot and are called clotting factors.
Red blood cells carry oxygen to all parts of the body, and carry back carbon dioxide to the lungs. White blood cells help fight infection. Platelets are tiny blood cells that help stop bleeding. Platelets are produced in bone marrow. Platelets circulate in the blood in an inactive, resting form for an average of 10 days. The exterior of a platelet, its membrane, is coated with receptors that are targeted by various proteins and this membrane is a key element in clotting.
If there is any injury, the circulatory system must work to stop the leak, and repair the ‘pipe’. That is when the coagulation cascade begins. In the cascade, a series of actions take place, where blood is transformed from a liquid into what becomes eventually becomes a blood clot.
The success of this system all depends on the vitamin K. Vitamin K is a necessary ingredient in the circulation of blood throughout the body. The presence of vitamin K is necessary both for the coagulation capacity that it is well known for, but also for the fluidity and the anti-coagulant properties, which is not as well known (Jesty & Beltrami, 2005).
Vitamin K is well known for its role in coagulation, and it can be a common misconception that if one takes a vitamin K supplement, the additional amount of vitamin K would result in your blood coagulating excessively, or ‘over clotting’, plugging your veins and you would die.
This outcome is impossible and the following information will help provide a background on the science of coagulation, the function of vitamin K, and why it is impossible to ‘plug up’ or ‘over clot’ your blood.
ANTI-COAGULATION
Typically, blood maintains its fluidity as it circulates throughout the body. This is referred to as an anti-thrombogenic or anti-coagulant state. This fluidity is no accident, but is due to a precise and balanced regulatory control by the anticoagulant system. The system includes certain processes and mechanisms to keep the coagulation cascade in check (Colvin, 2004), and actively works to prevent excess coagulation, which could produce widespread, unnecessary clots. It is also involved in localizing a clot, so that it only forms where needed at the site of an injury. The main anticoagulant mechanisms naturally present in the body include the following:
Platelets.
Platelets participate in the anticoagulant pathways. They secrete several inhibitors which serve to terminate the procoagulant process. For example, platelets release the enzyme plasminogen, which degrades the clot, and initiates tissue repair (Lanzer & Topol, 2013).
Vessel Wall.
Another mechanism is the vessel wall, which contains endothelial cells. Endothelial cells line the wall of the blood vessel and secrete coagulation inhibitors, like protein S on an ongoing basis (Stern et al, 1985; Fair et al, 1986). These inhibitors can rapidly inactivate the enzymes that promote coagulation enzymes. Some of the primary coagulation inhibitors secreted by the endothelial cells are discussed below:
One primary inhibitor is thrombomodulin, which is a membrane protein and is expressed on the surface of endothelial cells and serves as a cofactor for thrombin. Thrombin is a key enzyme of coagulation, however thrombomodulin can convert thrombin to an anticoagulant (Moussa, 2011; Yasuda, 2016). Thrombin also participates as an anti-coagulant by activating plasminogen to plasmin, which degrades clots while stimulating the production of other enzymes that inhibit coagulation.
Endothelial cells also secrete PA1-1 (plasminogen activator inhibitor) which helps convert plasminogen to plasmin, and creates resistance to clotting (Phillips et al, 1984). Plasmin will dissolve the old fibrin at injury sites and any fibrin which may be deposited in normal vessels, as well as fibrin blood clots (van Hinsbergh et al, 1985; Sakata et al, 1985).
Endothelial cells also produce tissue factor pathway inhibitor (TFPI), an anticoagulant protein. Tissue factor pathway inhibitor acts as a potent, natural inhibitor of the coagulation pathway, inhibiting major enzymatic complexes that would initiate the coagulation cascade (Broze, 1995; Bauer & Zwicker, 2003).
The endothelium also regulates the activities of circulating blood cells. When undisturbed, the endothelium actively prevents platelets from gathering together. Interactions between endothelial cells, platelets, and white blood cells are prohibited. These interactions are mediated by a wide array of soluble compounds and adhesion molecules (Celi & Lorenzet, 1997).
The endothelial cells also provide receptors for proteins in the blood that interfere with clot formation, (protein C), and promotes protein C pathway effects (Esmon, 1987; Esmon, 1989). Protein C is a major anti-coagulant. This means that unwanted clots are not formed, and embolisms don’t cause injury (McCarron, Lee & Wilson, 2017).
Circulating Elements
There are chemical elements circulating through the bloodstream that are anticoagulant forces.
A naturally occurring anticoagulant protein produced in the liver and circulating through the body, is antithrombin (AT), which functions as a mild blood thinner. It acts like a police protein that prevents you from clotting too much. Antithrombin binds coagulation factors, such as thrombin, which then form inert complexes, inactivating their clotting potential. This action is greatly enhanced (a thousand fold) by the presence of heparin, a substance formed by connective tissue cells (More et al, 1993; Liu & Rodgers, 1996; Broze, 1995; Stern et al, 1985; Shuman, 1986; Casu et al, 1981; Lindahl et al, 1980, Marcum & Rosenberg, 1984; Tollefsen & Pestka, 1985).
Also circulating are Protein C and S, which are proteins in the blood that help regulate blood clot formation. They work in concert as a natural anticoagulant system, mainly by inactivating clotting factors V and VIII, which are required for clot generation. Protein C works in conjunction with Protein S.
Vitamin K
Vitamin K has an important role in regulating the anti-coagulation system, and keeping the blood fluid (Espana et al., 2005). While vitamin K is primarily known for its role in clotting, it is also a key component in preventing blood clots. There are anticoagulation proteins which all depend on sufficient amounts of Vitamin K to be functional and, thus, active. These elements are known as protein C, protein S, and protein Z. (Esmon et al 1987: Lobato-Mendizabal & Ruiz-Arguelles, 1990; Grober et al, 2015).
Note: Vitamin K’s number one job is anti-clotting!!!
In the presence of Vitamin K, these proteins are carboxylated, which means that carboxyglutamic acid is brought into the protein and modified into Gla. Gla has an affinity for calcium ions (Friedman & Przysiecki, 1987; Vermeer, 1990). The calcium induces structural changes in the Gla domain which facilitate its interaction with the surface membrane of the cell (Freedman et al, 1996). This is a key mechanism for both the anti-coagulant and the coagulant systems.
The carboxylation and resulting changes in the Gla domain of the proteins are essential for them to be functional and active (Suttie, 1993). If the active forms of the protein are low, due to insufficient vitamin K, than there can be increased coagulation in the blood vessels which can result in abnormal clotting, sometimes with devastating consequences (Dahlback, Villoutreix, 2005).
Protein C
Protein C is a potent vitamin K-dependent, anticoagulant protein. The activation of protein C and the components involved have been termed the protein C pathway. The protein C pathway serves as a major system for controlling thrombosis or blood clots by inhibiting blood clotting factors V and VII, which limits coagulation. The essential components of this pathway involve the enzyme thrombin, thrombomodulin, the endothelial cell protein C receptor (EPCR), protein C and protein S (Esmon, 2003; Kisiel et al, 1977).
Thrombomodulin is a membrane protein, which is expressed on the surface of endothelial cells. Thrombomodulin serves as a cofactor for thrombin, which is the principal enzyme of clotting. When thrombomodulin binds to thrombin, thrombin is inactivated, and cleared from circulation more than 20 times faster than free thrombin, thus reducing the risk of clots forming. Essentially, thrombin is converted to an anticoagulant, instead of a coagulant, inhibiting its clotting and cell activation potential.
Also the formation of the thrombin-thrombomodulin complex augments protein C activation, leading to a 1000-fold increase in the production of activated Protein C (APC), which is a potent anticoagulant. APC degrades clotting factors, limits coagulation and prevents clot formation in areas of undamaged endothelium.
Protein C also indirectly degrades fibrin within a clot.
Protein S
Protein S (PS) was randomly discovered in the 1970s as a new vitamin K-dependent plasma protein in Seattle and therefore, named after the city of its discovery (Di Scipio et al, 1977). Protein S is a natural anti-coagulant with multiple biologic functions. The best characterized function of Protein S is its role as a cofactor to Protein C. The action of Protein C is enhanced when bound to Protein S (Stern et al, 1985; Fair et al, 1986).
Activated protein C (APC) requires protein S as part of the Protein C pathway (Castoldi & Hackeng, 2008). Whenever procoagulant forces are locally activated to form a clot, protein S participates in controlling clot formation (Soare & Popa, 2010; Castoldi et al, 2010; Marlar et al, 2011). As a cofactor, protein S helps to inactivate two clotting factors, FVa and FVIIIa, which dampens and shuts off clotting. A deficiency in the level of protein C or protein S is associated with an excessive tendency to form clots (Marlar et al 1982; Takashi et al, 1986).
The importance of protein C and protein S is demonstrated by the fact that deficiency of either is associated with increased risk of thrombosis or clotting (Bertina, 1985; Comp et al, 1984).
Protein Z
This is the most recently described component of the anticoagulant system. Protein Z is a vitamin K-dependent protein, which functions as a cofactor that dramatically enhances the inhibition of some coagulation factors. For example, in the presence of protein Z, the ability to inhibit clotting factor Xa is increased 100-fold ( Corral et al, 2007).
Thus, there is a potent system of anti-coagulant forces present in the body, maintaining the fluidity of blood and inhibiting clot formation throughout the body. Vitamin K is a necessary component, enhancing the effectiveness of the anti-coagulant system. With the presence of sufficient vitamin K, the proteins C, S, and Z are carboxylated and active.
If there was insufficient vitamin K available, the anti-coagulant proteins may be insufficiently carboxylated, with fewer of the proteins being active, leading to an increased risk of clots. Ironically, while Vitamin K is well known for its role in helping blood to form clots, it is also very necessary to prevent clots from forming (Esmon et al, 1987: Lobato-Mendizabal & Ruiz-Arguelles, 1990; Grober, et al, 2015) .
The anti-coagulant system is not triggered not is it resolved by vitamin K. The anti-coagulant system functions regardless of the presence of vitamin K, however, its effectiveness in preventing clots is improved with sufficient amounts of vitamin K.
Note: you are primarily in an anti-coagulant state, with your blood circulating
throughout your body, and vitamin K makes that happen.
COAGULATION
Typically, the anti-coagulation system maintains the fluidity of blood as it circulates throughout the body, and actively prevents clots from forming. However, if there is a threat to the integrity of the vascular system, then the body responds by forming blood clots, to ensure survival. The threats could consist of a trauma, injury, inflammation, infectious agents, or pathological situations such as surgery. These threats trigger a cascade of biochemical reactions known as the coagulation cascade.
Coagulation Cascade
The coagulation cascade is a pathway containing many biochemical steps that lead to the formation of blood clots during tissue injury. The clotting mechanism involves a multistep cascade of enzymes, whose jobs are mostly to activate the next enzyme in the cascade. In this cascade, the blood-clotting proteins assemble into a complex on the membranes of platelets and on endothelial cells in the vessel wall. These complexes allow the factors to efficiently contact one another to become activated and participate in clot formation.
There are many steps to this complex cascade.
1. First the blood vessel gets smaller, also known as vasoconstriction, where the damaged blood vessels narrow to reduce blood loss. Vasoconstriction is produced by vascular smooth muscle cells and is the blood vessel’s first response to injury. Blood vessels are lined with smooth muscle cells called endothelial cells, and these cells trigger the muscles to contract. Normally, the endothelial cells express molecules that inhibit platelet adherence and activation while platelets circulate through the blood vessels. However, when injured, the damaged cells release endothelin, promoting vessel constriction in an attempt to limit blood loss.
In this initiation phase, the blood comes in contact with a substance under the endothelial cells, called collagen, which activates circulating platelets and pro-coagulant proteins. Platelets floating in the blood are attracted to collagen and move to the site of the injury.
2. The second critical step is the formation of a platelet plug. As the platelets are attracted to collagen, they stick to each other and to fibers in the blood vessels and they form a plug that temporarily blocks blood flow. This platelet plug is a temporary patch over the leak.
