Published Research-Vitamin K and the Kidneys
Vitamin K, Kidneys and Heart Disease
An Extensive Overview of a Complicated Pathway
Simply Put:
Kidney Disease Induces Heart Disease
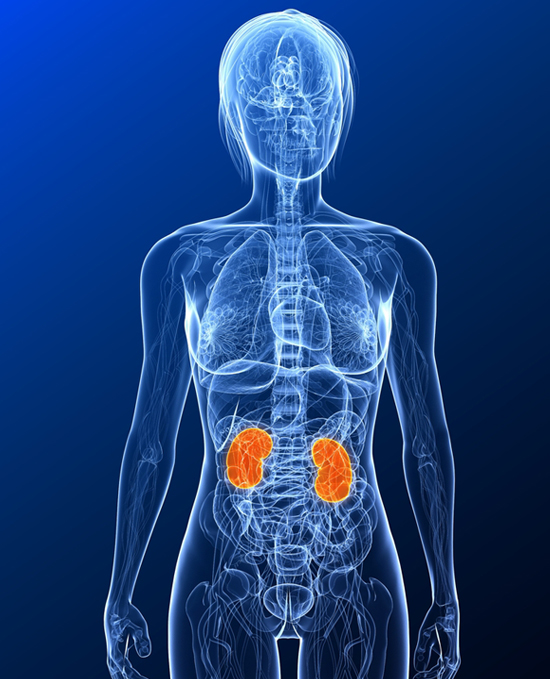
The kidneys are a pair of organs vital to the systemic health of your body. They are bean-shaped, each about the size of a fist and are located near the middle of the back, just below the rib cage, one on each side of the spine. The kidneys have many functional roles, including fluid and electrolyte balance, waste removal, acid-base balance, bone health, and stimulation of red blood cell production. Every day, a person's kidneys process about 200 quarts of blood to sift out about 2 quarts of waste products and extra water. Bodily waste comes from the normal breakdown of tissue and digestion. The waste flows in the blood through the kidneys to become urine. The urine travels through tubes called ureters to the bladder where it is stored until urination. If the kidneys did not process this waste it would build up in the blood and damage the body.
The actual removal of wastes occurs in tiny units inside the kidneys called nephrons. Each kidney has about a million nephrons. In the nephron, a glomerulus-which is a specialized nephron capillary bed-intertwines with a tiny urine-collecting tube called a tubule. The glomerulus acts as a filtering unit, or sieve, and keeps normal proteins and cells in the bloodstream, allowing extra fluid and wastes to pass through. A complicated chemical exchange takes place, as waste materials and water leave the blood and enter the urinary system. At first, the tubules receive a combination of waste materials and chemicals the body can still use. The kidneys measure out chemicals like sodium, phosphorus, and potassium and release them back to the blood to return to the body. In this way, the kidneys regulate the body's level of these substances. The right balance is necessary for life.
Kidney function is calculated using a blood sample and a formula to find the estimated glomerular filtration rate (eGFR). The eGFR corresponds to the percent of kidney function available. Some people are born with only one kidney but can still lead normal, healthy lives. For many people with reduced kidney function, a kidney disease is also present and will get worse. When kidney function drops below 10 to 15 percent, a person needs some form of renal replacement therapy—either blood-cleansing treatments called dialysis or a kidney transplant to sustain life. Given that kidneys are a key part of maintaining a sophisticated balance of chemicals within the body, a decline in their functioning has serious implications for health (http://kidney.niddk.nih.gov/kudiseases/pubs/yourkidneys).
The factors that influence the onset and the speed of kidney failure are not completely understood.
An acute kidney injury (AKI), is when an accident injures the kidneys, or when some drugs or poisons can make the kidneys stop working. Some doctors may also refer to this condition as acute renal failure (ARF). AKI may lead to permanent loss of kidney function, but if the kidneys are not seriously damaged, acute kidney disease may be reversed.
Most kidney problems, however, happen slowly. Gradual loss of kidney function is called chronic kidney disease (CKD) or what used to be known as chronic renal insufficiency. People with CKD may go on to develop permanent kidney failure, and must cope with the consequences of how kidney failure impacts the other organs, skeletal structure, mineral systems, and general health of the body. Data shows that people with CKD also gain a high risk of death from a stroke or heart attack. Other health issues can lead to chronic kidney disease, such as diabetes, or glomerulonephritis. Together, these cause approximately 75% of all adult cases. (http://www.usrds.org).
Total or nearly total and permanent kidney failure is called end-stage renal disease (ESRD). People with ESRD must undergo dialysis or transplantation to stay alive.
Chronic Kidney Disease
In the past Chronic Kidney Disease (CKD) was understood to be a progressive syndrome in which as the kidneys lose their renal functions, or their ability to filter blood, concentrate urine, excrete wastes, and maintain electrolyte balance, leading to a progressive deterioration of the mineral balance within the body. This leads to a disruption of the normal blood and tissue concentrations of phosphorus and calcium, and also leads to changes in circulating levels of hormones (KDIGO, 2009). Some of these hormones include the parathyroid hormone (PTH), vitamin D and other vitamin D metabolites, and the mineral metabolism in general. This can take place over months or years. The symptoms of worsening kidney function are non-specific, and might include feeling generally unwell, and a reduced appetite (Stenvinkel, 2010). Because of the asymptomatic nature of the disease, CKD is often not detected until its later stages when symptoms start to emerge (Slatopolsky and Delmez, 1994).
CKD is identified by a blood test for creatinine. Creatinine is a by-product of the creatine phosphate in normal muscle contractions, which becomes a chemical waste product filtered from the blood through the kidneys. If the filtering of the kidney is deficient, blood levels of creatinine rise. Therefore creatinine levels in blood and urine may be used to calculate the creatinine clearance (CrCl), which reflects the glomerular filtrate rate (GFR) or the flow rate of filtered fluid through the kidney. A higher level of creatinine indicates a lower GFR and a decreased capability of the kidneys to excrete waste products.
BUN refers to blood urea nitrogen, and is often significantly elevated in CKD. Blood carries protein to cells throughout the body. After the cells use the protein, the remaining waste product is returned to the blood as urea, a compound that contains nitrogen. Healthy kidneys take urea out of the blood and put it in the urine. If a person's kidneys are not working well, the urea will stay in the blood. Other possible causes of an elevated BUN include dehydration and heart failure.
Albuminuria refers to the amount of blood proteins in the urine. Healthy kidneys take wastes out of the blood but leave protein. Impaired kidneys may fail to separeate a blood protein called albumin from the wastes. As kidney function worsens, the amount of albumin and other proteins in the urine increases, and the condition is called proteinuria. A doctor may test for protein using a dipstick in a small sample of a person's urine taken in the doctor's office. The color of the dipstick indicates the presence or absence of proteinuria.
Chronic Kidney Disease Stages
Professional guidelines classify the severity of chronic kidney disease in five stages, with Stage 1 being the mildest and usually causing few symptoms and Stage 5 being a severe illness with poor life expectancy if untreated. Stage 5 CKD is often called End Stage Renal Disease (ESRD)and is synonymous with the now outdated terms chronic kidney failure(CKF) or chronic renal failure (CRF) (National Kidney Foundation, 2002). In Stage 5, there is established kidney failure, (GFR less than 15 mL/min/1.73, and elevated creatinine and BUN), and often permanent renal replacement therapy takes place via dialysis or kidney transplantation to prolong life. End-stage renal disease (ESRD) is the end result of many forms of CKD. (ESRD can be considered an anticoagulant-like condition and functional vitamin K insufficiency).
Chronic Kidney Disease-Bone Mineral Disorder (CKD-MBD)
It is now understood that CKD is not a disease simply limited to kidney dysfunction, but that the disturbances in mineral metabolism of kidney dysfunction results in a multisystem disorder (Brandenburg et al., 2009; Lindberg et al. 1999; Cunningham et al., 2004; Gal-Moscovici & Sprague, 2007). The Kidney Disease-Improving Global Outcomes (KDIGO) Workgroup saw the need to expand the understanding of the complex systemic impact of CKD (Moe et al., 2006) and they created the term CKD-MBD, Chronic Kidney Disease-Mineral and Bone Disorder; defined as a systemic disorder of mineral and bone metabolism due to CKD which divides patients into groups based on abnormalities in the three primary components used (KDIGO; 2009):
· Abnormalities of calcium, phosphorus, parathyroid hormone (PTH),, or vitamin D metabolism
· Abnormalities in bone turnover, mineralization, volume, linear growth, or strength
· Vascular or other soft tissue calcification.
--Abnormalities of calcium, phosphorus, parathyroid hormone, vitamin D metabolism, and other mineral dysregulation.
|
· Hyperphosphatemia. Phosphorus is a mineral found in a wide variety of foods. When you eat these foods, your body takes the phosphorus content and creates a related substance called phosphate. Most phosphate is held in your bones, however, a small percentage of it, called serum phosphate, circulates in your bloodstream. The kidneys are the major organ responsible for regulating serum phosphate levels, via filtering through the glomerulus and reabsorption by the proximal tubules. When the glomerular filtration rate (GFR) declines, phosphate is retained, and accumulates in the blood at abnormal levels. Failing kidneys do not convert enough vitamin D to its active form, and they do not adequately excrete phosphate. This can begin as early as CKD Stage II (Slatopolsky & Delmez, 1994). This is called hyperphosphatemia. Hyperphosphatemia is a central characteristic problem in CKD-BM, affecting between 30 and 50% of patients undergoing dialysis (Block et al., 1998), and has been a central focus of treatment (Savica et al, 2006). Phosphorus is critical for numerous normal physiological and cellular functions, so phosphate retention can trigger a cascade of events that can affect the mineral balance. It can stimulate the parathyroid gland by promoting parathyroid hormone secretion and synthesis (Naveh-Many et al., 2002; Moe et al, 2003), leading to secondary hyperparathyroidism (2HPT). Hyperphosphatemia is also an independent cardiovascular risk factor and potent predictor of cardiovascular morbidity and mortality in patients with advanced CKD (Ganesh et al, 2001; Block et al, 2004; Stevens et al, 2004; Slinin et al, 2005; Foley et al., 2009) and predicts a higher incidence of cardiovascular events than the normal population (Tonelli, et al, 2005). Per Foley, more than 50% of deaths in these patients are due to cardiovascular disease, a risk that is 20 to 30 fold higher than in the general population. In vitro studies indicate that high levels of phosphate induce calcification by causing vascular smooth muscle cells to transform into osteoblast-like cells that express bone-related proteins that regulate mineralization (Block & Port, 2000; Jono et al, 2000; Steitz et al, 2001; Wada et al, 1999; Chen et al, 2002; Shanahan,2005; Bellosta et al., 2007; Liu & Shanahan, 2011), such as alkaline phosphates, osteopontin, osteocalcin, and collagen. The net effect of these changes is to provide an optimal microenvironment within the vasculature for mineral deposition, enhancing susceptibility to vascular calcification. Similar osteogenic differentiation of VSMCs has been observed in vivo, in human and animal models of vascular calcification. (Steitz et al., 2001; Rattazzi et al., 2005; Moe et al., 2002; Moe et al., 2003; Krueger et al., 2009; Palmer et al., 2011). Additionally, phosphate often collaborates with calcium whereby elevated calcium and phosphorus together trigger vascular smooth muscle cell (VSMC) death and/or change to osteoblast-like cells, leading the vessels and soft tissues to calcify (Jono et al., 2000; Yang et al., 2004). Reynolds (et al., 2004) demonstrated that even modest increases in calcium can exacerbate mineralization in the presence of high phosphate concentrations. |
· Hyperparathyroidism (HPT). Hyperphosphatemia is a driving force in the development of hyperparathyroidism in CKD. The parathyroid glands are four pea-sized glands located on the thyroid gland near the front of the neck. Although their names are similar, the thyroid and parathyroid glands are entirely different glands, each producing distinct hormones with specific functions. The parathyroid glands secrete parathyroid hormone (PTH), which is involved in bone metabolism. This hormone finds its major targets in the bone and the kidneys, and dysregulation from CKD can lead to accelerated loss of bone mineral and other bone disease (Kohlmeier et al, 1997). Fluctuations in calcium are sensed by the parathyroid glands, which secretes excess parathyroid hormone levels in an effort to increase blood levels of calcium, pulling it from the bone, increasing calcium re-absorption by the kidney, and increasing kidney production of vitamin D (Martinez et al, 1998; Owda et al, 2003; Felsenfeld et al, 2007). This excessive secretion of parathyroid hormone is referred to as secondary hyperparathyroidism (sHPT). It is a universal consequence of renal failure and is central in the treatment of CKD-disordered bone and mineral metabolism (de Boer et al., 2007; Levin et al, 2007; Zehnder et al, 2007). Increased parathyroid hormone also results in an increased calcium level in the blood and urine known as hypercalcemia.
SHPT is highly correlated with vascular calcification and cardiovascular disease, bone disease (Elder, 2002), and an increased risk of mortality in patients with CKD (Goodman et al, 2000; Raggi et al, 2002; Block et al, 1998; Block et al, 2004). Kohlmeier (1997) found that hyperparathyroidism was most severe in patients with poor vitamin K status, suggesting that a vitamin K dependent process is important for the regulation of parathyroid hormone.
· Hypercalcemia. Calcium levels typically fall within a normal range in healthy individuals, and are necessary for normal neuromuscular function. In patients with CKD, serum calcium levels fluctuate widely, due to altered mineral homeostasis and also from some of the phosphate binder therapies (Levin et al, 2009; Schlieper et al, 2016). Too much calcium in the blood causes hypercalcemia, which leads to a cascade of negative reactions on chemicals and hormones in the body, such as secondary hyperparathyroidism, renal osteodystrophy (a bone disease that occurs when kidneys fail to maintain proper levels of calcium and phosphorus in the blood), and vascular calcification that further impairs cardiac functioning (Goodman et al, 2000; London et al, 2008; Yamada et al, 2007; Bolland et al, 2008; Bacchetta et al, 2012). It appears that the vasculature is a ready location for the body to deposit and store excess calcium, and a ‘positive’ balance of calcium in the body results in it being stored in tissues and creating calcifications. High calcium concentrations act synergistically with high concentrations of phosphate and induce osteoblast-like transformation of VSMCs (Reynolds et al., 1994), which serve as the foundation for calcification to grow (Cozzolino et al, 2019; Ren et al, 2022). Shroff et al, (2008) found that in children undergoing dialysis, the calcium load was high, and their vessels showed extensive vascular smooth muscle cell loss, owing to apoptosis.
· Vitamin D deficiency. The naturally occurring form of vitamin D is known as cholecalciferol, or vitamin D3. It is a fat soluble vitamin that is available in a few foods, can be taken as a supplement, and is produced when ultraviolet rays from sunlight strike your bare skin. Vitamin D3 is inactive biologically and needs to be changed twice in the body to become active. The first change occurs in the liver, which converts D3 to calcidiol. The second change occurs in the kidney, which converts calcidiol to calcitriol, which is a potent hormone and which is the active form of vitamin D in the body. Vitamin D is known for its crucial role in mineral metabolism and bone health, as a key regulator of calcium, phosphorus, bone metabolism, and in helping regulate the immune system (Ravani et al, 2009).
Failing kidneys do not convert enough vitamin D to its active form leading to significant disturbances in the mineral system of the body. Under normal conditions, calcitriol regulates the parathyroid hormone (PTH). When calcitriol level are low, the parathyroid gland becomes enlarged, and PTH levels rise (secondary hyperparathyroidism). Elevated PTH levels then cause an increase in calcium in the blood, leading to calcifications and blockage in blood vessels. Elevated PTH levels also cause problems with bone mineralization. Patients with CKD have an exceptionally high rate of vitamin D deficiency, in both adult and pediatric patients. Some studies have found up to 78% of hemodialysis patients to be vitamin D deficient (Teng et al., 2005). In patients with CKD, vitamin D deficiency can also result from a reduction of renal mass which leads to a reduction in calcitriol, (Cannata-Andia, &, 2002). The vast majority of patients with maintenance dialysis have insufficient vitamin D storage (National Kidney Foundation, 2006; Mehrota et al, 2009; Ravani et al, 2009; Bansal et al, 2013). Additionally, the decline in vitamin D levels can be part of an adaptive response to limit the toxic effects of high phosphates.
Deficient levels of vitamin D have have been associated with weakened bones, rickets, asthma, cardiovascular disease, cognitive impairments, cancer, diabetes, hypertension and multiple sclerosis (Bischoff-Ferrari et al, 2005; Boonen et al, 2007; Cauley et al, 2008; Holick, 2008; Giovannucci et al, 2008; Pilz et al, 2008; Wang et al, 2008; Dobnig et al, 2008). In patients with CKD, low vitamin D levels are associated with increased risk of mortality (Barreto et al, 2009; Drechsler et al, 2010; Pilz et al, 2011) and deficiency is an independent indicator of early death in CKD patients (Foley et al, 1998; Gonzalez et al, 2004). Vitamin D levels are inversely correlated with the extent of vascular calcification (Watson et al., 1997). In uremic rats, low levels of vitamin D are associated with massive vascular and soft tissue calcifications (Zitterman et al, 2007).
· Other complications of CKD include:
Complications from urea buildup, which leads to azotemia and uremia. Azotemia is a condition characterized by abnormally high levels of nitrogen-containing compounds, such as urea, creatinine and other nitrogen-rich compounds in the blood. Uremia refers to the constellation of End Stage Renal Disease sequelae that include shortness of breath, nausea, vomiting, anorexia, weight loss, lethargy, encephalopathy, pericarditis (inflammation of sac around heart), seizures and coma.
Hyperkalemia is when potassium accumulates in the blood. The symptoms include malaise and potentially fatal cardiac arrhythmias.
Metabolic acidosis, is when the kidneys are not able to remove enough acid from the body. This may cause an increased excitability of cardiac and neuronal membranes (Adrogue et al, 1981), gastrointestinal problems, muscle weakness, neurological problems, kidney stones or even kidney failure. Because this condition causes the blood to reabsorb calcium from the skeleton, it can also lead to osteoporosis (brittle bones due to loss of minerals).
Decreased erythropoietin synthesis, potentially leading to anemia and fatique. Erythropoietin, or EPO, controls red blood cell production and is produced in the kidney.
Increased blood pressure due to fluid overload, and the production of vasoactive hormones created by the kidney via the rennin-angiotensin system, RAS. The rennin-angiotensin system is a hormone system that regulates blood pressure and water and fluid balance. Fluid volume overload occurs when the circulating volume of blood is excessive. This fluid overload can increase blood pressure which then increases the risk of developing hypertension and/or suffering from congestive heart failure.
--Abnormalities in bone turnover, mineralization, volume, linear growth, or strength
Bone is a dynamic tissue, which constantly undergoes growth and remodeling. Bone forms through mineralization of cartilage, a process called ossification. Mature bone tissue is removed from the skeleton, a process called bone resorption. During resorption, the minerals are released resulting in a transfer of calcium from bone fluid to the blood, part of regulating calcium balance in the body. These dynamic processes also respond to the functional demands of daily activity, hormonal stress, and to micro-damage and injuries, allowing for maintenance and repair of the skeleton. These processes also control the reshaping or replacement of bone following injuries or stress from normal activity. In the first year of life almost 100% of the skeleton is replaced. In adults, remodeling proceeds at about 10% a year (WheelessOnline.com, captured 4-2-2013).
Disorders and dysregulation of mineral metabolism and endocrine function result in skeletal complications and renal bone disease, where there is abnormal bone turnover, abnormal mineralization, and linear growth, as well as extraskeletal complications where body tissues and vasculature acquire calcification rather than the skeleton (KDIGO, 2009; Moe et al, 2009). This occurs almost universally in patients with CKD stages 3-5.
The bone-disease component of CKD–MBD is a serious complication which may result in fractures (Ensrud et al, 2007), bone pain, osteoporosis, deformities in growing children, reduced growth velocity, and abnormal height (Craver et al, 2007). Dialysis patients in their forties have a relative risk of hip fracture that is 80-fold higher than that of age-matched and sex-matched control subjects. Furthermore, hip fracture in dialysis patients is associated with a doubling of the mortality observed in hip fractures for nondialysis patients (Coco M and Rush H, 2000; Alem et al, 2000). Analyses have found that race, and low or very high PTH levels are risk factors for hip fracture (Ensrud et al, 2007; LaCroix, 2008; Neer et al, 2001; Coco & Rush, 2000). Complications of hip fractures include bleeding, infection, loss of independence, and increased mortality. Vertebral fractures lead to height loss, reduced pulmonary function, gastrointestinal reflux, and chronic disability. In children, growth retardation and skeletal deformities reduce quality of life.
The mineral dysregulation that creates renal bone disease, also contributes to cardiovascular disease (Mizobuchi et al, 2009; Cozzilino et al, 2018. Rodriguez-Garcia (et al, 2009) have demonstrated a positive, significant correlation between vertebral fractures and vascular calcification in the dialysis population. They found in women with vertebral fractures, a correlation between vascular calcification and mortality and between vertebral fractures and mortality. Typically in people with CKD, bone mineral content decreases with the progression of CKD, while vascular calcifications increase (Klawansky et al, 2003). And research suggests that bone turnover may be directly linked to cardiovascular disease, as the low turnover, leads to calcium-phosphorus being deposited into vascular tissues, resulting in cardiovascular disease and heightened mortality (US Renal Data System, 2007; Coresh et al, 2007).
--Vascular or other soft tissue calcification.