There are three steps to platelet plug formation; platelet adherence, activation, and aggregation.
Adherence. The endothelial cells in the vessel wall begin to secrete the von Willebrand factor. Von Willebrand Factor (VWF) is a protein that acts as a bridge and binds to the exposed collagen, serving as the site for platelets to adhere to each other and to the disrupted vessel surface (Heemskerk et al, 2002). VWF also causes the platelets to change form, growing adhesive filaments and extensions that adhere to the collagen on the endothelial wall.
Activation. After platelet adherence occurs, the sub-endothelial collagen binds to receptors on the surface membrane of the platelet, which activates them. When activated, the platelets aggregate and expose sites that coagulation factors can bind to.
Inside each platelet are storage spaces called granules. The platelet contains three types of internal granules: alpha granules, dense granules, and lysomes. The alpha granules and dense granules move to the surface of the platelet, and fuse with the platelet membrane. Each of these granules are rich in certain chemicals that have an important role in platelet function. During platelet activation, the chemicals inside the granules are pushed out into the bloodstream via a process called degranulation.
These chemicals signal other platelets to come and pile onto the clot. For example, dense granules contain large quantities of calcium ions and adenosine diphosphate ADP). ADP is a key mediator in activating platelet aggregation and clot formation. Upon release from the platelet, ADP stimulates other platelets to activate. Calcium helps provides an important surface for various coagulation factors to assemble on.
Another secretion is thromboxane, which causes platelets to change shape from spherical to stellate. The platelets undergo a morphological change by assuming an irregular surface, forming numerous pseudopods and drastically increasing their surface area (Andrews & Berndt, 2004). This provides more area for the assembly of activated coagulation factors,
The alpha granules contain many proteins, including fibrinogen, thrombospondin, fibronectin, and von Willebrand factor.
Subsequently, there is an extensive formation of procoagulant enzymes on the membrane sites provided by activated platelets, monocytes, other circulating blood cells, as well as the damaged endothelium. These enzymes allow the next step in forming a platelet plug, aggregation, to happen. Platelets, therefore, act as vehicles to concentrate and potentiate coagulation reactions on the damaged vessels.
Aggregation. The final step of platelet plug formation is the aggregation of the platelets into a barrier-like plug. Receptors on the platelets bind and hold the platelets together and anchor them to the damaged endothelium. The completed plug will cover the damaged components of the endothelium, seal the injured area, and will stop blood from flowing out of it. If the wound is large enough, blood will not coagulate until the fibrin mesh from the coagulation cascade is produced, which strengthens the platelet plug. If the wound is minor, the platelet plug may be enough to stop the bleeding without the coagulation cascade.
3. The formation of a fibrin clot is the final step in the coagulation cascade. The platelet plug temporarily stops bleeding and is a very helpful emergency response. However, a platelet plug is only a temporary fix, as it is weak. It can’t last on its own. A fibrin clot is needed. A fibrin clot is a good, strong patch over a hole in a blood vessel. It is normally enough to stop the bleeding completely.
In the final step of coagulation, thrombin is generated, which is needed to produce fibrin. The activated platelet surface helps produce a large-scale thrombin burst, leading to the conversion of fibrinogen to fibrin (Monroe et al, 1996; Hoffman et al, 1995).
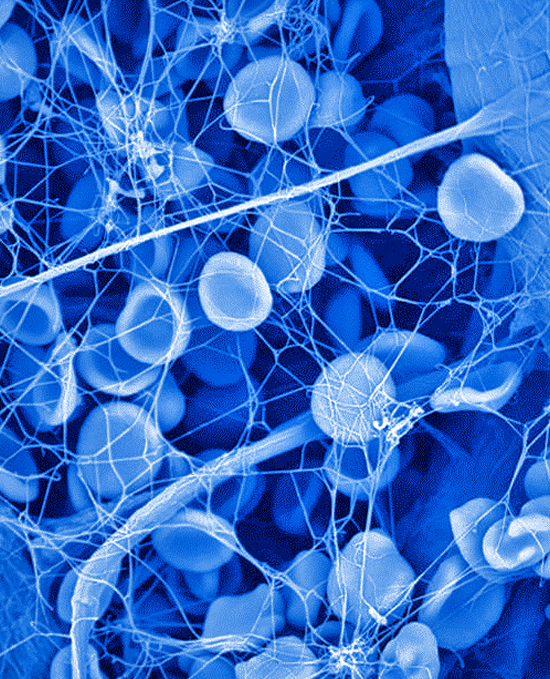
Fibrin threads wind around the platelet plug at the damaged area of the blood vessel, forming an interlocking network of fibers and a framework for the clot. This net of fibers traps and holds platelets, blood cells, and other molecules tight to the site of injury, functioning as the initial fibrin clot. This temporary fibrin clot can form in less than a minute and slows blood flow. It takes approximately sixty seconds until the first fibrin strands begin to intersperse among the wound. After several minutes, the platelet plug is completely formed by fibrin and blood loss is stemmed. This fibrin mesh is the base material for eventual healthy skin.
Think of this process as a spider web made of duct tape.
Then platelets in the clot begin to shrink, tightening the clot and drawing together the vessel walls to initiate the process of wound healing. Usually, the whole process of clot formation and tightening takes less than a half hour (Heemskerk et al, 2002; Kalafatis, et al, 1997; Davie, 2003). The result is a sturdy scab to protect the area as you heal (Hall, 2010). When it is no longer needed, the body gets rid of the fibrin clot.
Fibrinolysis is the tightly regulated system that digests already formed clots and/or prevents clots from growing. Fibrinolysis occurs simultaneously with the initiation of clot formation, limiting thrombosis to the local area of injury, and beginning the processes of clot revision, vascular damage repair, and ultimately, vessel recanalization (Davis et al, 2011). In this system, a series of blood proteins disengage the activated blood-clotting system, and begin the process to dissolve the clot.
The fibrinolytic system involves the conversion of plasminogen to plasmin. As the clot is formed, it also contains elements that will dissolve the clot. As an example, plasmin is trapped within the clot. The first key molecule in the cascade of the fibrinolytic system is plasmin, which is produced in an inactive form, plasminogen, in the liver.
Tissue plasminogen activators (TPA) are released from injured vessel walls. TPA activates plasminogen within the clot to plasmin. During fibrinolysis, plasmin degrades the fibrin mesh into small fragments. These fragments possess anticoagulant properties that inhibit thrombin and cause platelet dysfunction which inhibits aggregation (Krutsch, 2011). Plasmin also interferes with coagulation by destroying clotting factors VIII and V, from the fibrinogen group of factors.
After several days, the fibrin is dissolved, replaced by a permanent framework of scar tissue that includes collagen, the platelets subsequently degenerate into an amorphous mass, and thus, healing is complete.
Clotting Factors
The clotting factors are the group of related proteins that are in constant circulation in the blood or present in tissues of the blood vessels. At least 12 substances called clotting factors or tissue factors take part in the cascade of chemical reactions that eventually create a mesh of fibrin within the blood. They are numbered with Roman numerals (I, II, III, IV, V, VII, VIII, IX, X, XI, XII, XIII) and given a common name as well. The factors are numbered according to the order in which they were discovered and not according to the order in which they react. Each of the clotting factors has a very specific function. The clotting factors work together, with one triggering the other.
The first 4 of the 12 originally identified factors are referred to by their common names, i.e., fibrinogen (factor I), prothrombin (factor II), tissue factor (factor III), and calcium (factor IV). Clotting factor VI no longer exists. The more recently discovered clotting factors (e.g. prekallikrein and high-molecular-weight kininogen) have not been assigned Roman numerals..
Clotting factor III is also known as platelet tissue factor (TF). It is present in endothelial cells and helps initiate fibrin formation.
Calcium.
Clotting factor IV, calcium, is a co-factor for several other clotting factors such as III, VII, IX and X (Arthus & Pages, 1890; Arthus & Pages, 1891). Calcium is needed for those clotting factors to bind to membrane surfaces and to assemble together into clots. But that can only happen with the help of vitamin K. In the presence of vitamin K, those clotting factors become carboxylated, activating them. When calcium binds to carboxylated proteins it leads to a shape change that allows the protein to bind to membranes, such as the membranes of platelets and vessel walls.
Also, the calcium helps in assembling the clotting factors on the membrane surfaces of the activated blood platelets. The clotting factors are anchored to the platelet membrane surfaces through calcium bridges (Elodi & Elodi, 1983). The calcium ions essentially form a bridge between the clotting factor and the activated platelet surface. This is how the clotting process is kept localized at the original site of vessel injury.
Much of blood clotting is a result of blood-clotting proteins assembling into a complex on the membranes of platelets and endothelial cells; within these complexes, the factors can efficiently contact one another to become activated and participate in clot formation, as in the clotting cascade. These clotting factors together activate prothrombin to produce thrombin, which is central to coagulation. The thrombin then produces fibrin to fibrinogen, which produces the strongest clot. Calcium acts as a catalyst for this reaction.
Without carboxylation, these bridges will not form, and the adherence of the clotting factors to the injured cell walls does not take place. When levels of vitamin K are low, blood will take longer to clot. If calcium levels are also deficient, you may bleed to death.
Calcium is so important that the body precisely controls the amount of calcium in cells and blood. The body moves calcium out of bones and into the blood as needed, to maintain a steady level of calcium in the blood. If people do not consume enough calcium from their diet, then too much calcium is mobilized from the bones, weakening them. Osteoporosis can result (Doolittle, 2016). Most people gain enough calcium from their diets and taking a calcium supplement is not recommended.
Clotting factors can also be classified into three groups; the Fibrinogen Family, the Contact family, and Vitamin K dependent proteins family.
1.Fibrinogen Family:
Fibrinogen is clotting Factor 1. During a vascular injury thrombin converts fibrinogen to fibrin and subsequently to a fibrin-based blood clot.
Factor V is a protein made in the liver. When Factor V is activated it interacts with coagulation factor X. Together they form a complex that converts helps convert fibrinogen into fibrin.
Factor VIII is an essential blood clotting protein, also known as anti-hemophilic factor (AHF).
Factor XIII is an enzyme that crosslinks fibrin. A deficiency affects clot stability. This factors causes clots to dissolve slowly and carefully.
2.Contact Family: one of two major pathways for triggering the clotting cascade
Factor Xi or plasma thromboplastin is a form of factor XIa, one of the enzymes of the coagulation cascade.
Factor XII is also known as Hageman factor, is a protein that seems to be involved in later stages of clot formation (Renne, et al 2005).
Hmwk is one of four proteins which initiate the contact activation pathway (also called the intrinsic pathway) of coagulation. The other three are factor Xii, Xi, and prekallikrein.
Prekallikrein (PK) also known as the Fletcher Factor, participates in the surface-dependent activation of blood coagulation and fibrinolysis.
3.Vitamin K Dependent clotting proteins:
Vitamin K was originally identified for its role in the process of blood clot formation, though we know it is involved in much more than coagulation. The letter K was derived from the German word "koagulation". As with the anti-coagulant proteins, Vitamin K is a necessary cofactor for the critical clotting proteins.
With the presence of vitamin K, these clotting proteins become carboxylated. Amino acids are the building blocks of proteins. In this carboxylation process, the amino acid Glu, is converted into gamma-carboxyglutamate acid or Gla. Gla makes it possible for the protein to bind metals such as calcium. The presence of Gla residues in the vitamin K dependent clotting factors are essential for their function in the clotting process (Suttie, 1993; Monroe, 2010).
These Gla residues enable the protein to bind to membrane surfaces. Glu is a weak calcium chelator and Gla is a much stronger one, so the carboxylation of the protein substantially increases the calcium binding capacity of the protein (Esmon et al, 1975a; Nowak & Grzubowska-Chelbowczyk, 2014; Shearer, 1995). When the Gla domain binds calcium, it undergoes an important shape change, and is transformed from a random coil to an ordered structure. The Gla residues orient inward and together with calcium ions, form the interior core, and expose a binding site. Without the calcium, the shape change would not happen, and the binding site of the protein would not be exposed which is an important part of the clotting process (Stenflo, 1999; Nelsestuen et al, 2000; Soriano-Garcia et al, 1992).