The extensive cardiovascular risk for patients with kidney disease has been observed since the early days of dialysis (Tatler et al., 1973; Ibels et al., 1974). Most patients with CKD-MBD die from cardiovascular disease, not kidney failure. The cardiovascular complications are wide and varied, and it is the leading cause of death for people with chronic kidney disease, at a rate 20% higher than that of the general population, even after adjustment for age, gender, race and the presence of diabetes (Foley et al, 1998; Muntner et al, 2002; Levey et al, 2007; Schroff et al, 2007; Collins, 2003; Go et al., 2004; Manjunath et al, 2003; Ninomiya et al, 2005; Go, 2016).
The research has extensively documented the various sorts of cardiovascular disease that is associated with CKD (USRDS, 1998; Goodman et al., 2000; Block et al. 2004; Quinibi, 2005; Ketteler & Giachelli, 2006; Cozzolino et al, 2019). The rate of cardiac failure among patients with advanced CKD is 40% (Foley et al, 1998). Cardiovascular disease predicts a faster decline in the GFR (Go et al, 2004; Schiffrin et al, 2007) and as the GFR declines, obstructive CAD increases (Nakano, et al, 2010; Chonchol, 2008). A higher incidence rate of myocardial infarction has been documented repeatedly in patients with CKD (Muntner et al., 2002; Ninomiya et al, 2005; Rubenstein et al, 2000; Beddhu et al, 2002; Fried et al., 2003). Sudden Cardiac Death is common and accounts for about 25% of patient deaths among those on dialysis. After sudden cardiac arrest, survival is universally poor with a six months survival of 3-11 % (Pun et al, 2007; Lai et al, 1999; Moss et al, 1992; Herzog et al, 2011).
Vascular calcification occurs when calcium accumulates in the intima and/or media layers of the vessel wall once it has become mineralized (Vliegenthart et al, 2005). Both types of calcification are associated with an increased risk of myocardial infarction (Lehto et al, 1996) and cardiovascular mortality (London et al., 2003). Over 70% of dialysis patients have significant coronary artery and aortic calcification, 50% of dialysis patients have calcified valves, 50% of dialysis patients have significant coronary calcification, and 50% of cardiovascular deaths that may be associated with abnormal tissue calcification in patients treated with dialysis (Raggi et al, 2002; Wang et al, 2003; Goodman et al., 2000; Moe, 2006; Sigrist, 2006; McCullough et al., 2008; Ix, et al., 2007; Amann, 2008). Vascular calcification is so significant in CKD patients that the severity of coronary arterial calcification (CAD) and its progression are predictors of future mortality risk for CKD patients (Okuno et al, 2007; Ketteler, Rothe et al., 2011), particularly for patients who are in Stage 5 – End Stage Renal Disease (London et al, 2003; Blacher et al., 2001; Wang et al, 2003; Adragao et al, 2004; Block et al, 2007; Schlieper et al, 2008) even when under the age of thirty (Braun et al., 1996; Qunibi, 2005; Goodman et al, 2000; Oh et al, 2002; Blacher et al, 2001; Giachelli, 2004). Ultrasonographic studies have shown a much higher prevalence of calcified plaques in CKD patients than in age-matched controls (Savage et al, 1998). Matsuoka (et al., 2004) showed that the five year survival rate of patients with a high coronary calcium score was 30% lower compared to patients with a score below 200, clearly establishing the prognostic relevance of coronary calcification in dialyzed patients. Peripheral artery disease is common in about 24% of CKD patients (O’Hare, et al, 2004).
CKD patients are particularly prone to medial calcification, known as Monckeberg’s sclerosis, which is a form of vessel hardening, where calcium deposits are found in the muscular middle layer of the walls of arteries, the tunica media. Artery walls are built by layers of vascular smooth muscle cells (VSMCs) separated by the elastic internal laminas (Abedin et al, 2004). The VSMC’s in the vessel wall transform to osteoblast-like cells, which precedes calcification and is similar to the mechanisms underlying bone formation (Wallin et al., 2004). It occurs in arteries of any size, including small arteries where atherosclerosis does not occur (Lachmann et al, 1977; Chowdhury et al, 2004). Medial calcification can contribute to left ventricular hypertrophy, dysfunction and failure and often leads to arterial stiffening, elevated systolic and pulse pressure, increased pulse wave velocity, and increased cardiac workload (Amann, 2008; Schwarz et al, 2000; Gross et al, 2007; Moe et al, 2003; Ibels et al, 1979; London et al, 2005). Medial calcification is predictive of cardiovascular and all-cause mortality in CKD patients (London et al, 2003; Giachelli, Speer et al. 2005; Zoungas et al, 2007).
This early vascular aging (EVA) is a hallmark of senescence, or deterioration, as well as a strong predictor of cardiovascular morbidity and mortality in the CKD population (Cunha et al, 2017). Growing evidence shows that vitamin K plays a crucial role and vitamin K supplementation may provide a novel treatment target for EVA (Dai et al, 2020).
Calcification of the intimal layer is reflective of atherosclerotic heart disease and is independently predictive of future cardiovascular events and overall mortality. (Thompson & Partridge, 2004). Intimal calcification occurs in areas devoid of smooth muscle cells, and is usually limited to the large and medium sized conduit arteries (Moore, 1996). It increases the risk of plaque erosion and rupture (Vliegenthart et al., 2002; Virmani et al, 2002; London, 2003; London et al, 2004; Abedin et al, 2004; Sosnov et al, 2006). Nephrosclerosis, the renal expression of intimal arteriosclerosis, is the most frequent renal disease underlying the high prevalence of chronic kidney disease in the general population (London,et al, 2011).
Arterial stiffness is measured as aortic pulse wave velocity (PWV), and PWV represents one of the strongest predictors of cardiovascular mortality and cardiovascular outcomes in dialysis patients (Blacher, et al, 1999; Pannier et al, 2005; Nemczik, et al, 2012). Arterial stiffness tends to increase in parallel with the progression of kidney function decline (Wang et al., 2005; Pannier et al., 2005; Kimoto et al., 2006). In this population, arterial rigidity is typically associated with calcifications, and Pulse Wave Velocity in ESRD reaches the highest level observed in human diseases (Blacher et al., 1999).
Calcific uremic arteriopathy, also known as calciphylaxis, is unique to patients with ESRD and classically manifests as calcification of cutaneous and subcutaneous arteries with occlusive intimal proliferation and subsequent fat necrosis (Danziger, 2008).
It has been determined that the uremic environment created by kidney failure accelerates the progression of atherosclerosis (Braun et al., 1996; London et al., 2003). (Once calcification is established, it follows a progressive and accelerated course during CKD (Sigrist, 2007; Russo, 2007; Bursztyn, 2003; Kronenberg 2003; Chertow 2002; Raggi, 2004; Block 2005; Suelack 2001).
Other cardiac difficulties in CKD involve pressure overload, volume overload and non-hemodynamic factors that alter the myocardium. Pressure overload is the result of long standing hypertension and vascular stiffness. These can result in congestive heart failure (Bagshaw et al., 2010), ischemic heart disease, cardiac arrhythmias (usually A-fib), and valvular calcification (Ronco et al, 2010; Schrier, 2007; Das et al., 2006). The progression of CKD is often accompanied by Left Ventricular Hypertrophy and diastolic dysfunction (McCullough et al., 2004).
It was widely believed that cardiovascular disease was the result of a passive accumulation of mineral buildup. It is now understood that cardiovascular disease and its vascular calcification burden is an actively regulated process of tissue bio-mineralization that may be possible to manage. In the case of kidney disease, it is now understood that the wide prevalence of cardiovascular disease is a direct reflection of the mineral dysregulation of the uremic environment (Shioi et al, 2009; Westenfeld et al., 2007), which confers additional risk factors for coronary vascular disease. The mineral disorder of CKD dysregulates calcification inhibitors and promotes calcification inducers (Shio et al, 2009; Westenfeld et al, 2007; Drueke & Massy, 2010; Ivanovski et al, 2005). Uremia-associated risk factors like chronic inflammation, hyperphosphatemia, vitamin D deficiency, and an increased calcium load promote calcification, while deficiencies of calcium inhibitors such as vitamin K are helpless to stop it (Goodman et al, 2000; Ganesh et al, 2001; Block et al, 2004; Ebert et al, 2020). And a widely used treatment in CKD is warfain, which interferes with calcium inhibitors, and is known to promote vascular and other soft tissue calcification, contributing to cardiovascular disease (Thompson & Towler, 2012).
For some, chronic kidney disease is a clinical model of premature aging characterized by cardiovascular disease, persistent uremic inflammation, osteoporosis muscle wasting and frailty (Stenvinkel et al, 2013; Shanahan et al, 2013; Kooman et al, 2014). The accelerated aging process mediated by vascular calcification is a hallmark of aging, as well as a strong predictor of cardiovascular morbidity and mortality in a CKD population (Dai et al, 2020). Growing evidence shows that vitamin K plays a crucial role in counteracting oxidative stress, DNA damage, senescence and inflammaging (Shea et al, 2014; Harshman & Shea, 2016; Franceschi et al, 2018; Dihingia et al, 2018; Dai et al, 2020)
Treatment of CKD-MBD
-CALCIFICATION INDUCERS
There is no cure for chronic kidney disease. It is not reversible. Kidney function, once lost due to a disease process, does not return. There is only management of the risk factors in order to slow down the progression of the disease and its profound multi-system effects. Dialysis or transplantation are treatments of last resort, and dialysis does not replace the function of the kidneys. The risk factors begin early in the course of the disease and contribute to the cardiovascular disease and calcification that is the leading cause of death (Sigrist et al, 2007). The goal of treatment now is to manage the mineral dysregulation as a whole, while specifically intervening upon the systemic and local factors that can inhibit vascular calcification (KDIGO, 2009; Razzaque et al, 2005; Schiffrin et al, 2007; Westenfeld et al, 2007; O’Neill & Lomashvili, 2010). The focus of treatment has been shifting to two other pathways. One, being a consideration of inducers of calcification and finding a way to restrain them, and the other pathway being a consideration of the natural calcium inhibitors and finding a way to promote them, such as vitamin K (Koos et al, 2005; Ketteler et al, 2006).
The following discussion reviews the leading inducers of calcification within CKD and some of the treatments that have been attempted over the years. Included in this discussion is vitamin K deficiency, which is being recognized as a symptom in its own right, as well as holding the potential to be an important treatment, given that it is key to the regulation of calcium in the body.
· Hyperphosphatemia. Over the past 40 years, hyperphosphatemia has been a central therapeutic issue in advanced CKD. During the last decade, research has established the role of hyperphosphataemia as a major player in promoting cardiovascular (CV) calcification and an important predictor of mortality in chronic kidney disease (CKD) patients (Block et al., 1998; Ganesh et al, 2001; Block et al, 2004; Young et al, 2005; Slinin et al, 2005). Mainstays of the treatment have been the reduction of dietary phosphorus, use of phosphate binders to capture phosphate within the colon and excrete it from the body, and optimized phosphorus removal via dialysis, and unfortunately, none of those were able to accomplish the job (Heinrich, 2008; Kalantar-zadeh et al, 2010
However, the view on phosphate binders have undergone an evolution. In the 1970s, aluminum salts were the standard treatment and were excellent phosphate binders. However, they resulted in a toxic accumulation of aluminium in the blood, bone, brain, and nerve tissues (Andreoli et al., 1984; Jespersen et al., 1991; Lerner et al, 1986; Alfrey et al, 1976) and were essentially discontinued.