Calcium binding by the Gla residues is also essential for activating and anchoring circulating blood clotting factors at the site of injury. The Gla domain directly binds to cell membrane surfaces through calcium ion bridges (Furie & Furie, 1992; Freedman et al, 1995; Freedman et al, 1996; Berkner & Runge, 2004; Kalafatis et al, 1994). The presence of calcium is required for the vitamin K dependent clotting factors, such as prothrombin to be activated and trigger the clotting process to form the enzyme thrombin (Rawala-Sheikh et al, 1992).
An essential element in the success of coagulation cascade is the assembly of the various clotting complexes in an orderly fashion on the surface of the platelets and endothelial cells. Within these complexes, the factors can efficiently contact one another to become activated and participate in clot formation. The GLA domains provide the critical link, localizing the clotting factors to the platelet surface (Magnusson et al, 1974).
The vitamin K dependent clotting factors are Factor II, VII, IX, and X. (Stenfloet al, 1934; Nelsestuen et al, 1974; Magnusson et al, 1974; Zytkovicz et al, 1975; Vermeer et al, 1978; Olson, 1984). These four coagulation proteins need to be carboxylated or activated in order to become biologically functional. These proteins have in common the requirement to be post-translationally modified by carboxylation of glutamic acid residues, forming Gla, in order to become biologically active. Vitamin K enables those clotting factors to clot the blood quickly (Askim, 2001; Bern, 2004; Theuwissen et al, 2012; Shearer & Newman, 2008).
Factor II is also known as Prothrombin. Prothrombin, has 10 glutamic acids in the amino-terminal region of the protein which can be carboxylated. Without vitamin K, the carboxylation does not occur and the proteins that are synthesized are biologically inactive.
The precursor of prothrombin binds less than 1 mol of calcium per mole of protein. When it is carboxylated, each mole of the prothrombin protein can bind 10 to 12 mol of calcium. (Berdanier, Advanced Nutrition Micronutrients).
Activated prothrombin forms thrombin. Thrombin converts fibrinogen to fibrin, the insoluble protein that solidifies the blood clot. As well, thrombin is the most important platelet activator, and it activates other clotting factors, Factors VIII and V, and it activates Factor XIII, which crosslinks the fibrin.
Prothrombin time (PT) is a blood test that measures how long it takes for blood to clot. It may also be referred to as an INR test (International Normalized Ratio), which was developed as a way to standardize the various testing methods for prothrombin, so as to produce results that could be compared.
Factor VII (Proconvertin). When cells are damaged, they increase a protein on their surface called tissue factor, or TF. The tissue factor needs to bind to factor VII in the clotting cascade. Factor VII cannot be bound until it is activated with the assistance of vitamin K.
Acquired Factor VII deficiency is the most common reason for prolonged prothrombin time (clotting time). Warfarin use, vitamin K deficiency, and liver disease are the main causes of acquired factor VII deficiency.
Factor IX converts Factor X to its active form in the presence of calcium ions, phospholipids and factor VIIIa. A deficiency of factor IX causes a type of hemophilia called Christmas disease (Biggs et al 1952). Clotting times can be severely, moderately or mildly decreased with this deficiency.
Factor X is the first enzyme in the common pathway of thrombus formation. It is activated on the surface of blood platelets with the help of tissue factor, calcium and vitamin K. Once the enzyme is activated it becomes factor Xa, which is responsible for the conversion of prothrombin to thrombin within your clotting cascade.
An adequate balance between the pro-and anti-coagulant systems is a prerequisite for the prevention of bleeding and/or clotting (Esmon, 1989; Stenflo, 1948). Fortunately, vitamin K seems to activate the pro-coagulation parts of the pathway simultaneously and proportionately to its activation of the anti-coagulation branches, and most people maintain fairly normal clotting levels across a wide range of vitamin K status (Matsuzaka et al, 1993).
Vitamin K is a necessary component in the coagulant system. However, vitamin K is also a bystander. The coagulant system is not triggered not is it resolved by vitamin K. The coagulation system is triggered by injury, trauma, disease, etc. It is not triggered by the presence of vitamin K. However, vitamin K is a key factor in the effectiveness of the coagulant system. When the availability of vitamin K is low, the carboxylation of the clotting factors is insufficient, and fewer of them are active.
WHAT HAPPENS IN THE ABSENCE OF VITAMIN K
In the absence of vitamin K, the clotting factors are not carboxylated. If the Gla-domain of a vitamin K-dependent coagulation factor is not carboxylated or modified, the protein loses its capacity to bind to membrane surfaces and thus is no longer able to participate in coagulation reactions. Clot formation is compromised. Lack of these Gla residues results in impaired coagulation or even anticoagulation, which may lead to thrombosis (Kalafatis et al, 1996)
As an example, the medication warfarin, (aka Coumadin) interferes with the formation of Gla, meaning the clotting factor prothrombin (Factor II) cannot bind to calcium, making it inactive and unable to produce thrombin to start the clot (Stenflo et al, 1974; Friedman & Przyiecki, 1986). A deficiency in circulating, carboxylated prothrombin decreases the amount of thrombin available for coagulation and increases the body's tendency to hemorrhage following a blow or injury. Interfering with Gla formation is the mechanism by which warfarin keeps clots from forming, but which also leads to a functional deficiency of vitamin K in the body.
In states of vitamin K deficiency, under-carboxylated species of the vitamin K-dependent coagulation proteins are released from the liver into the blood; their levels increase with the degree of severity of vitamin K deficiency. These uncarboxylated proteins are unable to participate in the normal coagulation cascade because they are unable to bind calcium, and they do not interact with biological membranes (Aoki, Ohdama, Kirokawa, ).
These under-carboxylated forms are referred to as PIVKA - Proteins Induced by Vitamin K Absence (aka des-carboxy-prothrombin). The measurement of under-carboxylated prothrombin (PIVKA-II) is the most useful and sensitive homeostatic marker of sub-clinical vitamin K deficiency. Importantly, PIVKA-II is detectable in plasma before any changes occur in conventional coagulation tests. Several types of assays for PIVKA-II have been developed, such as the K-1 test and the uncarboxylated osteocalcin test (Widdershoven et al, 1987).
RESEARCH EXAMPLES
Vitamin K is key for both coagulation and anti-coagulation. Vitamin K is necessary to carboxylate the clotting proteins so they are active and clot appropriately. Vitamin K is also necessary to activate the anti-coagulation proteins.
Low amounts of vitamin K can impact clotting efficacy, and also promote unnecessary clotting due to deficiencies in the anti-coagulant system. High amounts of vitamin K ensures the efficacy of both systems, only. Having sufficient vitamin K ensures that the proteins are activated.
There is no documented case of toxicity for phylloquinone or menaquinones, regardless of dosage intake (National Research Council, 2011; Bresson et al, 2008). And the FDA has not identified any upper limit in vitamin K doses, as there have been no reports of toxicity (Commission Directive 2008/100/EC).
Research has been done to show that high amounts of vitamin K do not result in over-clotting.
Animal Studies
An animal study conducted with rats showed no toxicity with high doses of vitamin K. In the study, the rats were put on a vitamin K deprived diet, and their circulating prothrombin levels were measured. The rats were given single doses of 0, 2.5 mg/kg, or 10 mg/per kg of body weight per day for 90 days. In human terms, this amounted to a median lethal dose of greater than 2000 mg/kg of body weight. Even at this level, there were no signs of systemic toxicity or abnormalities in neurological functioning, and no adverse effects were found (Pucaj et al, 2011) .
Another animal study showed that thrombosis risk was not increased when given doses of MK4, up to 250 mg/kg of body weight (Ronden et al, 1997).
Human Studies
A study of elderly patients with osteoporosis were given 45 mg/day three times day, after meals for 12 weeks. The clotting parameters remained stable, indicating that MK4 can be administered safely (Asakura, et al, 2001). In human subjects, a study was conducted to examine whether vitamin K supplementation improves bioactivity in patients on dialysis. The subjects were given doses of 45, 135, or 360 micrograms a day for six weeks. The risk of clots or thrombosis was evaluated by the endogenous thrombin potential, which is the most sensitive marker to evaluate thrombosis risk in plasma. Clotting risk was not affected by MK-7 intakes as high as 360 mcg a day for 6 weeks (Westenfeld, Krueger, et al 2012).
Theuwissen and her group expressly studied the question of whether very high vitamin K intake could lead to increased clotting risk. Since the key role of vitamin K in regulating haemostasis is generally known, an obvious question is whether increased vitamin K intake may lead to increased clotting tendency. They gave MK7 to healthy subjects and studied their thrombin generation. They gave them daily doses of 10, 20, 45, 90, 180 or 360 ug. for 12 weeks. Their results showed that while circulating osteocalcin and matrix Gla protein were increasingly carboxylated, there were no adverse effects on thrombin generation and no effect on the blood coagulation system in general, such as a change in prothrombin time. There was no evidence of vitamin K-induced hypercoagulability in healthy subjects (Theuwissen, Cranenburg et al, 2012).
There have been published accounts of super high intakes of vitamin K, with no toxic effect. A 39 year old male deliberately ingested a superwarfarin product. To counteract the dose, he was given 200 milligrams a day of vitamin K1 for five months without any adverse effects (Sheen et al, 1994).
In 2003, a young man was brought to the emergency room after eating four boxes of brodifacoum, a lethal vitamin K antagonist, over four days, plus pieces of glass. He was treated for both the glass and the poisoning, for which they gave him 300 milligrams of vitamin K1 a day. 28 days after discharge he returned, as he had not maintained the vitamin K1 intake. During the second treatment, his vitamin K1 dosage was increased to 800 milligrams a day. At a five month follow-up he was doing well.
Recently, an article was published discussing the differential diagnosis of rat poisoning and treatment in two separate cases. In one case the patient had taken a long-acting rat poison. He was given 75 milligrams of vitamin K1, twice a day for over four months so as to stabilize his coagulation system and restore it to relative normality. In the second case, a woman was treated with 100 milligrams of vitamin K daily for 2 days, which restored her coagulation function. In a general discussion of treatment options, it was recommended to administer vitamin K at doses of 50 milligrams a day or higher intravenously, and then shifting to oral doses of 100 milligrams a day, for three to six months, and sometimes for more than a year (Schulman & Furie, 2014). The highest reported dose has been 400 milligrams daily (Spahr et al, 2007).
Summary
This page clarified the primary elements of the circulatory system and its ability to keep blood flowing freely, and the coagulation system, which ensures that the blood will quickly clot if needed. Vitamin K is a required component for both systems to function effectively.
Many folks are concerned that taking vitamin K will trigger coagulation, as if high doses of vitamin K would lead to high frequencies of blood clotting. This is an impossibility, as vitamin K does not start the clotting process, it only enables the coagulation system to function effectively. When the coagulation cascade begins, vitamin K levels ensure that the system will clot your blood quickly and effectively. High levels of vitamin K only ensure the coagulation system has what it needs. Low levels of vitamin K create a risk that coagulation would be impaired. Additionally, research and case studies have shown that folks can tolerate massive doses of vitamin K, with no toxicity or disruption in the coagulation system.
Another misconception seems to be that taking vitamin K will somehow ‘thicken’ the blood, rendering it less fluid and functional throughout the body. This also is not possible as the coagulation system localizes the clot formation. Endothelial cells only at the site of the injury release the protein, tissue factor, which activate and attract platelets to that location. The clotting factors form only at that location on both the platelets and the vessel wall. The entire vascular system does not attract clot formation. In fact, if you remember the anti-coagulation system, the endothelial cells in the tissue wall are constantly expressing anti-coagulant proteins, such as Protein C, and thrombomodulin, which terminates clot expansion and localizes clotting in a dose-dependent manner (Walker & Fay, 1992; Dorffler-Melly et al, 2003; Panteleev et al, 2006).