In the 1990s, calcium carbonate and calcium acetate became the standard phosphate binder treatment (Ritz, 2004; Cozzolino et al. 2010) and were somewhat effective, however, it has become clear that calcium-based binders significantly increase the calcium load in the body, and contribute to the calcification that is the leading cause of death (London, 2008; Alfrey et al., 1976). In the past, practitioners believed that the calcification in predialysis and dialysis patients was due to the supersaturation of calcium from the kidney dysfunction(Chen, et al, 2006; Schwarz et al, 2000; Russo et al., 2007). Subsequently, it has been established that calcium based phosphate binders enhance the progression of vascular calcification both directly and indirectly, first by increasing the systemic calcium load, and then by reducing the calcium storage in the bone, with there being a significant reduction in thoracic vertebral bone density (Chertow et al., 2002; Cozzolino et al., 2010; Schroff et al., 2010) with a concomitant increase in coronary calcification score (Rostand & Drueke, 1999; Guerin et al, 2000; Goodman et al, 2000; Raggi et al, 2005), an increase in fatal vascular events, a poor outcome (Bleyer al, 1999; Ganesh et al., 2001; Branley, 2006), and bone disease (Block et al., 2012). Even when the calcium dosages were administered under strict surveillance, they have been associated with the worsening of coronary artery calcium scores (Chertow et al, 2002; Barreto et al, 2008; Quinibi et al, 2008; Hill et al, 2013), and an acceleration of the calcification (Block et al, 2005).
The search continues to find a phosphate binder that would not increase the calcium load, and the superiority of one compound over another has not been established. Sevelamer hydrochloride (SH) was developed as the first phosphate binder that contains neither calcium nor aluminium (Chertow et al., 1997), and lanthanum carbonate has emerged as a possible alternative, but the results are inconclusive (Asmus et al, 2005; Block et al, 2005; Russo et al, 2007; Quinibi et al, 2008; Suki et al, 2007; Hutchison et al., 2009). And recent findings raise the concern that sevelamer may reduce the absorption of vitamin K (Fusaro et al, 2019). An in vitro study to determine the absorption of vitamins K, B6, B12, C, and folic acid showed that sevelamer had almost complete absorption of vitamin K, C, and folic acid (Takagi et al, 2010; Jansz et al, 2018), an outcome which would further inhibit the calcium regulation properties of vitamin K and heighten the calcification risks for CKD patients (Cozzollino et al., 2012). Neradova (et al 2017) found that two out of five commonly used binders interfered with the bioavailability of vitamin K. A study of 387 patients on hemodialysis showed that Sevelamer interfered with MK4 absorption (Fusaro et al, 2020).
· Secondary Hyperparathyroidism. The ultimate goals of treating sHPT are to normalize mineral metabolism, prevent bone disease, and to prevent calcifications. Treatment focuses on minimizing hyperphosphatemia and hypocalcemia without producing hypercalcemia and overly suppressing the parathyroid hormone (Tomasello, 2008). Achieving control of the mineral metabolismin sHPT is difficult and is attempted with combination therapy that includes oral phosphate binders, active vitamin D compounds (calcitrol), calcimimetics, and adjusting the calcium concentration in the dialysate, any and all of which could potentially affect vascular calcification. Consequently, a significant amount of research has been directed at optimizing these therapies to minimize vascular calcification.
Early research indicates that vitamin K supplements may positively impact sHPT. Animal trials investigating the effect of menaquinones (vitamin K2) found that, among other effects, it delayed an increase in PTH serum levels, stimulated renal calcium reabsorption, and improved bone health (Iwamoto, et al, 2003). Nakashima et al, (2004) investigated the influence of vitamin K2 on hemodialysis patient with low serum parathyroid hormone levels measured with bone metabolism markers. After administration of 45 mg/day of MK4, bone remodeling was improved in patients with CKD. Given the evidence that vitamin K improves bone health and prevents calcifications, it would seem logical to pursue and advocate an inexpensive and non-toxic vitamin K alternative for parathyroid hormone support, rather than a more expensive and risker approach (Iwamoto et al., 2001).
· Hypercalcemia. An excess of calcium has a profound effect on the nervous system, but more significantly, excess calcium in the body is associated with the cardiovascular disease and calcification that is the leading cause of death in CKD (Solomon et al., 1994). Measures undertaken to treat hypercalcemia may be divided into nonspecific therapies aimed mainly at increasing the excretion of calcium in the urine and decreasing intestinal absorption of calcium, those specifically aimed at slowing bone resorption, those directly removing calcium from circulation, and those aimed at controlling the underlying diseases causing hypercalcemia. Often initial therapy involve fluids to rehydrate, diuretic medications to help flush excess calcium, IV biphosphonates are given to prevent bone breakdown, corticosteroids to help counter the effects of too much vitamin D in the blood, and hemodialysis to remove excess waste and calcium. Drugs used to treat other conditions in CKD can cause hypercalcemia. Reducing or stopping these drugs, such as phosphate binders, or calcitrol is a treatment strategy for managing hypercalcemia. Dialysis is also used as a treatment for hypercalcemia in patients with kidney failure.
What is most interesting is that the key regulator of calcium, vitamin K, has yet to be researched as a possible treatment agent for hypercalcemia (Fusaro et al, 2011). Given that Vitamin K activates proteins in the body that regulate calcium through a carboxylation process, making both matrix gla protein (cMGP) and bone gla protein (cBGP) biologically active, and that cMGP inhibits vascular calcifications, while cBGP has an important role for a proper mineralization process and bone health, further investigating vitamin K and its effect could be worthwhile (Roumeliotis et al, 2022).
· Vitamin D levels. The impaired ability of the diseased kidney to convert vitamin D into its active form, 1α,25(OH)2D3, often leads to a vitamin D deficiency, which in turn can lead to secondary hyperparathyroidism, weak bones, and a compromised immune system. Traditional treatments for vitamin D deficiency in CKD usually consists of vitamin D2, or calcitriol (D3) given as a capsule of 50,000 IUs once a month, titrated to maintain iPTH, calcium, phosphorus, and Ca x P within KDOQI target ranges. However, calcitriol increases serum calcium levels and suppresses parathyroid hormone (PTH) release. While this treatment addresses the secondary hyperparathyroidism, the resulting increase in serum calcium levels (hyperecalcemia) together with increased serum phosphate (hyperphosphatemia) promotes mineralization in the vasculature (Stim et al, 1995; Sprague et al, 2003; Jara et al, 2002; Jono et al., 1998), the formation of fetuin-A mineral complexes (Price et al., 2004) and the local transformation of VSMCs into osteoblast-like, calcified cells (Jono et al., 1998; Tukaj et al, 2000; Rebsamen et al, 2002; Zebger et al, 2011; Shioi et al, 2000; Norman et al, 2005). It appears that there is a narrow range of vitamin D levels in which vascular function is optimized, and levels below or above this range can significantly increase the risk for cardiovascular disease (Hsu et al, 2008). In adult patients with CKD, the severity and progression of vascular calcification correlates with circulating vitamin D levels (Garcia-Canton et al, 2011; Goldsmith et al, 1997).
Vitamin D and vitamin K have overlapping metabolic and physiologic roles involving skeletal and vascular health, and it is believed they have a synergy of action, however there are few studies that have examined this synergy. Vitamin D helps you absorb the calcium you need, and it appears that vitamin K directs that calcium to your skeleton, rather than your vasculature. In one study, postmenopausal women with osteopenia and osteoporosis were given Mk4, D3, or MK4 and D3. Calcium was not supplemented. After two years, bone mineral density (BMD) increased in the MK4 and D3 group the most when compared to the control group, or when compared to the groups receiving either MK4 or D3 alone. This suggest that MK4 and D3 might have a synergistic benefit for bone health, perhaps the nexus being the vitamin K dependent protein, osteocalcin. The synthesis of osteocalcin by osteoblasts is regulated by the vitamin D (Ushiroyama et al, 2002). Vitamin K2 promotes normal vitamin D-stimulated osteocalcin accumulation and mineralization processes (Koshihara et al, 1996), and D3 has been found to enhance the reductive recycling of MK4 (Miyake et al, 2001). One study found that healthy older women who took supplements of vitamin K1 together with supplements of calcium plus moderate vitamin D3, enhanced their BMD, and increased serum levels of carboxylated osteocalcin (Bolton-Smith et al, 2007).
Vitamin D and vitamin K overlap in other areas, and seem to both play a role with inflammation (Clowes et al, 2005; Libby, 2006) and have antioxidant power to protect living cells against attack (Li et al, 2009; Chen et al, 2003). Further exploration of the synergy between vitamin K and vitamin D might be fruitful directions for additional research (Hou et al, 2018).
· Vitamin K Deficiency. Newly identified as a treatment focus in CKD-BMD is vitamin K and its sufficiency. Vitamin K refers to a family of structurally related, fat-soluble vitamins occurring as phylloquinone (vitamin K1) or a series of vitamins commonly termed menaquinones (vitamin K2), that are known for their role in blood clotting. The different K vitamins have different chemical structures and seem to be utilized differently by the body. All forms of vitamin K serve as a cofactor for the carboxylation of K dependent proteins which help bind calcium. Vitamin K1 (phylloquinone) is the primary form of vitamin K found in the diet and the major form of vitamin K found in the liver. K2 is an umbrella term for the family of menaquinones. The menaquinones are longer-chained, have longer half-lives and are better absorbed, typically in extra hepatic tissues, such as the arterial wall, pancreas and testes. Specifically, menaquinone 4 (MK4) is a K2 vitamin that is present in the diet in only very small quantities, but it is the major form found in extra-hepatic tissues such as the vasculature, brain, and reproductive organs. There is evidence that K1 is converted to Mk-4 directly within tissues, (Thijssen et al, 1996; Davidson et al, 1998; Spronk et al, 2003; Thijssen et al, 2006; Okano et al, 2008; Al Rajabi et al, 2012). MK7 is more difficult to come by and is not produced by human tissue.
Animal and molecular studies have demonstrated that vitamin K is vital to the healthy functioning of many bodily tissues and organs (Schurgers et al., 2008). These tissues contain proteins that require sufficient amounts of vitamin K, in order to be carboxylated and then biologically active. Carboxylation is the chemical modification of proteins triggered by the presence of vitamin K. These proteins are both local and circulating, and some, such as osteocalcin and matrix Gla protin were identified as critical regulators of vascular calcification (Mazzini, et al, 2006; Price et al, 1985; Ferland, 1998: Tsaioun, 1999, Maree, 2007).