Less well known is the fact that vitamin K is also a key element in the circulatory system, as well as in the coagulation system. Sufficient amounts of vitamin K are required to ensure that the blood flows freely. Actually, the risk of unnecessary clots is increased when there are low amounts of vitamin K. Without sufficient vitamin K present in the body, the anti-clotting proteins are not active and are impaired.
So vitamin K cannot ‘over-clot’ your blood and is an essential element for your blood to flow freely throughout your body.
REFERENCES
Arthus M, Pages C. Nouvelle theorie chimique de la coagulation du sang. Arch de Physiol. 1890:739-746.
They found that calcium was essential for coagulation.
Arthus M, Pages C. Theorie chimique de la coagulation du sang. Ac Sci C B. 1891;112:241-244.
Biggs R, Douglas AS, MacFarlane RG, Dacie JV, Pitney WR, et al. Christmas disease: A condition previously mistaken for haemophilia. Br Med J. 1952 Dec 27;2(4799):1378-82.
An important evolution, as the research sorted out the consequences of impaired clotting factors and delineated the diseases accurately.
1970
Magnusson S, Sottrup-Jensen L, Petersen TB, Morris HR, Dell A. Primary structure of the vitamin K-dependent part of prothrombin. FEBS Lett. 1974 Aug 25;44(2):189-93.
Determined that the role of vitamin K in blood coagulation was to cause the modification of glutamic acid residues into Gla, and make them calcium binding.
Nelsestuen GL, Zytkowicz TH, Howard JB. The mode of action of vitamin K. Identification of gamma-carboxyglutamic acid as a component of prothrombin. J Biol Chem. 1974;294:6347-6350.
Stenflo J, Fernlund P, Egan W. Vitamin K dependent modifications of glutamic acid residues in prothrombin. Proc Natl Acad Sci USA. 1974;71:2730-2733.
Their study concluded that it was the Gla residues in carboxylated vitamin K proteins that bound up calcium, and that the process took place in the vitamin K-dependent clotting factors.
Zytkowicz TH, Nelsestuen GL. [3H] diboane reduction of vitamin K-dependent calcium-binding proteins. Identification of a unique amino acid. J Biol Chem. 1975 Apr 25;250(8):2968-72.
This study concluded on a method to identify proteins which are vitamin K-dependent.
Nelsestuen GL, Broderius M, Martin G. Role of gamma-carboxyglutamic acid. Cation specificity of prothrombin and factor X-phospholipid binding. J Biol Chem. 1976;251(22):6886-93.
Kisiel, W., Canfield, W.M., Ericsson, L.H. & Davie, E.W. (1977) Anticoagulant properties of bovine plasma protein C following activation by thrombin. Biochemistry. 1977;16:5824-5831.
Stenflo, J. (1976) A new vitamin K-dependent protein. Purification from bovine plasma and preliminary characterization. J. Biol. Chem., 251, 355-363.
This study was introducing what would be referred to as Protein C.
Di Scipio RG, Hermodson MA, Yates SG, Davie EW. A comparison of human prothrombin, factor IX (Christmas factor), factor X (Stuart factor), and protein S. Biochemistry 1977;16:698–706.
Stenflo J, Suttie JW. Vitamin K-dependent formation of gamma-carboxyglutamic acid. Ann Rev Biochem. 1977;46-157-72.
Vermeer C, Govers-Riemslag JW, Soute BA, Lindhout MJ, Kop J, Hemker HC. The role of blood clotting factor V in the conversion of prothrombin and a decarboxy, prothrombin into thrombin. Biochim Biophys Acta. 1978 Feb 1;538(3):521-33.
1980
Lindahl U, Backstrom G, Thunberg I, Leder IG. Evidence for a 3-O-sulfated D-glucosamine residue in the antithrombin-binding sequence of heparin. Proc Natl Acad Sci USA. 1980;77:6551-55.
Griffin JH, Evatt B, Zimmerman TS, Kleiss AJ, Wideman C. Deficiency of protein C in congenital thrombotic disease. J Clin Invest. 1981 Nov;68(5):1370-3.
Casu B, Oreste P, Torri G, Zoppetti G, Choay J, Lormeau JC, Petitou M, et al. The structure of heparin oligosaccharide fragments with high anti-(factor Xa) activity containing the minimal antithrombin III-binding sequence. Chemical and 13 C nuclear-magnetic-resonance studies. Biochem J. 1981;197:599-609.
Bertina RM, Broekmans AW, van der Linden IK, Mertens K. Protein C deficiency in a Dutch family with thrombotic disease. Thromb Haemost. 1982 Aug 24;48(1):1-5.
Marlar, R.A., Kleiss, A.J. & Griffin, J.H. Mechanism of action of human activated protein C, a thrombin-dependent anticoagulant enzyme. Blood. 1982;59:1067- 1072
This study concluded that the active form of protein C may serve as a major regulator of cofactors of coagulation.
Elodi S, Elodi P. Surface-governed molecular regulation of blood coagulation. Mol Aspects Med. 1983;6(4):291-353.
This study discusses the spatial control of blood clotting. Under physiological circumstances a clot is formed only in the vicinity of injury. The consecutive actions of coagulation are confined to the surface produced by the injury. The reactions taking place on the surface form an enzyme cascade, which amplifies the relatively weak triggering signal by several orders of magnitudes.
Nelsestuen GL. Calcium involvement in the protein-membrane systems of blood coagulation, Inorganic Chimica Acta. 1983;79:41.
This article discusses calcium, which functions to aid binding of vitamin K-dependent proteins to membranes. This calcium binding to Gla causes a protein conformational change which is a prerequisite to protein-membrane binding. Calcium also serves a second role as a bridge between ligands of the protein and the membrane surface.
Bertina RM, Broekmans AW, Krommenhoek-van Es C, van Wijngaarden A. The use of a functional and immunologic assay for plasma protein C in the study of the heterogeneity of congenital protein C deficiency. Thromb Haemost. 1984 Feb 28;51(1):1-5.
Comp, P. C, Nixon RR, Cooper MR, Esmon CT. Familial protein S deficiency is associated with recurrent thrombosis. J Clin Invest. 1984;74:2082.
Esmon CT. Protein C. Prog Hemost Thromb. 1984;7:25-54.
The protein C anticoagulant pathway provides many new insights into control mechanisms for regulating coagulation, and is a major regulatory pathway. The complexity of the system has only recently begun to emerge. Once activated, protein C has an almost total dependence on protein S to express anticoagulant activity. This suggests that deficiencies of protein S may also be associated with thrombotic tendencies. Protein S offers an additional intriguing property. They discuss the fundamental mechanisms involved in regulating blood coagulation.
Marcum JA, Rosenberg RD. Anticoagulantly active heparin-like molecules from vascular tissue. Biochemistry. 1984;23:1730-37.
Olson RE, The function and metabolism of vitamin K. Annu Rev Nutr. 1984;4:281-337.
Since the discovery of gamma-carboxyglutamic acid a decade ago, great progress has been made in advancing our knowledge of the function and metabolism of vitamin K. The distribution of this new amino acid in proteins and the presence of the vitamin K-dependent carboxylase in diverse tissues have emphasized the widespread significance in biology of a new triad: vitamin K, Gla, and calcium. Since this enzyme is an intrinsic membrane-bound protein, the scientific attack on its structure and function is at one of the present frontiers of molecular biology.
Philips M, Juul AG, Thorsen S. Human endothelial cells produce a plasminogen activator inhibitor and a tissue-type plasminogen activator-inhibitor complex. Biochim Biuophys Acta. 1984;802:99-110.
Stenflo J. Structure and function of protein C. Semin Thromb Hemost. 1984 Apr;10(2):109-21.
Vigano S, Mannucci PM, Solinas S, Bottasso B,. Mariani G. Decrease in protein C antigen and formation of an abnormal protein soon after starting oral anticoagulant therapy. Brit J Haemat. 1984;57:213-220.
Bertina RM. Hereditary protein S deficiency. Haemostasis. 1985;15:241.
Protein S is a vitamin K-dependent plasma protein that serves as a cofactor of activated protein C(APC) in its inhibitory action on clotting factor V and factor VIII and in its stimulation of fibrinolytic activity. Patients with a protein S deficiency were found to be at risk for the development of venous thrombotic disease at a relatively young age.
Stern DM, Nawroth PP, Kisiel W, Vehar G, Esmon CT. The binding of factor IXa to cultured bovine aortic endothelial cells. Induction of a specific site in the presence of factors VIII and X. J Biol Chem. 1985;260:6717-6722.
Sakata Y, Curriden S, Lawrence D, Griffin JH, Loskutoff DJ. (1985) Activated protein C stimulates the fibrinolytic activity of cultured endothelial cells and decreases antiactivator activity. Proc. Nat. Acad. Sci. USA, 1985;82:1121-1125.
This study looked at the role of activated protein C on increased fibrinolytic activity (dissolving clots).
Stern E, Nawroth P, Handley D, Kisiel W. An endothelial cell-dependent pathway of coagulation. Proc Natl Acad Sci USA. 1985;82:2523-27.
This study looked at the role of the endothelial cells in coagulation. This endothelial cell-dependent pathway suggests a central role for factors VIII and IX consistent with their importance in clotting.
Tollefesen, DM, Pestka CA. Heparin cofactor II activity in patients with disseminated intravascular coagulation and hepatic failure. Blood. 1985;66:769-74.
van Hinsbergh VWM, Bertina, RM, van Wijngaarden A, van Tiburg, NH, Emeis, JJ, Haverkate F. Activated protein C decreases plasminogen activator inhibitor activity in endothelial cell-conditioned medium. Blood. 1985;65:444-451.
Cultures of endothelial cells from human umbilical cord were used to study the effect of activated human protein on the production of plasminogen activators, inhibitors and factor VIII-related antigen. The data suggested that activation of the coagulation system may lead to a secondary increase of the fibrinolytic activity by changing the balance between plasminogen activators and inhibitors.
Fair DS, Marlar RA, Levin EG. Human endothelial cells synthesize protein S. Blood. 1986;67:1168-1171.
The production of protein S by endothelial cells supports the hypothesis that cofactor production and expression by the endothelial cells play a significant regulatory role in the initiation, propagation, and suppression of hemostasis and thrombosis.
Friedman PA, Przyiecki CT. Vitamin K-dependent carboxylation. Int J Biochem. 1987;19(1):1-7.
This article reviews what was currently known at the time about vitamin K and the carboxylation reaction.
Shuman MA. Thrombin-cellular interactions. Ann NY Acad Sci. 1986;485:228-39.
Takahashi H, Hanano M, Hayashi S, Arai Y, Yoshino N, Takakuwa E. Plasma levels of protein C and vitamin K-dependent coagulation factor in patients on long-term oral anticoagulant therapy. Tohoku J Exp Med. 1986 Aug;149(4):351-7.
These findings indicate that long-term oral anticoagulant therapy results in the suppression of the synthesis of both vitamin K-dependent coagulation factors and Protein C, but the production of the coagulant and anticoagulant proteins is well-balanced.
Esmon CT. The regulation of natural anticoagulant pathways. Science. 1987;235:1348-52.
This study looked at the role of the vascular endothelium in preventing blood clot formation, and concluded that the protein C pathway was key. They also considered that this pathway provides a link between inflammation and coagulation.
Esmon CT, Viagno-D’Angelo S, D’Angelo A, Comp PC. Coagulation proteins C and S. Adv Exp Med Biol. 1987;214:47-54.
Proteins C and S are two vitamin K-dependent plasma proteins that work in concert as a natural anticoagulant system. The anticoagulant activity is expressed through the selective inactivation of Factors Va and VIIIa. Multiple mechanisms and/or drugs can lead to acquired deficiencies of these proteins: oral anticoagulation, liver disease, DIC and in the case of protein S, lupus erythematosus, nephrotic syndrome, pregnancy and certain hormones. The anticoagulant activity of protein C decreases rapidly after administration of warfarin. Protein S antigen levels do not decrease as rapidly, but protein S functional levels are often low in patients with an acute thrombus. The available information all suggest that deficiency of protein C and protein S should be considered a risk factor contributing to recurrent thrombotic disease and that the function of these proteins is altered by many common clinical conditions which have associated an increased risk of thrombosis.
Widdershoven J, van Munster P, De Arbreu R, Bosman H, van Lith T, van der Putten-van Meyel M, et al. Methods compared for measuring des-carboxy-prothrombin (PIVKA-II). l Clin Chem. 1987 Nov;33(11):2074-8.
PIVKA-II (Protein Induced by Vitamin K Absence) is abnormal des-carboxylated prothrombin, which is present in vitamin K deficiency or in patients using warfarin. With a sensitive method for PIVKA-II, biochemical vitamin K deficiency can be established before clinical symptoms occur.
Furie B, Furie BC. The molecular basis of blood coagulation. Cell. 1988 May 20;53(4):505-18.
The blood coagulation cascade is an intricately complex web of positive and negative feedback loops finely tuned to ensure hemostasis without spontaneous hemorrhage or thrombosis. This study focuses on the molecular basis of blood coagulation with particular attention to the biochemistry and regulation of this pathway as it relates to humans in health and disease.
Esmon, CT. The roles of protein C and thrombomodulin in the regulation of blood coagulation. J Biol Chem. 1989;264:4743-46.
1990
Lobato-Mendizabal E, Ruiz-Arguelles GJ. Protein C, protein S and thrombomodulin: one of the new antithrombotic mechanisms. Rev Invest Clin. 1990 Jan-Mar;42(1):54-62.
In this review paper, the salient features of the anticoagulant/fibrinolytic mechanism depending on coagulation protein C, protein S and thrombomodulin are reviewed. Coagulation protein C, activated at the endothelial cell surface exerts two anti-thrombotic effects: one anticoagulant dependent on the free protein S and the other pro-fibrinolytic, independent of protein S. Both inherited and acquired deficiencies of protein C and/or protein S lead to a thrombosis-prone state that has to be identified promptly to avoid vaso-occlusive episodes.
Vermeer C. Gamma-carboxyglutamate-containing proteins and the vitamin K dependent carboxylase. Biochem J. 1990 Mar 15;266(3):625-36.
A discussion of the rapid developments in the vitamin K field. They felt it was plausible that the administration of vitamin K or vitamin K antagonists may form additional tools to prevent or to cure diseases related to an incorrect functioning of these vitamin K-dependent proteins.
Dow P, Ham SW, Geib SJ. Mechanism of action of vitamin K. J Am Chem Soc. 1991;113(20):7734-43.
Mikaelsson, M.E. 1991. The role of calcium in coagulation and anticoagulation. In Sibinga CTS, Das PC, Mannucci PM. Coagulation and blood transfusion. Developments in hematology and immunology. Boston: Springer. p. 29–37.
Furie B, Furie BC. Molecular and cellular biology of blood coagulation. N Engl J Med 1992; 326: 800–6.
Regulation of coagulation by antithrombin 3, proteins C and S, and the biochemical role of vitamin K are described. Evolving knowledge of the molecular biology of the coagulation enzymes and regulatory proteins is presented as well as the molecular pathology of hemophila. New monitoring assays for coagulation are presented.
Rawala-Sheikh R, Ahmad SS, Monroe DM, Roberts HR, Walsh PN. Role of gamma-carboxyglutamic acid residues in the binding of factor IXa to platelets and in factor-X activation. Blood. 1992;79(2):398-405.
Soriano-Garcia M, Padmanabhan K, de Vox AM, Tulinksy A. The calcium ion and membrane binding structure of the Gla domain of calcium-prothrombin fragment 1. Biochemistry. 1992;31:2554-2566.
Walker FJ, Fay PJ. Regulation of blood coagulation by the protein C system. FASEB J. 1992;6:2561-67.
Structural features of both activated protein C and its substrates (coagulation factors V and VIII) are such that they require the localization of enzyme and substrate on the surface of membranes for optimum activity.
Mann KG, Lorand L. Introduction: blood coagulation. Methods Enzymol. 1993; 222: 1–10.
Matsuzaka T, Tanaka H, Fukuda M, Aoki M, Tsuji Y, Kondoh H. Relationship between vitamin K dependent coagulation factors and anti-coagulants (protein C and protein S) in neonatal vitamin K deficiency. Arch Dis Child. 1993;68:297-302.
They studied newborn babies and their findings suggest that carboxylation of coagulation factors and proteins C and S, acts to maintain both coagulation and anticoagulation activities in parallel.
More I, Sim R, Hudson M, Dhillon AP, Pounder R, Wakefield AJ. Immunohistochemical study of tissue factor expression in normal intestine and idiopathic inflammatory bowel disease. J. Clin Pathol. 1993;46:703-08.
Suttie JW. Synthesis of vitamin K-dependent proteins. FASEB J. 1993 Mar;7(5):445-52.
Kalafatis M, Swords NA, Rand MD, Mann KG. Membrane-dependent reactions in blood coagulation: role of the vitamin K-dependent enzyme complexes. Biochim Biophys Acta. 1994;1227:13-129.
Sheen SR, Spiller HA, Grossman D. Symptomatic brodifacoum ingestion requiring high-dose phytonadione therapy. Vet Hum Toxicol. 1994 Jun;36(3):216-7.
This study reports the deliberate ingestion of a superwarfarin product, brodifacoum, in a 39 year-old male. He presented with prothrombin and partial thromboplastin times of 150 and 113 sec, respectively. His coagulopathy was corrected by administration of blood products and phytonadione (manmade form of vitamin K). To maintain normal clotting studies this patient required the highest maintenance dose of phytonadione, 200 milligrams/day reported to date. The patient was able to tolerate this dose for 5 months without adverse effects.
Shearer MJ. Vitamin K. Lancet. 1995;345:229-234.
Broze GJ, Jr. Tissue factor pathway inhibitor. Thromb Haemost. 1995;74:90-93.
Discusses the understanding that tissue factor is responsible for the initiation of coagulation, but sustained clotting requires persistent and amplified procoagulant action of clotting factors VIII, IX, and XI.
Davie EW. Biochemical and molecular aspects of the coagulation cascade. Thromb Haemost. 1995;74:1–6.
Freedman SJ, Furie BC, Furie B, Baleja JD. Structure of the Calcium Ion-Bound Gamma-Carboxyglutamic Acid-Rich Domain of Factor IX. Biochem. 1995;34(8):12126-37.
This study determined the calcium bound structure of clotting factor IX, including the location of the nine Gla residues, the folding, and the possible location of the internal calcium binding pocket.
Hoffman M, Monroe DM, Oliver JA, Roberts HR. Factors IXa and Xa play distinct roles in tissue factor-dependent initiation of coagulation. Blood. 1995;86:1794–1801.
The article discusses the role of tissue factor as a major initiator of coagulation and the roles of clotting factors IXa and Xa. When activated, Xa is to activate platelets by generating a small amount of thrombin. IXa, on the other hand, enhances thrombin to the platelet surface. These factors play distinct roles, leading to an explosion of thrombin generation.
Groenen-van Dooren MM, Ronden JE, Soute BA, Vermeer C. Bioavailability of phylloquinone and menaquinones after oral and colorectal administration in vitamin K-deficient rats. Biochem Pharmacol. 1995 Sep 7;7;50(6):797-801.
Rats were made vitamin K-deficient by feeding them a diet devoid of vitamin K and by rigorously preventing coprophagy. After one week, circulating prothrombin concentrations were between 5 and 10% of initial values, and various amounts of phylloquinone, menaquinone-4, and menaquinone-9 were given in a single dose either subcutaneously, orally, or colorectally. The relative 'vitamin K activities' of these compounds were assessed by comparing their ability to support prothrombin synthesis after subcutaneous injection. Colonic absorption of all three forms of vitamin K was extremely poor, suggesting that physiological menaquinones in the colon do not contribute substantially to vitamin K status in rats.
Kalafatis M, Egan J O, van't Veer C, Mann KG. Regulation and regulatory role of gamma-carboxyglutamic acid containing clotting factors. Critical Reviews in Eukaryotic Gene Expression. 1996;l6(1):87–101.
Blood coagulation is initiated following damage of the vessel wall. The large number of proteins that participate in the reactions that regulate blood coagulation must behave in a concerted manner to generate alpha-thrombin. Following mechanical injury to the vessel wall, a cell-associated protein, tissue factor, is exposed and initiates a series of enzymatic reactions localized on a membrane surface generally provided by cells and accumulating platelets. The binding of the enzymes and zymogen substrates to the exposed membrane surface and their activation are in part governed by the gamma-carboxyglutamic acid residues (gla) of each protein. Absence of gamma-carboxylation of one or more of the critical glutamic acid residues results in an impaired coagulation/anticoagulation process which may lead to a bleeding diathesis or thrombosis.
Liu L, Rodgers GM. Characterization of an inducible endothelial cell prothrombin activator. Blood. 1996;88:2989-94.
Monroe DM, Hoffman M, Roberts HR. Transmission of a procoagulant signal from tissue factor-bearing cells to platelets. Blood Coag Fibrinol. 1996;7:459–464.
The goal of the current study was to examine the mechanism by which factor VIIa/tissue factor (TF) activity leads to platelet activation as the first step in initiation of coagulation. We conclude that sufficient thrombin generation occurs on the TF-bearing cell (or TF-bearing vesicle) in the absence of platelets, to provide the procoagulant signal that leads to platelet activation. The activated platelet surface then provides sites for TF-activated factor IXa to recruit factor Xa to bind and assemble into functional Xase and IIase complexes.
Seyama Y, Horiuch M, Hayashi M, Kanke Y. Effect of vitamin K2 on experimental calcinosis induced by vitamin D2 in rat soft tissue. Int J Vitam Nutr Res. 1996;66(1):36-8. The effect of vitamin K2 on calcium (Ca) and inorganic phosphorus (P) levels in the aorta and kidney obtained from experimental calcinosis induced by vitamin D2 of male rats was investigated. A high dose of vitamin K2 (100 mg/kg body weight) inhibited the increase in the aorta and kidney, and a low dose of vitamin K2 (10 mg/kg body weight) showed the same tendency, but the degree of the efficacy was small. It appeared that a high dose of vitamin K2 suppressed experimental calcification of soft tissues induced by vitamin D2. Therefore, a pharmacological dose of vitamin K2 might have a usefulness for the prevention and treatment of arteriosclerosis with calcification.
Celi A, Lorenzet R, Furie B, Furie BC. Platelet-leukocyte-endothelial cell interaction on the blood vessel wall. Semin Hematol. 1997;34:327-35.
Interaction of these cell adhesion molecules serves to recruit circulating cells to the blood vessel endothelium or to accumulated platelets on the vessel wall and to foster cell-cell communication.
Crowther MA, Donovan D, Harrison L, McGinnis J, Ginsberg J. Low-dose oral vitamin K reliably reverses over-anticoagulation due to warfarin. Thromb Haemost. 1998 Jun;79(6):1116-8.
Patients receiving long-term warfarin frequently develop asymptomatic excessive prolongation of their international normalized ratio (INR) results. This prospective cohort study was designed to address whether 1 mg of oral vitamin K effectively reduces the INR value of such patients. 62 patients receiving warfarin were given 1 milligram of oral vitamin K. Results showed that the vitamin K reliably reduced the INR to the therapeutic range within 24 hours. The therapy was convenient, inexpensive and safe .
Furie Bruce, Bouchard BA, Furie BC. Vitamin K-dependent biosynthesis of gamma-carboxyglutamic acid. Blood. 1999;93(6):1798–1808.