Animal and molecular studies have demonstrated that vitamin K is involved in the development and progression of vascular calcification, as mediated by the carboxylation of matrix gla protein (MGP) (Shea et al, 2007; Geleijnse et al, 2004; Schurgers et al, 2008; Price et al, 1998; Schurgers et al, 2001; Schurgers et al, 2007; Wallin et al, 2008). When vitamin K is deficient, the proteins like MGP are uncarboxylated and inactive, and their physiological function is impaired (Rennenberg et al, 2010; Zak-Golab, 2011). Uncarboxylated proteins may continue to be circulated, but are ineffective (Abedin et al., 2004). This is associated with increased vascular calcification, both in populations with and without renal disease (Murshed et al, 2004; Schurgers et al, 2005). When those proteins have been deleted through genetic modification with rodents, and were unavailable to accept vitamin K, the animals died quickly due to massive calcification of the arterial system (Luo et al, 1997).
Less than optimal vitamin K status in otherwise healthy populations may be much more common than previously thought, particularly in the elderly (Knapen et al, 1989; Sadowski et al, 1989; Duquette et al, 1994; Cozzolino et al, 2020). And research has established that the CKD population is no different (Wallin & Schurger, 2008). Low or insufficient vitamin K levels have been identified as a risk factor for people with CKD-BMD (Schlieper et al, 2011; Schurgers, Barreto et al, 2010; Elliott et al, 2014). There is a high prevalence of subclinical vitamin K deficiency in patients at all stages of kidney failure, ranging from 60-90% (Kohlmeier et al, 1997; Malyszyko et al, 2002; Pilkey et al, 2007; Garland et al, 2008; Holden et al. 2008; Nerlander et al, 2009; Holden et al, 2010; Schlieper et al, 2011; Cranenburg et al, 2012; Westenfeld et al, 2012; Voong et al, 2013; Stenvinkel et al, 2017; Cozzolino et al, 2019; Fusaro et al, 2020). And the deficiency of vitamin K for CKD patients may also create a risk factor for their bone health (Evenepoel et al, 2019). In one study, one out of four hemodialysis patients had a serum phylloquinone concentration that was at least two standard deviations below the mean of healthy adults (Saupe et al, 1993). There several clinical trials underway looking at the effects of vitamin K on markers of vascular calcification in hemodyalisis patients (Caluwé R, et al, 2020; Haroon et al, 2020).
There are many possible reasons for the low vitamin K levels in CKD (Caluwe et al, 2020). Phosphate binders, proton-pump inhibitors and antibiotics are frequently prescribed to dialysis patients and may negatively influence vitamin K bioavailability through various mechanisms (Jansz et al, 2018). Dietary restrictions can lead to inadequate intake, dysbiosis due to the uremic condition leading to decreased vitamin K production by microbiota, and hemodialysis associated deficits (Cranenburg et al, 2012; Fusaro et al, 2017). The gamma carboxylase activity is decreased in an experimental uremic milieu. The pro-calcifying uremic environment may exhaust vitamin K stores. Vitamin K antagonists (VKA) negatively impact vitamin K status in bone and arteries. Some believe that poor oral intake of vitamin K is the main cause of the deficiency (Wyskida, 2015, Fusaro, et al, 2017), and a recent study illustrated the low dietary intake as the primary explanation (Wikström et al, 2020). The next theory was the use of phosphorus binders (Fusaro et al, 2019; Jansz et al, 2018). There several clinical trials underway looking at the effects of vitamin K on markers of vascular calcification in hemodyalisis patients (Caluwé R, et al, 2020).
And there appear to be notable sex and age differences in tissue vitamin K levels (Harshman et al, 2016; Huber et al 1999). Harshman studied the vitamin K metabolome in mice exposed to vitamin K deficient diets. They found significant sex-specific differences in all tissues for measurements of K1 , MK4, and various other long-chain MKs. Female rats had significantly higher levels of K1 and MK4 in all tissues.
Additionally, CKD patients have been found to have an increased amount of inactive MGP circulating (Schurgers et al., 2010), reflecting a vitamin K deficiency. Pilkey et al, (2007) revealed abnormal phylloquinone and undercarboxylated osteocalcin concentrations in 29% and 93% of the hemodialyzed subjects, respectively. Holden et al. (2008) documented frequent vitamin K deficiency; abnormal phylloquinone levels were present in 23.8% of patients, with high percentages (>20%) of undercarboxylated osteocalcin present in all subjects studied. In a comprehensive study, Holden (et al., 2010) measured vitamin K and D status via dietary intake, plasma phylloquinone levels, serum percent uncarboxylated osteocalcin (%ucOC), proteins induced by vitamin K absence (Pivka II), VKOR, apolipoprotein E genotype, and plasma vitamin D levels in 172 subjects with stage 3 to stage 5 CKD. The mean vitamin K1 intake was 130 ug/d. They found that sub-clinically, a systemic vitamin K deficiency was present, with 6% deficient in phylloquinone, 60% had increased levels of serum percent uncarboxylated osteocalcin meaning low vitamin K, and 94% had increased PIVKA-II (proteins induced by vitamin K absence), whereas 58.3% and 8.6% had vitamin D insufficiency and deficiency, respectively. Patients with proteinuria (excess proteins in the urine) had both a suboptimal vitamin D status as well as worse peripheral vitamin K status. (Holden et al., 2010). Circulating levels of ucOC has been proposed as a marker of atherosclerosis in non-dialysis patients with CKD (Zhang et al, 2015).
Dephospho-carboxylated Matrix Gla Protein (dp)cMGP is thought to be a sensitive marker of vitamin K deficiency (Boxma et al, 2012). Cranenburg et al, (2010) reports that (dp)ucMGP (dephospho-uncarboxylated Matrix Gla Protein) deficiency is higher among patients with diseases characterized by vascular calcification, including CKD, and (dp)ucMGP was found to be positively associated with aortic calcium score in 107 patients with CKD (Schurgers et al., 2010). An alternate monoclonal-antibody ELISA that measures total-ucMGP (whether or not it is phosphorylated) is also available, and this measure of total ucMGP was reported to be inversely associated with calcification in a small sample of hemodialysis patients (n = 40) (Cranenburg et al, 2009). In a supplementation trial that will be discussed later, Westenfeld also established that hemodialysis patients had a functional vitamin K deficiency with a 4.5-fold higher dephosphorylated-uncarboxylated MGP (dp-ucMGP) and 8.4-fold higher uncarboxylated osteocalcin (ucOC) levels compared with controls. PIVKA-II levels were elevated in 49 hemodialysis patients (Westenfeld et al, 2012). Jansz et al (2018) found that dp-ucMGP was lower (or improved) after a transplant and recommended that vitamin K status or supplements be considered for patients with CKD. Kidney transplant recipients continue to have a high mortality and graft risk and are often low in vitamin D and K. When vitamins D and K are both low, the risk of mortality increases following a transplant. Additionally, a low vitamin K status when vitamin D is administered increased the risk even more, meaning if vitamin D is given, then vitamin K should also be given (Van Ballegooijen et al, 2020).
Undercarboxylated prothrombin, also known as proteins induced in vitamin K absence or antagonism—factor II (PIVKA-II), can be measured by commercial assays. PIVKA-II levels are not influenced by kidney function and can thus be used to assess hepatic vitamin K status in CKD (Kato et al, 2002). A level of 2 nmol/L is generally accepted as a cut-off for vitamin K deficiency (Elliott et al, 2014). PIVKA-II responds to dietary vitamin K depletion, warfarin use and supplementation with both phylloquinone and MK-4.
Moreover, cohort studies revealed that the plasma dp-ucMGP levels increased with the progression of CKD, especially in patients with CKD stages 3-5 (Thanratnopkoon et al, 2018; Jaminon et al, 2020). Other studies have evaluated the risk of increasing dp-ucMGP levels on renal function. Jacques (et al, 2019) found that dp-ucMGP levels correlated with the Renal Resistive Index, cardiovascular risk factors and renal function. The Nephrotic Syndrome Study Network cohort study reported that renal MGP expression increased in five out of six rats that underwent nephrectomy (Miyata et al, 2018). This evidence explains the renoprotective role of MGP and further indicate that vitamin K exerts a beneficial effect on renal function. And dp-ucMGP was associated with increased mortality risk in people with advanced chronic kidney disease (Dai et al, 2021). Others feel that dp-ucMGP may serve as a modifiable risk factor for CKD (Groothof et al, 2021).
Patients undergoing dialysis have been found to be deficient in vitamin K (Nagata et al, 2014). Stankowiak-Kulpa and colleagues (2011) evaluated vitamin K status in 28 patients with CKD who are treated with peritoneal dialysis. Dialysis vintage ranged from 3 to 89 months. Vitamin K status was assessed using PIVKA-II. In addition, total protein and albumin levels, total cholesterol, LDL cholesterol, triglyceride, calcium, urea and creatinine concentrations were determined. PIVKA-II concentrations were abnormal in 46.4% (13) subjects. BMI values, both total and LDL cholesterol concentrations were significantly higher in patients with a deficiency, than those without vitamin K deficiency. Their results suggest that peritoneally dialyzed patients with CKD are at high risk of subclinical vitamin K deficiency as defined by the specific and sensitive marker, PIVKA-II. Fusaro (et al, 2011) found that substantial proportions of patients were deficient in MK4, K1, and MK7, and that these deficiencies were predictors for other complications, such as vertebral fractures and aortic calcifications. Cranenburg,(et al., 2012) measured vitamin K1 and K2 intake and their status in 40 hemodialysis patients. They found the intake was low, especially on days of dialysis and the weekend and not surprisingly: they also found that non-carboxylated bone and coagulation proteins were elevated in 33 of the hemodialysis patients, indicating subclinical hepatic vitamin K deficiency. Westenfeld et al (2012) found that hemodialysis patients had 4.5-fold higher dephosphorylated-uncarboxylated MGP and 8.4-fold higher uncarboxylated osteocalcin levels compared with controls, meaning that they lacked sufficient vitamin K to carboxylate the MGP and osteocalcin. PIVKA-II levels were elevated in 49 hemodialysis patients, also reflecting low vitamin K status. Wyskida (et al, 2015) found MK4 concentrations in hemodialysis patients were low, and likely attributed to diminished meat consumption and reduced K1 conversion, and then in 2016, they established that there was a functional vitamin K1 deficiency in hemodialysis patients in Poland (Wyskida et al, 2016. Yet, one more study confirming that most hemodialysis patients have a functional vitamin K deficiency (de Oliveira et al, 2020).
There is growing evidence to suggest that a defect in the carboxylation process contributes to the accumulation of under-carboxylated VKDPs and reflects an overall impact of uremia on vitamin K metabolism (Westenfeld et al, 2012). Patients with chronic kidney disease appear to consume an adequate amount of vitamin K yet exhibit very high levels of under-carboxylated VKDPs in the circulation. In the general population, the under-carboxylated fraction of a VKDP is thought to reflect deficiency at the site of production of that protein. Pre-clinical studies indicate an impact of uremia on tissue levels of vitamin K and on the activity of GGCX, the key enzyme involved in activation of VKDPs (Kaesler et al, 2014; Turner et al, 2018). These findings suggest a direct impact of CKD on vitamin K recycling and the carboxylation process. And there are published and unpublished studies to indicate that the apparent carboxylation defect in hemodialysis patients can be corrected with both vitamin K1 and vitamin K2 supplementation. patients with CKD are a clinical group at high risk for low circulating levels of vitamin K1 and elevated levels of dysfunctional VKDPs.
And the deficiency of vitamin K for CKD patients may also create a risk factor for their bone health (Evenepoel et al, 2019). There is a large body of research that has established the relationship between vitamin K and bone health. And since bone disease is a central aspect of CKD-BMD, supplementation with vitamin K could also help with bone health (Fusaro et al, 2022; see http://www.k-vitamins.com/index.php?page=Bone). Some believe that of the vitamin K family, the menaquinones, specifically MK4 may offer the most promise, and that the menaquinones seem to reduce bone resorption by stimulating osteoprotegerin production (Sasaki et al, 2005).
Warfarin.
Warfarin is one of the most frequently prescribed drugs to control blood clots and is used regularly in the treatment of CKD for the prevention of blood clots, atrial fibrillation, and occasionally as a blood thinner for ease of dialysis hookups. The prevalence of warfarin prescription to dialysis patients varies across nations from <5% in Germany, Spain, and Japan to as high as 26% and 37% in the US and Canada, respectively (Miller et al, 2006; Wizemann et al, 2010). Warfarin is also known as Vitamin K antagonist (VKA), as it blocks the Vitamin K epoxide reductase enzyme (VKOR), that results in the regular coagulation of blood that vitamin K is necessary for. (This is what made warfarin effective originally, as a rat poison). Unfortunately, warfarin and any other VKA treatments may have undesired side-effects, as we now know that a number of proteins outside of the coagulation system require vitamin K to be come carboxylated and biologically active, including the proteins that regulate calcification (Price et al, 1998; D'Andrea et al, 2008; Chatrou et al, 2011). Warfarin use is also associated with arterial stiffness (Mac-Way et al, 2014). When it antagonizes the vitamin K cycle, it also prevents the carboxylation of vitamin K dependent proteins such as MGP, which is the best known inhibitor of calcification (Price et al, 1998; D'Andrea et al, 2008) and hence becomes a contributor to calcification (Chatrou et al, 2011).
There is an abundance of research indicating that warfarin use contributes to vascular calcification. Animal studies suggest that VKA treatment causes medial calcification similar to Mönckeberg’s sclerosis (Price et al, 1998; Spronk et al, 2003; Essalihi et al, 2003). Rats treated with warfarin developed focal calcification of the elastic lamellae of the aorta and aortic valve after only 2 weeks; after 5 weeks, calcification was evident on radiographs (Price et al, 1998). McCabe and colleagues (McCabe et al, 2013) showed that giving vitamin K antagonists (VKA) or using low vitamin K2 intake in rats with CKD markedly increases the degree of vascular calcification. Schurgers (2013) demonstrated for the first time that warfarin increases plaque calcification in the apoE−/− model with rats and concluded that warfarin affects plaque calcification by inhibiting post-translational γ-carboxylation of MGP. This is in agreement with previous in vitro studies demonstrating that warfarin treatment causes ucMGP production by VSMCs (Schurgers et al, 2007).
A high number of CKD patients receive oral anticoagulants (vitamin K antagonists; VKA). VKAs not only interact with carboxylation of coagulation factors but also impair MGP carboxylation (Diener et al, 2012). These constellations make CKD patients (Goodman et al, 2000; Foley et al, 1998) and patients undergoing VKA therapy (Schurgers et al, 2004; Koos et al, 2005; Lerner et al, 2009) prone to vascular calcification. Treatment of CKD patients with vitamin K2 has been a suggested option to inhibit vascular calcification by counteracting the vitamin K deficiency (Westenfeld et al, 2012). An important study added MK4, to complement with the vitamin K antagonist. They found that the additional K2 supplementation on top of a VKA diet attenuated the calcification of AVF veins in both CKD animals and animals with healthy renal function (Zaragatski et al, 2016).
Despite the frequency of warfarin prescription, there are few studies that have evaluated the consequences of its use in patients with CKD, and they reveal that warfarin treatment is associated with arterial calcification and upregulation of uncarboxylated MGP (ucMGP) (Schurgers et al, 2004; Koos et al, 2005; Holden et al, 2007; Weijs et al, 2011; Rennenberg et al, 2010). Warfarin treated patients with CKD develop vitamin k deficiency with a high prevalence of vascular calcification and vertebral fractures, and a much higher risk of death (Fusaro et al, 2015; Lin et al, 2017). One study has demonstrated that long-term warfarin exposure was independently associated with greater severity of aortic valve calcification in dialysis patients (Holden et al., 2007). A multicenter, cross-sectional study with a 3 year follow-up of patients on hemodialysis for more than 1 year, showed that the use of warfarin was associated with increased odds of aortic and iliac calcification, vertebral fractures and mortality in warfarin-treated hemodialysis patients (Fusaro et al, 2015).
Concerns have been raised about therapeutic vitamin K antagonism (warfarin) in dialysis patients with atrial fibrillation (Chan et al, 2009; Kruger et al, 2009) In a retrospective study, it was shown that dialysis patients have an increased risk for both hemorrhagic and ischemic stroke when treated with warfarins compared with no treatment at all (Chan 2009). In addition, in a randomized trial to prolong graft patency with warfarin, the study had to be stopped because of significantly increased major bleeding events in the treatment group (Crowther et al, 2002).
Calciphylaxis (calcific uremic arteriolopathy) is a rare, disastrous, and often lethal manifestation of vascular calcification in CKD patients and is characterized by calcifications of cutaneous arterioles with subsequent exulcerations and superinfection (Ross, 2011). Anecdotal evidence has linked warfarin use to the pathogenesis of calcific uremic arteriopathy in patients with ESKD (Coates et al., 1998; Schurgers et al., 2005; Danziger, 2008). About 50% of patients with CKD stage 5D who develop calciphylaxis are on VKAs (Verdalles Guzman et al, 2008; Chatrou et al, 2012). Data from the German Calciphylaxis registry and a Japanese survey demonstrate that treatment with warfarin represents a risk factor for calciphylaxis (Brandenburg et al, 2011; Hayashi et al, 2012). A recent study looked at levels of carboxylated and uncarboxylated MGP and found that for every 0.1 unit reduction in relative carboxylated MGP concentration was associated with a more than two-fold increase in calciphylaxis risk (Nigewekar et al, 2017). This potential pathomechanism has prompted the Vascular Calcification Working Group of the National Kidney Foundation to put forward efforts to better understand the role of vitamin K antagonists in the vascular disease of CKD patients, including the implementation of a calciphylaxis registry, investigating warfarin use in relation to outcomes from the registry (Goodman et al., 2004), and to consider recommending avoiding the use of vitamin K antagonists in patients with CKD Stage 5, wherever possible.
Furthermore, the ESRD cohort has several particular characteristics that might contribute to their overall sensitivity to warfarin use, including the combination of vitamin K deficiency, phosphate elevation, and vitamin D use, which might cumulatively add to the potential vascular toxicity of warfarin. Clearly, more studies are needed to evaluate the relationship of warfarin, VKDPs, and vascular calcification in the ESRD cohort.
Statins.
Kidney disease is associated with a prevalence of coronary artery calcification (CAD). . Statins have been prescribed to manage the CAC. However research has shown that statins did not improved the CA score, and repeated imaging showed that statin therapy was associated with a greater progression of CAC (Chen et al, 2017). Data suggests that statin therapy may have a negative impact on vitamin K. When mice were given atorvastatin and vitamin K1, there was a 41% reduction of MK4 in the kidney in mice (Caluwe et al, 2020). A clinical study conducted on hemodialysis patients treated with statins showed higher baseline coronary artery calcification and a greater progression of calcification compared to hemodialysis patients who did not receive statins (Turner et al, 2018).
-CALCIFICATION INHIBITORS
The treatment goal has shifted to promoting the factors that inhibit calcification in CKD-BMD, such as vitamin K, but the research is still in its infancy (Haroon et al, 2020). Although animal and in vitro data support this role for vitamin K, actual clinical trials with CKD patients have hardly begun. (Holden et al, 2015; Krueger et al, 2013). Research has just begun to explore and clarify the role of vitamin K in CKD, considering both vitamin K1 (phylloquinine) and vitamin K2 (menaquinones), typically focusing on Mk4 and Mk7. A preventive role for vitamin K in vascular calcification has been proposed based on its role in activating matrix Gla protein (MGP), a calcification inhibitor that is expressed in vascular tissue, and other vitamin K dependent proteins (Gallieni et al, 2012).
There are naturally occurring inhibitors of calcification, which are all involved in the maintenance of vascular tissue. Some of them include fetuin-A, matrix gla Protein (MGP), osteocalcin, and bone morphogenetic proteins (BMPs), and many of them are vitamin K dependent proteins. As already described, Vitamin K-dependent proteins play an essential role in the pathogenesis of mineral and bone disorders related to CKD, including vascular calcification (Neven et al, 2011; Zak-Golab et al, 2011). The realization that calcification in CKD-BMD as an actively regulated process, and can be managed is a relatively recent conclusion and highlights the potential of vitamin K. Clinical trials on calcification inhibitors and kidney disease are relatively sparse, but nonetheless, we will present an overview thus far.
· Fetuin A- Fetuin-A is a protein synthesized in the liver and secreted into the circulation throughout the body. It is the most important systemic inhibitor of soft-tissue calcification (Heiss et al, 2003; Suliman et al, 2008). It accumulates in the skeleton during mineralization (Schinke et al., 1996). Animal data show that mice deficient in fetuin develop extensive soft tissue calcifications in the myocardium, kidney, tongue and skin (Schafer et al, 2003; Ketteler et al, 2003; Ketteler, 2005), the severity and extent of which are exacerbated in the uremic state (Jahnen-Dechen et al, 1997; Schafer et al, 2003; Westenfield, et al, 2004). Moreover, there is an association between low fetuin-A levels and the magnitude of valvular calcification (Wang et al,2005). In vitro, Fetuin-A inhibited mineralization and the data demonstrated that fetuin-A, and MGP play an important role in uremic vascular calcification (Moe et al., 2005). In vitro studies of VSMCs undergoing osteogenic differentiation have shown that fetuin-A is taken up by these cells and inhibits calcification. (Reynolds et al, 2005).
Clinical studies consistently show that fetuin-A deficiency is associated with increased vascular calcification, all-cause and cardiovascular mortality in CKD patients (Moe et al., 2005; Odamaki et al., 2005; Suliman et al., 2008). Fetuin-A levels begin to decline from the early stages of CKD and are significantly lower in patients with atherosclerosis (Sevinc et al, 2021). Ketteler (et al, 2003) demonstrated that the concentration of fetuin-A in serum is lower in CKD Stage 5 hemodialysis patients than in individuals of corresponding age and sex without renal disease, and this was correlated with increased mortality. Furthermore, circulating levels of fetuin-A are increased in patients with calciphylaxis, perhaps indicating a failed attempt to maintain calcium homeostasis. Serum from dialysis patients was found to be significantly less effective at inhibiting calcium phosphate crystal formation than normal serum with appropriate fetuin-A concentrations, and this lack of efficacy could be reversed by the addition of purified fetuin-A in quantities that restore serum levels to normal (Schafer et al, 2003; Ketteler et al, 2003).