Vitamin K has been found to be an essential vitamin. Since the discovery of vitamin K and its association with blood coagulation, many milestones have been passed on the road to understanding the biological role of vitamin K. Because carboxylase activity is found in essentially all mammalian tissues and because γ-carboxyglutamic acid has been observed in both vertebrates and invertebrates, this amino acid must play an important biological role in protein function. The biosynthesis of γ-carboxyglutamic acid is the topic of this review.
Olson RE. In: Shils M, Olson JA, Shike M, Ross AC, eds. Modern Nutrition in Health and Disease. 9th ed. Baltimore: Lippincott Williams & Wilkins; 1999:363-380.
Stenflo J. Contributions of Gla and EGF-like domains to the function of vitamin-K dependent coagulation factors. Crit Rev Eukaryot Gene Expr. 1999;9(1):59-88.
Blood coagulation is a response to vascular injury leading to the activation of platelets and coagulation factors with the ultimate formation of a fibrin plug. Several coagulation factors require vitamin K for normal biosynthesis. This review looked at features of the Gla and EGF-like domains that provide the coagulation serine proteases with unique properties, such as affinity for certain biological membranes, and which also mediate protein-protein interactions.
2000
National Research Council (2000). Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. Washington DC: National Academy Press.
Dahlback B. Blood coagulation. Lancet 2000; 355: 1627–32.
Under normal circumstances, the coagulation system is balanced in favor of anticoagulation. Thrombin is the key effector enzyme of the clotting cascade. Antagonists of vitamin K inhibit a vitamin-K-dependent modification of several coagulation proteins, which is required for these proteins to attain a phospholipid-binding conformation. Gene therapy may soon be a therapeutic option for inherited deficiencies of factors VIII and IX.
Esmon C. The protein C pathway. Crit Care Med. 2000 Sep;28(9Suppl):S44-8.
This article reviewed the emerging knowledge of the multiple mechanisms by which the protein C anticoagulant pathway can control the inflammatory response.
Triplett DA. Coagulation and bleeding disorders: review and update. Clin Chem. 2000 Aug;46(I Pts):1260-9.
Asakura H, Myou S, Ontachi Y, Mizutani T, Kato M, Saito M, et al. Vitamin K administration to elderly patients with osteoporosis induces no hemostatic activation, even in those with suspected vitamin K deficiency. Osteoporos Int. 2001 Dec;12(12):996-1000.
This study looked at whether vitamin K administration alters the clotting system or promotes clots to develop. Elderly women were given large doeses of MK4, 45 MG/3 times a day for 12 weeks. Their clotting parameters remained stable, including the amount of thrombin generated. The results indicated that MK4 can be administered safely and in large doses.
Askim M. Vitamin K in the Norwegian diet and osteoporosis. Tidsskr Nor Laegeforen. 2001;121(22):2614-6.
The level of vitamin K1 in the Norwegian diet is estimated to be 60 micrograms a day, which is too low. Also the incidence of osteoporosis in Norway is high. A study should be done to determine any links and an analysis of vitamin K in Norwegian foods should be conducted.
FAO/WHO. Human vitamin and mineral requirements. Report of a Joint FAO/WHO expert consultation, Bangkok, Thailand. Food and Nutrition Division, FAO Rome. 2002.
Furie B, Furie BC, Roth DA. 2003. Vitamin K-Dependent blood coagulation proteins: Normal function and clinical disorders. Handin RI, Lux SE, Stossel TP. Blood: Principles and Practice of Hematology, 2nd Ed. Vol. 1. Philadelphia (PA). Lippincott, Williams & Wilkins. p. 1157-1194.
Heemskerk JW, Bevers EM, Lindhout T. Platelet activation and blood coagulation. Haemost. 2002 Aug;88(2):186-93.
Platelet activation and blood coagulation are complementary, mutually dependent processes in haemostasis and thrombosis. Platelets interact with several coagulation factors, and can provide binding sites for prothrombin and factor XI. They take over the initiating role of tissue factor in coagulation activation.
Dorffler-Melly J, de Kruif M, Schwarte LA, Franco RF, Florquin S, Spek CA et al. Functional thrombomodulin deficiency causes enhanced thrombus growth in a murine model of carotid artery thrombosis. Basic Res. Cardiol. 2003;98:347-352.
Bauer K, Zwicker J. 2003. Blood: Principles and practice of hematology. Philadelphia, PA: Lippincott Williams & Wilkins.
Esmon C. Inflammation and thrombosis. J Thromb Haem. 2003;1(7) https://doi.org/10.1046/j.1538-7836.2003.00261.x
Systemic inflammation is a potent prothrombotic stimulus. Inflammatory mechanisms upregulate procoagulant factors, downregulate natural anticoagulants and inhibit fibrinolytic activity. Some insights into the evolution and linkages between inflammatory mechanisms and the coagulation/anticoagulation mechanisms have become evident from recent structural studies. This review will summarize the interactions between inflammation and coagulation.
Davie EW. A brief historical review of the waterfall/cascade of blood coagulation. J Biol Chem. 2003;278:50819-32.
This article explores some of the events and people involved in unraveling the basic mechanisms leading to the clotting of blood.
Di Cera E. Thrombin interactions. Chest. 2003;124(Suppl. 3):11S–7.
After generation from prothrombin, thrombin plays multiple roles in the blood coagulation cascade that are mediated by interaction with a number of physiologic substrates, effectors, and inhibitors. The functional versatility of thrombin owes much to its evolutionary origin and results from structural determinants and mechanisms.
Mann KG, Brummel K, Butenas S. What is all that thrombin for? J Thromb Haemost. 2003;1:1504–14.
The consequence of the integration of the effects of procoagulant and anticoagulant systems governing thrombin generation is the establishment of an effectively ‘digital’ system that is either off or on. Once a threshold has been reached, the response of the process is only dictated by the pro†and antiâ€coagulant concentrations present in a reaction volume. This produces a desirable expectation for the hemostatic system, i.e. it responds effectively and rapidly to a threat dealing with hemorrhage but is not provoked to activation by inconsequential stimuli.
Tsutaoka BT, Miller M, Fung SM, Patel MM, Olson KR. Superwarfarin and glass ingestion with prolonged coagulopathy requiring high-dose vitamin K1 therapy. Pharmacotherapy. 2003;Sep;23(9):1186-9.
A 23-year-old man was brought to the emergency department after eating four boxes of brodifacoum-containing rodenticide over a 4-day interval and pieces from approximately two bottles of glass over the previous 2 weeks. He was asymptomatic but his prothrombin time was markedly elevated with an international normalized ratio (INR) of 37.8. At a vitamin K1 dosage of 300 mg/day, the INR corrected to less than 2.0 and the patient was discharged taking that dosage. He returned 26 days later with hematuria and flank pain, and his INR was 189. He was administered FFP and packed red blood cells, and his vitamin K1 dosage was increased to 800 mg/day; his INR returned to baseline. At 5-month follow he was doing well.
Andrews RK, Berndt MC. Platelet physiology and thrombosis. Thromb Res. 2004;114(5-6):447-53.
This review will focus on the structure-function of primary platelet adhesion receptors, GPIb-IX-V and GPVI, and how they act together to regulate platelet thrombus formation in pathophysiology.
Bern M. Observations on possible effects of daily vitamin K replacement, especially upon warfarin therapy. J Parenter Enteral Nutr. 2004;28(6):388-98.
Vitamin K supplements are now recommended by the U.S. Food and Drug Administration (FDA) for patients receiving IV nutrients, on a daily rather than weekly basis. Supplemental vitamin K1 will ensure adequate supplies for hepatic saturation and thus the production of clotting factors II, VII, IX, and X, plus the anticoagulants protein C, protein S, and protein Z. But this is not the entire story. This recommended supplement will affect other physiologic systems that also use vitamin K-dependent gamma-carboxylation. Also considered are possible positive or negative effects that chronic warfarin therapy may have upon the other vitamin K-dependent systems under discussion. This review offers a platform for further discussion and derived clinical research provoked by this new FDA recommendation.
Berkner KL & Runge RW. The physiology of vitamin K nutriture and vitamin K-dependent protein function in atherosclerosis. J Thromb Haemost. 2004 Dec;2(12):2118-32.
Recent advances have led to a substantial revision in our understanding of vitamin K physiology. While vitamin K was originally associated only with hepatic VKD proteins that participate in hemostasis, VKD proteins are now known to be present in virtually every tissue. New assays have revealed that while the current recommended daily allowance for vitamin K is sufficient for maintaining functional hemostasis, the undercarboxylation of at least one non-hemostatic protein is frequently observed in the general population. Recent studies suggest VKD proteins are involved in arterial calcification, which may be influenced by dietary levels of vitamin K and by anticoagulant drugs such as warfarin that antagonize vitamin K action.
Colvin BT. Physiology of haemostasis. Vox Sang. 2004;87(Suppl 1):43–6.
Gunther KE, Conway G, Leibach L, Crowther MA. Low-dose oral vitamin K is safe and effective for outpatient management of patients with an INR>10. Thromb Res. 2004;113(3-4):205-9.
Low-dose (2 mg) oral vitamin K, coupled with temporary warfarin discontinuation, appears to be a safe and effective treatment for severe warfarin associated coagulopathy in non-bleeding patients.
Aoki N, Ohdama S-C, Hirokawa K. Thrombomodulin: Its expression and release into the circulation. Current Aspects of Blood Coagulation, Fibrinolysis, and Platelets. Conference Proceedings. 1993:14-16.
Thrombomodulin is a thrombin-binding anticoagulant cofactor, which is expressed on the surface of endolethial cells. This study looked at the surface activity of thrombomodulin. TM converts procoagulant thrombin to an anticoagulant and plays a central role in the protein C anticoagulant pathway.
Schenone M, Furie BC, Furie B. The blood coagulation cascade. Curr Opin Hematol 2004; 11: 272–7.
This article summarizes some of the advances that have been made in this field from the last quarter of 2002 and during 2003.
Dahlback B. Blood coagulation and its regulation by anticoagulant pathways: genetic pathogenesis of bleeding and thrombotic diseases. J of Int Med. 2005;257:209-223.
The reactions of blood coagulation are carefully controlled by several anticoagulant mechanisms and under normal conditions they prevail over the procoagulant forces. Genetic or acquired disturbances of the natural balance between the pro- and anticoagulant systems may result in bleeding or thrombotic diseases.
Dahlback B, Villoutreix BO. Regulation of blood coagulation by the protein C anticoagulant pathway: novel insights into structure-function relationships and molecular recognition. Arterioscler Thromb Vasc Biol. 2005 Jul;25(7):1311-20.
The protein C system provides important control of blood coagulation by regulating the activities of factor VIIIa (FVIIIa) and factor Va (FVa), cofactors in the activation of factor X and prothrombin, respectively. The system comprises membrane-bound and circulating proteins that assemble into multi-molecular complexes on cell surfaces. The protein C system is physiologically important, and genetic defects affecting the system are the most common risk factors of venous thrombosis.
Dahlback B, Villoutreix BO. The anticoagulant protein C pathway. FEBS Lett. 2005;579(15):3310-6.
The anticoagulant protein C system regulates the activity of coagulation factors VIIIa and Va, cofactors in the activation of factor X and prothrombin, respectively. The protein C system contains multi-domain proteins, the molecular recognition of which will be reviewed.
Espana F, Medina P, Navarro S, Zorior E, Estelles A, Aznar J. The multifunctional protein C system. Curr Med Chem Cardiovasc Hematol Agents. 2005;3(2):119-31.
The importance of the protein C anticoagulant pathway is emphasized by the increased risk of venous thromboembolism (VTE) associated with protein C and protein S deficiencies, the factor V Leiden mutation, and reduced circulating APC levels. The protein C pathway also plays a significant role in inflammatory processes, since it prevents the lethal effects of E. coli-associated sepsis in animal models and improves the outcome of patients with severe sepsis. This review summarizes the mechanisms that contribute to these biological activities of the protein C pathway.
Jesty J, Beltrami E. Positive feedbacks of coagulation: their role in threshold regulation. Arterio Thromb Vasc Biol. 2005;25(12):2463-9.