Besides fetuin-A, a number of small vitamin K–dependent proteins have been discovered acting as potent calcification inhibitors. Examples are matrix Gla protein (MGP), osteocalcin (OC), also known as bone Gla protein, and possibly also the newly discovered Gla-rich protein (GRP). In contrast to fetuin-A, these proteins are local inhibitors of calcification, i.e., they are synthesized in the tissues in which they exert their function.
· Matrix Gla Protein (MGP) - Matrix Gla protein (MGP), is one of the most potent inhibitors of arterial calcification and matrix mineralization (Gopalakrishnan, et al, 2001; Schurgers et al., 2007; Luo, et al., 1997; Malyszko et al. 2002; Malyszko et al, 2004; Holden et al., 2008), and was the first endogenous calcification inhibitor to be identified. MGP regulates tissue mineralization and is synthesized by vascular smooth muscle cells and chondrocytes, locally in the arterial wall (Murshed et al, 2004; Ketteler et al, 2003; Ketteler et al, 2005). MGP has been shown to modulate both cell differentiation and calcification (Bostrom et al., 2001; Zebboudj et al, 2002; Newman et al., 2001). MGP inhibits bone morphogenetic protein 2 and 4 (BMP-2 and -4) (Zebboudj et al., 2003; Yao et al., 2006; Yao et al., 2009), suppresses the differentiation of vascular smooth muscle cells into embryonic bone cells (Speer et al.,2009), and directly inhibits calcium-crystal growth in the vessel wall (Shanahan, 2005; Schurgers et al., 2008; O’Young et al, 2011; Cui et al, 2018). (BMP-2 and BMP-4 are potent inducers of bone formation (Zebboudj et al, 2002)),
The importance of MGP as an inhibitory factor for vascular calcification was illustrated in the MGP knock-out mouse, which spontaneously develops massive aortic calcification and dies at 6-8 weeks of age as a result of aortic rupture and subsequent internal hemorrhage (Luo, 1997). In data from humans, the extent of coronary calcification, as determined by EBCT, is correlated with serum MGP levels (Jono et al., 2004). MGP is not present in normal blood vessels; however high local MGP expression is usually found in the vicinity of atherosclerotic plaques, especially in the lipid-rich regions surrounding calcified areas (Shanahan et al, 1994; Dhore et al 2001; Schurgers et al., 2001 Canfield et al., 2002). As in the case of fetuin-A, this pattern is interpreted as a local attempt to counteract and limit vascular calcification. Eventually, this attempt at regulation fails, and the expression of MGP is decreased globally before atherosclerotic or medial calcification occurs (Shanahan et al., 2000; Hao et al., 2004). Consistent with this, there is research showing that folks with an MGP genetic polymorphism was associated with kidney stones (Lu et al 2012), highlighting the central role of MGP and calcium developments.
MGP requires vitamin K-dependent gamma-carboxylation for biological activation and carboxylation (Schurgers, 2007), which is required for its capacity to inhibit calcification (Demer, 1995; Wallin et al., 2000). The presence of vitamin K permits the abundant Gla-MGP expression in the arterial wall, with a subsequent reduction in vascular calcification (Krueger et al., 2009;). The carboxylated form of MGP is carried in plasma by fetuin (Price et al., 1987). It has been shown that undercarboxylated MGP (ucMGP) is associated with intimal and medial calcification, indicating local or systemic vitamin K depletion is a potentially important confounder in the development of arterial calcification ((Schurgers, et al., 2005; Delanaye, et al 2014).
Moe (et al, 2005) has shown a direct correlation between local MGP expression and the presence of calcification in sections from arteries of patients with CKD Stage 5. Significantly lower ucMGP levels were found in dialysed patients compared to age-matched controls. Severely calcified arteries from diabetic patients exhibited a very high proportion of undercarboxylated MGP in close spatial association with calcifications, pointing to local or systemic vitamin K deficiency (Schurgers et al. 2005; Gao et al, 2007; Lu et al, 2012; Lu et al, 2013; Wei et al, 2018; Mizuiri et al, 2019). In this dialyzed patient population, inverse correlation was found between augmentation index, an arterial stiffness parameter, and serum ucMGP levels. Besides ucMGP had an inverse association with phosphate and a positive association with fetuin-A levels, suggesting that low ucMGP can be a marker of active calcification and impaired arterial stiffness in dialysis (Hermans, et al., 2007). Wei et al (2016) showed that MGP was co-localized with microcalcifications in diseased kidneys, and was absent in normal kidneys. They concluded that active MGP may inhibit the calcification in renal tissue. In a separate paper they present data showing that high renal microvascular function was inversely associated with the amount of uncarboxylated MGP in several ethnic groups. In conclusion, the current findings from Wei (et al, 2016) serve the extend the protective role of vitamin K from the macrocirculation to the microcirculation - as exemplified by renal function, and possibly suggest a potential for prevention by vitamin K supplementation.
Kidney Stones and MGP
Kidney stones (also called renal calculi, nephrolithiasis or urolithiasis) are hard deposits made of minerals and salts that form inside your kidneys. Kidney stone formation is a complex event and results from an imbalance of promoting and inhibiting factors (Moe, 2006). The pathological mechanism of kidney stone formation was at least partly analogous to vascular calcification, such as forming calcific plaques, increasing expression of calcification inhibitors and regulating actively calcification process. Hydroxyapatite was observed in both atherosclerotic plaques and kidney stones.
MGP regulates vascular calcification of the extracellular matrix. MGP is expressed in the kidney, where it directly binds to crystals (Aggarwal KP, et al, 2013). Two case–control studies found an association between nephrolithiasis and genetic variation in the MGP gene (Gao et al, 2007; Lu et al, 2012). In rat models of nephrolithiasis, lack of MGP expression was associated with crystal formation in injured renal tubules (Lu, Tao et al, 2013), whereas its expression was upregulated in response to calcium oxalate (Gao et al, 2010; Lu et al, 2013). A recent study found that for a every doubling of uncarboxylated, inactive MGP, the odds of kidney stones increased by 31%. The longitudinal analysis spanning 12 years of follow-up showed that the risk of having recurring kidney stones increased 2.5 fold for the doubling of uncarboxylated MGP (We, et al, 2017). Research has already established that supplementation with vitamin K2, 180mcg per day, decreased inactive MGP (Knapen et al, 2015). So it appears that one important factor in the development of kidney stones is a vitamin K deficiency, where matrix Gla protein is not activated and cannot help inhibit the calcification that takes place. And research has demonstrated that treatment with vitamin K1 can inhibit the formation of renal crystals in vivo. VK1 increases MGP expression and functions through MGP to reduce crystal deposition in cells and provide cell protection, indicating that VK1 treatment could be a potential strategy for the treatment and prevention of nephrolithiasis (li et al, 2019).
· Bone Gla Protein (BGP) - Osteocalcin, or bone Gla protein, is a small gamma-carboxylated protein that is expressed by both osteoblasts and VSMCs and is abundantly deposited in the extracellular matrix of bone and in the calcified vasculature (Shanahan et al., 2000; Shanahan et al., 1999; Proudfoot et al., 2002). When carboxylated, BGP binds hydroxyapatite, which is the foundation matrix that embeds calcification (Shanahan et al, 2000; Price, 199; Ducy et al, 1996). Osteocalcin is an active modulator of VSMC cell signaling and osteochondrogenic differentiation in VSMCs, but additional studies are required to establish the form and source of osteocalcin that can exert these effects, and the VSMC receptor that mediates downstream signaling (Idelevich et al, 2011). Knockout mice, bred for genetic removal of BGP processing, develop hyperostosis which is an excessive growth of bone, suggesting osteocalcin is a determinant of bone formation (Ducy et al., 1996). Given the important role of osteocalcin in the regulation of metabolism, it may be a new link between vascular calcification and bone and metabolic disorders that may help to explain some of the apparent association of bone loss with vascular calcification in some patient groups like those with CKD-BMP. (Kapustin & Shanahan, 2011). Szulc, et al, (1993) found that uncarboxylated osteocalcin (BGP), not conventional calcium metabolism measures, predicted the risk of hip fracture. Osteocalcin levels in the blood are predictors of cardiovascular events in patients on hemodialysis (Yamashita et al, 2013).
· Growth arrest specific gene-6 (GAS-6) – Gas-6 is a vitamin K dependent protein produced by vascular smooth muscle cells and is involved in many physiologically important processes, including inflammation and calcification (Fernandez-Fernandez et al, 2008). It was found in 1988 and has a high structural homology with protein S, another VKD protein. It is found in the lung, heart, kidney, intestine, bone marrow, VSMCs and the liver (Manfioletti et al, 1993; Nakano et al., 1995). It affects vascular smooth muscle cell movement and death, and is considered a local regulator of calcification, protecting against vascular calcification (Hurtado et al, 2011; Saller et al, 2006). In sites of cellular injury, Gas-6 provides protection from cell death (Melaragno et al, 2004). In a model of phosphate-induced vascular calcification, Gas-6 signaling protected VSMCs from calcification by inhibiting apoptosis (Son et al., 2006). This is relevant in the context of vascular calcification, as apoptotic VSMCs can serve as a nidus for calcium phosphate precipitation.
Given the prevalence of inflammation and vascular disease in people with CKD, research showed that Gas-6 was significantly increased compared with normal controls. The levels of Gas-6 rose with each advancing stage of kidney disease, and were inversely associated with GFR and have been inversely correlated with MRP levels (Hallajzadeh et al, 2015). It was concluded that Gas-6 is dysregulated with renal disease and inversely proportional to renal function (Lee et al, 2012). Gas6 given to mice led to improvement following a sepsis induced kidney injury (Chen et al, 2016), and reduced both cell death and inflammation (Giangola et al, 2015). In an animal study, treatment with Gas-6 significantly decreased blood levels of creatinine and BUN by 29% and 27%, respectively, improved the renal histological injury index and reduced apoptosis in the kidneys (Giangola et al, 2015). Another animal study showed that the administration of Gas6 for sepsis reduced nitrogen and creatinine, and renal damage, and improved survival (Chen et al, 2016).