This article reviews the evidence for system idling, the structures of the various feedback mechanisms of clotting, the mechanisms by which they can produce threshold behavior, and the possible role of thresholds in system regulation. It focuses on tissue factor (TF), the initiator of coagulation, which continuously circulates in the plasma, and the clotting system which "idles," generating very low levels of active clotting enzymes, clotting products, and by-products. Given the enormous amplification potential of the clotting cascade, rigorous control is required to ensure that such low-level stimulation does not cause massive system amplification and response. We propose that among the various mechanisms of regulation, activation thresholds may play a major role. Such thresholds act like switches, so that small stimuli and/or nonproductive local conditions will generate no response, whereas larger stimuli or the existence of local prothrombotic conditions will produce a full, explosive response.
Reese AM, Farnett LE, Lyons RM, Patel B, Morgan L, Bussey HI. Low-dose vitamin K to
augment anticoagulation control. Pharmacotherapy. 2005 Dec;25(12):1746-51.
85 patients on warfarin with fluctuating INRs were supplemented daily with vitamin K, 100 micrograms a day. After vitamin K supplementation, INR fluctuations diminished in nearly all patients, significantly. They concluded that daily low-dose vitamin K was beneficial.
Panteleev MA, Ovanesov MV, Kireev DA, Shibeko AM, Sinaurze EL, Anayeva NM, et al. Spatial propagation and localization of blood coagulation are regulated by intrinsic and protein C pathways, respectively. Biophysical J. 2006;90(5):1489-1500.
Blood coagulation in vivo is a spatially non-uniform, multistage process: coagulation factors from plasma bind to tissue factor (TF)-expressing cells, become activated, dissociate, and diffuse into plasma to form enzymatic complexes on the membranes of activated platelets. This article studied spatial regulation of coagulation and identified the roles of specific pathways at different stages.
Pirmohamed M. Warfarin. Almost 60 years and still causing problems. Br J Clin Pharma. 2006 Nov;62(5):509-11.
Schurgers LJ, Aebert H, Vermeer C, Bültmann B, Janzen J. Oral anticoagulant treatment: friend or foe in cardiovascular disease. Blood. 2004;104:3231-3232.
Calcification is a common complication in cardiovascular disease and may affect both arteries and heart valves. In animal models, vitamin K antagonists (oral anticoagulants [OACs]) were shown to induce arterial calcification. To investigate whether long-term OAC treatment may induce calcification in humans also, we have measured the grade of aortic valve calcification in patients with and without preoperative OAC treatment. These observations suggest that OACs, which are widely used for antithrombotic therapy, may induce cardiovascular calcifications as an adverse side effect.
Renné T, Pozgajová M, Grüner S, Schuh K, Pauer HU, Burfeind P, et al. Defective thrombus formation in mice lacking coagulation factor XII. J Exp Med. 2005 Jul;202(2):271–81.
They studied blood coagulation, and established that clotting factor XII is essential for clot formation, and identify factor XII as a novel target for anti-clotting therapy.
Corral J, Gonzalez-Conejero R, Hernandez-Espinosa D, Vicente V. Protein Z/Z-dependent protease inhibitor (PX/XPI) anticoagulant system and thrombosis. Br J Haematol. 2007;137:99-108.
Handin RI, Lux SE. 1995. Blood: Principles and Practices of Hematology. Philadelphia (PA): Lippincott.
Sconce E, Avery P, Wynne H, Kamali F. Vitamin K supplementation can improve stability of anticoagulation for patients with unexplained variability in response to warfarin. Blood. 2007 Mar 15;109(6):2419-23.
Patients receiving warfarin who have unstable control of anticoagulation have a significantly lower intake of dietary vitamin K compared with their stable counterparts. Seventy warfarin-treated patients with unstable anticoagulation control were randomly assigned in a double-blinded fashion to receive a daily amount of 150 mcg oral vitamin K, or placebo orally for six months. Anticoagulation control improved in 33 of 35 patients receiving vitamin K supplementation; of these, 19 fulfilled our criteria for having stable control of anticoagulation. However, only 24 of 33 patients receiving placebo demonstrated some degree of improvement, with only 7 patients fulfilling the criteria for having stable control. Supplementation of vitamin K can significantly improve anticoagulation control in patients with unexplained instability of response to warfarin.
Spahr JE, Maul JS, Rodgers GM. Superwarfarin poisoning: a report of two cases and review of the literature. Am J Hematol 2007;82(7):656-660.
Superwarfarins are anticoagulant rodenticides similar to warfarin, but which have various substituted phenyl groups replacing the terminal methyl group, resulting in a fat-soluble, long-acting anticoagulant that is nearly 100 times more potent than the parent compound.
We describe two cases of consumption, one related to unknown etiology, and the other related to utilization of the superwarfarin to potentiate a drug of abuse. The clinical manifestations including bleeding symptoms and abnormal coagulation assays are discussed.
Zhu A, Sun H, Raymond RM Jr, Furie BC, Furie B, et al. Fatal hemorrhage in mice lacking gamma-glutamyl carboxylase. Blood. 2007 June 15;109(12):5270-5.
The carboxylation of glutamic acid residues to gamma-carboxyglutamic acid (Gla) by the vitamin K-dependent gamma-glutamyl carboxylase (gamma-carboxylase) is an essential posttranslational modification required for the biological activity of a number of proteins, including proteins involved in blood coagulation and its regulation. This study looked at mice carrying a mutation for gamma-carboxylase. Only 50% of offspring survive to birth, due to hemorrhage. This outcome, with other data, suggest broad functional importance of carboxylation, that affects multiple biologic processes.
Bresson JL, Flynn A, Heinonen M, et al. Vitamin K2 added for nutritional purpose in foods for particular nutritional uses, food supplements and foods intended for the general population. EFSA J. 2008;822:1–31.
Castoldi E, Hackeng TM. Regulation of coagulation by protein S. Curr Opin Hematol. 2008 Sep:15(5);529-36.).
Protein S expresses both activated protein C-dependent and activated protein C-independent anticoagulant activities. This review underscore the central role of protein S in the regulation of coagulation and may have important implications for the evaluation of the thrombotic risk associated with protein S deficiency.
Wolberg AS, Campbell RA. Thrombin generation, fibrin clot formation and hemostasis. Transfux Apher Sci. 2008 Feb;38(1):15-23.
Clot formation entails thrombin-mediated cleavage of fibrinogen to fibrin. Recent studies suggest that abnormal thrombin generation patterns produce abnormally structured clots associated with an increased risk of bleeding or thrombosis. Further studies of fibrin formation during in situ thrombin generation are needed to understand fibrin clot formation in vivo.
2010
Castoldi E, Maurissen LF, Tormene D, Spieia L, Gavasso S, Radu C, et al. Similar hypercoagulable state and thrombosis risk in type I and type III protein S-deficient individuals from families with mixed type I/III protein S deficiency. Haemetologica. 2010 Sep;95(9):1563-71.
Protein S, which circulates in plasma in both free and bound forms, is an anticoagulant protein that stimulates activated protein C and tissue factor pathway inhibitor. This study looked at individuals with protein S deficiency and they found that both types of deficiency are associated with an increased risk of thrombosis.
Hall JE. Guyton and Hall Textbook of Medical Physiology: Enhanced E-Book. 11th ed. Philadelphia: Elsevier Health Sciences; 2010. Chapter 36, Hemostasis and blood coagulation; pp. 457–9.
Soare AM, Popa C. Deficiencies of proteins C, S and antithrombin and activated Protein C resistance--their involvement in the occurence of arterial thromboses. J Med Life. 2010 Oct-Dec;3(4):412-5.
Deficiencies of natural anticoagulants protein C, protein S, antithrombin and activated protein C resistance are components of inherited thrombophilia. Inherited thrombophilia was defined as a genetically determined tendency towards venous thromboembolism, which characteristically occurs in young patients (before 40 to 45 years old), without apparent causes, and tend to recur. Screening is recommended in order to get treatment.
Davis PJ, Cladis FP, Motoyama EK. Smith’s Anesthesia for Infants and Children, 8th Ed. Elsevier, Amsterdam, Netherlands. 2011. Chapter 36. Systemic Disorders, by Lynn G Maxwell, Salvatore R Goodwin, Thomas J Mancuso, Victor C Baum, Aaron L Zuckerberg, Philip G Morgan, Etsuro K Motoyama, Peter J Davis, Kevin J Sullivan.
Marlar RA, Gausman JN. Protein S abnormalities: A diagnostic nightmare. J of Hema. 2011;86(5):418-421.
Heterozygous deficiency of Protein S (PS) increases the risk for developing thrombosis. Many acquired conditions alter plasma PS levels. It is important to diagnosis Protein S deficiency. This article reviews the three basic assays available and their associated problems. They also discuss the confounding and interfering factors that make it difficult to obtain an accurate diagnosis of PS deficiency.
Moussa AA. 2011. Thrombomodulin and antithrombin-III as evidence for varied activation of the coagulation cascade. ObGyn.net; [accessed July 2018].
,http://www.obgyn.net/pregnancy-and-birth/thrombomodulin-and-antithrombin-iii-evidence-varied-activation-coagulation-cascade
The current study was conducted to understand the relevance of the endothelium to subsequent activation of the coagulation cascade and to determine the changes of two natural anticoagulant factors, circulating TM levels and AT-III activity, in pre-eclamptic pregnancies.
Vermeer C, Knapen MH. 2012. Vitamin K and bone. In: Anderson JJB, Garner SC, and Klemmer PJ. Diets, nutrients, and bone health. Boca Raton (FL); CRC Press. Ch. 12.
Holmes MV, Hunt BJ, Shearer MJ. The role of dietary vitamin K in the management of oral vitamin K antagonists. Blood Rev. 2012;26:1–14.
This review assesses the evidence for the importance of vitamin K nutrition during VKA (warfarin) therapy. Preliminary evidence suggests that the stability of anticoagulation therapy may be improved by daily vitamin K supplementation, but further studies are needed to find out whether this, or other dietary interventions, can improve anticoagulant control in routine clinical practice.
Schurgers LJ, Joosen IA, Laufer EM, Chatrou MLL, Herfs M, Winkens MHM, et al. Vitamin K-antagonists accelerate atherosclerotic calcification and induce a vulnerable plaque phenotype. PloS One. 2012;7(8):343229.
Vitamin K-antagonists (VKA) (warfarin) are treatment of choice and standard care for patients with venous thrombosis and thromboembolic risk. In experimental animal models as well as humans, VKA have been shown to promote vascular calcification. As vascular calcification is considered an independent risk factor for plaque instability, this study investigated the effect of VKA on coronary calcification in patients and on calcification of atherosclerotic plaques in the ApoE model of atherosclerosis.
Theuwissen E, Cranenburg EC, Knapen MH, Magdeleyns EJ, Teunissen KJ, Schurgers LJ, et al. Low-dose menaquinone-7 supplementation improved extra-hepatic vitamin K status, but had no effect on thrombin generation in healthy subjects. Br J Nutr 2012;108: 1652–1657.
This study looked at the effects of extra intake of menaquinones on the carboxylation of the extra-hepatic Gla-proteins. A total of forty-two healthy Dutch men and women received either placebo capsules or menaquinone-7 (MK-7) capsules at a daily dose of 10, 20, 45, 90, 180 or 360 μg. Circulating uncarboxylated OC (ucOC), carboxylated OC (cOC) and desphospho-uncarboxylated MGP were measured. MK-7 supplementation at doses in the order of the RDA increased the carboxylation of circulating uncarboxylated OC and MGP. No adverse effects on thrombin generation were observed. Extra MK-7 intake at nutritional doses around the RDA improved the carboxylation of the extra-hepatic vitamin K-dependent proteins. Whether this improvement contributes to public health, i.e. increasing the protection against age-related diseases needs further investigation in specifically designed intervention trials.
Vermeer C. Vitamin K: the effect on health beyond coagulation – an overview. Food Nutr Res. 2012; 56: 10.3402/fnr.v56i0.5329.
Vitamin K is essential for the synthesis of proteins belonging to the Gla-protein family. The four blood coagulation factors, belong to this family. Other members of the Gla-protein family are osteocalcin, matrix Gla-protein (MGP), and Gas6 that play key functions in maintaining bone strength, arterial calcification inhibition, and cell growth regulation, respectively. In total 17 Gla-proteins have been discovered at this time. The dietary vitamin K requirement is based on the need for clotting, and doesn’t account for the needs of the other Gla-proteins. The triage theory states that during poor dietary supply, vitamins are preferentially utilized for functions that are important for immediate survival. This explains why in the healthy population all clotting factors are synthesized in their active form, whereas the synthesis of other Gla-proteins is sub-optimal in non-supplemented subjects. Prolonged sub-clinical vitamin K deficiency is a risk factor for osteoporosis, atherosclerosis, and cancer. Accumulating scientific data suggests that new, higher recommendations for vitamin K intake should be formulated.
PMCID: PMC3321262
Westenfeld R, Krueger T, Schlieper G, Cranenburg EC, Magdeleyns EJ, Heidenreich S, et al. Effect of vitamin K2 supplementation on functional vitamin K deficiency in hemodialysis patients: a randomized trial. Am J Kidney Dis. 2012;59:186–195.
This study confirms that most hemodialysis patients have a functional vitamin K deficiency. More importantly, it is the first study showing that inactive MGP levels can be decreased markedly by daily vitamin K(2) supplementation. Our study provides the rationale for intervention trials aimed at decreasing vascular calcification in hemodialysis patients by vitamin K supplementation.
Lanzer P, Topol EJ. 2013. Pan Vascular Medicine: Integrated Clinical Management. reprint of 1st edition, 2002. New York City. Springer Science & Business Media. New York City.
Majeed H, Rodger M, Forgie M, Carrier M, Taljaard M, Scarvelis D, et al. Effect of 200 uG/day of vitamin K1 on the variability of anticoagulation control in patients on warfarin: a randomized controlled trial. Thromb Res. 2013 Sep;132(3):329-35.
Controversy exists whether low-dose vitamin K supplementation can improve anticoagulation control in patients with unstable anticoagulation under warfarin. In a single-centre randomized, double-blind, placebo-controlled study, this study evaluated the effectiveness of 200 μg/day of vitamin K1 in patients with unstable control under warfarin. Vitamin K1 supplementation reduces the standard deviation of INRs as an indicator of the variability in anticoagulation control in patients treated with warfarin for venous embolisms.
Beulens JWJ, Booth SL, van den Heuvel E, Stoecklin E, Baka A, Vermeer C. The role of menaquinones (vitamin K2) in human health. Brit J Nutr. 2013 Oct;110(8):1357-68.
Present dietary reference values (DRV) for vitamin K are exclusively based on phylloquinone, and its function in coagulation. The present review describes the current knowledge on menaquinones, or vitamin K2. Dietary intake of menaquinones accounts for up to 25 % of total vitamin K intake and contributes to the biological functions of vitamin K. However, menaquinones are different from phylloquinone with respect to their chemical structure and pharmacokinetics, which affects bioavailability, metabolism and perhaps impact on health outcomes. There are significant gaps in the current knowledge on menaquinones based on the criteria for setting DRV. Therefore, we conclude that further investigations are needed to establish how differences among the vitamin K forms may influence their role in human health and the recommended daily allowance.
Suleiman L, Negrier C, Boukerche H. Protein S: A multifunctional anticoagulant vitamin-K dependent protein at the crossroads of coagulation, inflammation, angiogenesis and cancer. 2013. Crit Revs in Oncology/Hematology. 2013;88:637-654.
Since its discovery in 1970, protein S (PS) has emerged as a key vitamin K-dependent natural anticoagulant protein involved with multiple biological processes, including coagulation, apoptosis, atherosclerosis, angiogenesis/vasculogenesis, and cancer progression. The purpose of this review is to provide a brief chronicle of the discovery and current understanding of the mechanisms of PS signaling, and how PS regulate various cellular functions.
Wypasek E, Undas A. Protein C and protein S deficiency – practical diagnostic issues. Adv Clin Exp Med. 2013 jul-aug;22(4):459-67.
Protein C (PC) and protein S (PS) are vitamin K-dependent glycoproteins, that act as natural anticoagulants. The activation of PC by thrombin occurs on the surface of endothelial cells and involves thrombomodulin and endothelial Protein C receptor. Patients with low PC and PS levels and the known mutation within PROC or PROS1 genes combined with other genetic or environmental thrombosis factors are at increased risk of recurrent thromboembolic events and require lifelong oral anticoagulation.
Nowak JA, Grzubowska-Chlebowczyk U, Landowski P, Szaflarska-Poplawska A, Klincewicz B, et al. Prevalence and correlates of vitamin K deficiency in children with inflammatory bowel disease. Sci Rep. 2014;4:4768.
Palta S, Saroa R, Palta A. Overview of the coagulation system. Indiana J Anaesth. 2014 Sep-Oct; 58(5):515-523.
Coagulation is a dynamic process and the understanding of the blood coagulation system has evolved over the recent years. Normal coagulation pathway represents a balance between the pro-coagulant pathway that is responsible for clot formation and the mechanisms that inhibit the same beyond the injury site. Imbalance between the two components predisposes a patient to either bleed or present with thrombosis. The physiology needs to be understood to predict the pathological and clinical consequences before treatment.
Grober U, Reichrath J, Holick MF, Kisters K. Vitamin K: an old vitamin in a new perspective. Dermatoendocrinol. 2015 jan 21;6(1): e968490.
The following review describes the history of vitamin K, the physiological significance of the K vitamers, updates skeletal and cardiovascular benefits and important interactions with drugs.
Monroe III DM, Hoffman M, Roberts HR. 2010. Williams Hematology. 8th ed. New York NY: McGraw-Hill Professional Publishing. Chapter 115. Molecular biology and biochemistry of the coagulation factors and pathways of hemostasis; pp. 614–6.
Krutsch JP. 2011. Anesthesia secrets, 4th Ed. In: Duke J. ed. Coagulation; Coagulation. Philadelphia (PA), Elsevier, p. 51-57.
Doolittle RF. Some important milestones in the field of blood clotting. J of Innate Immunity. 2016;8:23-29.
Several different milestones in the field of blood coagulation are described. The first milestone considered is the role of vitamin K. The second relates to the discovery of the ‘new’ clotting factors after World War II. A third focuses on the transformation of fibrinogen into fibrin.
Yasuda N, Goto K, Ohchi Y, Abe T, Koga H, Kitano T. The efficacy and safety of antithrombin and recombinant human thrombomodulin combination therapy in patients with severe sepsis and disseminated intravascular coagulation. J of Crit Care. 2016 Dec;36:29-34.
This study looked at treatments with thrombomodulin and antithrombin for intravascular clots. Their data suggested that combination therapy with both was more effective in improving platelet counts, as well as in reducing mortality.
Kampouraki E, Kamali F. Dietary implications for patients receiving long-term oral anticoagulation therapy for treatment and prevention of thromboembolic disease. Expert Rev Clin Pharmacol. 2017 Aug;10(8):789-797. doi: 10.1080/17512433.2017.1345622. Epub 2017 Jun 26.
The effectiveness of oral anticoagulation therapy with warfarin (a vitamin K antagonist) for blood clot risk is well recognised. However, warfarin has an unpredictable anticoagulation response, which make it difficult to achieve and maintain optimal anticoagulation. In this article, they cover the results of studies on the effect of vitamin K supplementation on anticoagulation stability. Expert commentary: A stable dietary vitamin K, promoted by daily oral vitamin K supplementation, can improve anticoagulation stability in patients on warfarin therapy.
Caluwe R, Pyfferpen L, De Boeck K, De Vriese AS. The effects of vitamin K supplementation and and vitamin K antagonists on progression of vascular calcification: ongoing randomized controlled trials. Clin Kidney J. 2016 Apr;9(2):273-9.
Vitamin K is essential for the activation of matrix gla protein (MGP), a powerful inhibitor of tissue calcification. Functional vitamin K deficiency may contribute to the high vascular calcification burden in haemodialysis patients. In addition, haemodialysis patients are frequently treated with vitamin K antagonists, mainly to prevent stroke in atrial fibrillation, potentially compounding the cardiovascular risk. This study looked at hemodialysis patients being treated with vitamin K antagonists. They concluded that supplementing with vitamin K could reduce the cardiovascular risk.
Tie JK, Stafford DW. Structural and functional insights into enzymes of the vitamin K cycle. J Thromb Haemost. 2016 Feb;14(2):236-47.
Dahlberg S, Nilsson CU, Kander T, Schott U. Detection of subclinical vitamin K deficiency in neurosurgery with PIVKA-II. Scand J Clin Lab Invest 2017 Jul;77(4):267-274.
Vitamin K is known for supporting the carboxylation of hepatic coagulation proteins. Levels of proteins induced by vitamin K absence for factor II (PIVKA-II) reflect under-carboxylated prothrombin and can be used to detect subclinical vitamin K deficiency. The aim of this study was to determine the prevalence of perioperative subclinical vitamin K deficiency among neurosurgical patients using PIVKA-II and investigate the existence of any correlation to standard coagulation assays. Thirty-five patients undergoing brain tumor resection were included. In conclusion, PIVKA-II was increased in many patients preoperatively and then increased by the morning following surgery. Standard coagulation assays were largely non-pathological. The effect of perioperative treatment with different vitamin K supplements should be investigated in future studies, as well as clinical trials evaluating their antitumor effects.
McCarron JG, Lee MD, Wilson C. The endothelium solves problems that endothelial cells do not know exist. Trends Pharmacol Sci. 2017Apr;38(4):322-338.
The endothelium is the single layer of cells that lines the entire cardiovascular system and regulates vascular tone and blood-tissue exchange, recruits blood cells, modulates blood clotting, and determines the formation of new blood vessels. To control each function, the endothelium uses a remarkable sensory capability to continuously monitor small changes in the concentrations of many simultaneously arriving extracellular activators that each provides cues to the physiological state. They propose that the sensing is distributed among cells, working as a collective.
Aleksandrov AP, Mirkov, Ninkov M, Kataranovski M. Effects of warfarin on biological processes rather than haemostatis: A review. Food and Chemical Toxicology. 2018 Jan;113.
Warfarin is the world's most widely used anticoagulant drug. Its anticoagulant activity is based on the inhibition of the vitamin K-dependent (VKD) step in the complete synthesis of a number of blood coagulation factors that are required for normal blood coagulation. Warfarin also affects synthesis of VKD proteins not related to haemostasis, including those involved in bone growth and vascular calcification. This review provides an overview of the published data dealing with the effects of warfarin on biological processes other than haemostasis.
Dahlback B. Vitamin K dependent protein S: Beyond the protein C pathway. Semin Thromb Hemost. 2018 Mar;44(2):176-184.
Protein S is a vitamin K-dependent protein circulating in plasma. Protein S in plasma has multiple anticoagulant properties and deficiency is associated with increased risk of blood clots. Protein S has additional functions beyond being an anticoagulant. This review will discuss the multiple functions of protein S, describing its role as cofactor to activated protein C with a subsequent focus on the other functions of protein S.
Saad J, Schoenberger L. Physiology, platelet activation. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482478/
This article reviews the physiological components of platelet activation during primary hemostasis.
Written by RPT 7/12/18
"In life, in any given situation, one can either be a winner, a loser, or a victim.
If you keep your nose clean, work hard, work smart, and pay attention,
you will win far more than you lose - - - but every now and then you will
lose - - - no worries - - - but what is unacceptable is being a victim.
I chose not be a victim.” - Pat
Click here to read his story
Koncentrated K
USA
Phone: (715) 612-5858
Copyright © 2024 Koncentrated K, web content in part or in whole may not be used without written consent. All rights reserved.