· Gla Rich Protein (GRP) – GRP is a vitamin K dependent protein, and it has the highest Gla percent of any known protein (Viegas, et al., 2008), hence its name. It is a circulating protein that found in bone cells, and is also expressed and accumulated in soft tissues, including the skin, and vascular system, and accumulates in high levels at sites of pathological calcification in the vascular system, and at cancer sites (Viegas, et al, 2009; Cancela et al, 2012). Low blood levels of GRP have been shown as a marker of vascular calcification in CKD patients (Silva et al, 2020). Though the research has just begun, it is believed that GRP may be involved as a modulator of calcium availability, and an inhibitor of osteogenesis (Surmann-Schmitt et al, 2008; Viegas et al 2018; Willems et al 2018). Discovered only in 2008, it has been found to have an exceptional capacity to bind calcium and collagen, and much remains to be learned about GRP. GRP has been found to be an important inhibitory component of calciprotein particles, which are believed to possess a defense mechanism against mineral metabolism (Yamada et al, 2018; Viegas et al, 2018).
· Bone morphogenic proteins (BMP) - BMPs are a group of growth factor proteins also known as cytokines (molecules that are involved with metabolism and homeostasis). They help regulate, repair, and maintain bone formation, and they can be found at sites of vascular calcification (Bleuming et al., 2007). They are not vitamin K dependent proteins, but depend on carboxylated vitamin K dependent proteins, such as MGP to bind and inhibit calcification (Bostrom et al, 2001; Zebboudj et al, 2002; 2003; Li et al, 2012). So far, thirty different BMPs have been discovered. BMP-2 and BMP-7 are frequently studied in relation to calcification (Bostrom et al, 1993). BMP-2 is thought to help induce differentiation of VSMCs into bone like tissue and calcification (Chen et al, 2003; Dhore et al, 2001). BMP-7 is a regulator of skeletal remodeling and the VSMC phenotype and reduces serum phosphate in the process. BMP-7 is thought to be key to normal kidney development (Simon et al, 1999; Wang et al, 2003), and in CKD, BMP-7 has been found to reverse vascular calcification. BMP-7 has been shown to be protective against the progression of vascular calcification in uremic mice fed a high-fat/cholesterol diet (Davies et al, 2003; Davies et al, 2005). In an animal model of calcification worsened by CKD, via genetic modification, animals were treated with a BMP-7 dosage every day for 15 weeks. Untreated uremic mice experienced an increase in aortic root calcification, whereas BMP-7–treated mice exhibited a reduction in calcification, and osteocalcin as an osteoblast marker was down-regulated (Mathew et al, 2007). In an epidemiological study in CKD patients, plasma BMP-7 levels were significantly higher than in control subjects, compatible with the hypothesis of an early mobilization of the protein against vascular calcification (Musial et al, 2008). It is important to note that BMP-7 was originally identified as a regulator of bone homeostasis (Ishimura, 2005).
In general, mounting evidence shows that VKDPs (vitamin K dependent proteins) are useful tools to improve early diagnosis, monitor progression or identify complications of CKD (Silaghi et al, 2019).
Vitamin K Supplementation
It is well known that CKD patients are at high risk of vascular calcification. Vitamin K deficiency results in functionally inactive MGP, and it has been documented that people with CKD-BMD are deficient in vitamin K, meaning that supplementation with vitamin K could represent an important opportunity to modify and reduce a major risk factor for vascular calcification in people with CKD (McCabe et al., 2013; Fusaro et al, 2017; Wei, et al 2016; Wei, et al 2016B; Wuyts & Dhondt, 2016; Lee & An, 2019). Even after kidney transplantation, vitamin K deficiency was associated with significantly increased risk in all-cause mortality, among patients followed over a median of 9.8 years (Boxma et al, 2012; Keyzer et al, 2015; Fusaro et al, 2020a). Obviously, this group is an ideal target for testing whether vitamin K supplements can normalize the circulating dp-ucMGP levels and whether the change in vascular vitamin K status will result in an improved clinical outcome (Stępień et al, 2020).
The data basis for the detrimental role of vitamin K deficiency, on calcification in CKD patients is constantly growing stronger over time. There is a growing consensus that all patients on dialysis should be supplemented with vitamin K, with the goal of conducting the research that determines the end points, in a patient-based manner (Ketteler & Brandenburg, 2017; Bellone et al, 2022).
Early experimental studies with animals have established that it is possible to modify calcification inhibitors or their regulators and have an impact on vascular calcification in the context of CKD, with the supplementation of vitamin K (Schurgers 2013). In a research setting, warfarin is often used to induce calcification. Spronk (et al., 2003) gave both warfarin and phylloquinone to create arterial calcification in rodents. In this model, the high levels of warfarin knock out the carboxylation of MGP, leading to calcification of the arteries, while the phylloquinone maintained normal coagulation. He then supplemented with a diet rich in K1 or MK4, and showed that the MK4, not K1, was the key factor that inhibited the warfarin-induced arterial calcification. This is explained by the different transport and tissue distribution of menaquinones, resulting in a much more prominent protective effect of menaquinones (compared with phylloquinone) on arterial calcification.
Additionally, diets high in vitamin K have been shown to improve arterial elasticity in warfarin-treated rats, suggesting that the calcification from warfarin treatment is due to the inhibition of the vitamin K-dependent gamma-carboxylation of MGP. Regression of this vascular pathology in a rat model was found under high intake of both vitamin K1 and K2 (Schurgers et al, 2007). In addition, MGP isolated from atherosclerotic plaque of aging rats was found to be incompletely uncarboxylated, thereby inhibiting its ability to function as a calcification inhibitor (Sweatt et al, 2003). It has already been established by others that high dietary vitamin K (K1 or MK-4) increases the carboxylation of MGP, and that supra-therapeutic levels of warfarin shift the balance to the uncarboxylated form (Schurgers et al, 2007).
In the most relevant and thorough study yet, McCabe and colleagues (2013) evaluated the role of vitamin K and therapeutic levels of warfarin on the vasculature of rats with CKD. They aimed to determine whether warfarin or a diet supplemented with vitamin K would modify arterial calcification in rodents. They also investigated whether the presence of CKD modified the concentrations of vitamin K1 and MK4 is tissues. They measured the calcium content within four arteries, before and after inducing CKD. At the end of a 7 week treatment, they found substantial calcification when high doses of warfarin were administered. There was no significant elevation in calcium found in CKD animals treated with high dietary vitamin K, in any vessel, compared with controls. In CKD animals treated with low dietary vitamin K, calcium levels were significantly elevated in both the renal artery and abdominal artery. To confirm that altering vitamin K status would modify the serum and tissue concentrations of K1 and MK4, they measured concentrations of both in the serum, liver, heart, kidney and aorta. They found that tissue concentrations of both K1 and MK-4 were markedly elevated in all animals assigned to the high K1 diet. In animals treated with warfarin, there were significant reductions in vitamin K concentrations in the heart and kidney, but not in the liver, as well as markedly increased susceptibility to calcification in all vessels studied. In both control and CKD animals, K1 was the primary form of vitamin K in serum, liver, and cardiac tissue, whereas MK-4 was the primary form of vitamin K in the kidney. The aorta contained both K1 and MK-4. They concluded that vitamin K status was critical in the predisposition of blood vessels to calcification in a rodent model of CKD. And that therapeutic doses of warfarin, markedly increased vascular calcification, whereas high dietary vitamin K1 intake attenuated the vascular calcification in animals with CKD, despite hyperphosphatemia, while also restoring tissue calcium content comparable to that of non-CKD animals. The results of this study support a role for vitamin K as a potential treatment option to attenuate the development of vascular calcification in CKD (McCabe et al., 2013). If this finding holds true for patients with CKD, it would be of great importance with huge therapeutic implications for vitamin K treatment.
Kaesler and colleagues (2014) induced uremia in rats and studied the calcification that took place outside of the bones. After seven weeks, there was overt calcification in the aorta, heart and kidneys. Treatment with vitamin K for four weeks restored the carboxylase activity within the kidneys and reduced the heart and kidney calcification that had begun. Curi (et al, 2018) found that MK4 supplements reduced bone mineralization in rats through the BMP-2 pathway.
In studies of animals with CKD, the research has established that vitamin K plays a key role in the inhibition of vascular calcification. Research on the vitamin K in people with CKD-BMD is still in its infancy, and the question of whether increased vitamin K intake also is protective against vascular calcification in patients with CKD and might help to decrease their high cardiovascular mortality remains to be determined in prospected clinical trials (Parker et al, 2009; Shea & Holden, 2012; McCabe et al, 2013; Schurgers, 2013; Gallieni & Fusaro, 2014; Wei et al, 2016; Wei et al, 2018). Puzantian (et al, 2018) established a link between circulating dp-ucMGP and kidney dysfunction and calcification.
The early findings are promising (Shea & Holden, 2012). Schlieper and colleagues (2011) tested whether dephospho-carboxylated MGP and desphospho-uncarboxylated MGP (dp-ucMGP) predicts survival in a cohort of hemodialysis patients. Additionally they tested whether vitamin K2 supplementation can improve the deficient vitamin K status in dialysis patients. Pivka-II measures the plasma levels of the liver protein induced by vitamin K absence. The majority of dialysis patients (121/188) exhibited a vitamin K deficiency as indicated by increased PIVKA-II levels. When adjusted for age, low plasma levels of dp-cMGP remained a significant predictor for all-cause and cardiovascular mortality in dialysis patients. IT appears that the level of matrix Gla proteins can be a predictor of mortality in patients (Roumeliotis et al, 2017). Next they looked to determine whether vitamin K can affect those levels. 17 hemodialysis patients were given vitamin K2 (135 ug) orally over six weeks, resulting in a significant reduction of dp-ucMGP. This establishes that vitamin K2 supplementation can improve the vitamin K status of dialysis patients.
Westenfeld et al. demonstrated that menaquinone supplements induce a dose-dependent decrease in plasma dp-ucMGP levels in dialysis patients. After establishing a significant vitamin K deficiency in hemodialysis patients, Westenfeld et al (2012) also investigated whether daily vitamin K supplementation improves the bioactivity of vitamin K-dependent proteins in hemodialysis patients, assessed by circulating dephosphorylated-uncarboxylated MGP, uncarboxylated osteocalcin, and uncarboxylated prothrombin (PIVKA-II). Vitamin K(2) supplementation of 135 ug and 360 ug MK7, induced a decrease in circulating undercarboxylated forms for all vitamin K dependent proteins, including dephosphorylated-uncarboxylated MGP, uncarboxylated osteocalcin, and PIVKA-II levels, after only six weeks of daily supplementation. More importantly, it is the first study showing that inactive MGP levels can be decreased markedly by daily vitamin K(2) supplementation for CKD patients, and provides the rationale for intervention trials aimed at decreasing vascular calcification in dialysis patients by vitamin K supplementation. This shows that vitamin K is able to reach the tissues, including the vessel wall, and to correct the biochemical and local tissue consequences of vitamin K deficiency (Wallin, Schurgers, Wajih, 2008).
Kurnatowska and colleagues (2013) conducted a prospective, randomized study designed to compare the effect of oral administration of vitamin K2 plus low-dose vitamin D or vitamin D alone on the progression of coronary artery calcification score (CACS) and common carotid intima media thickness (CCA-IMT). 42 non-dialysis patients with CKD stage 3-5 and 37 patients with CKD stage 3-5 not requiring dialysis with a coronary artery calcification (CAD score) were studied. The subjects received a daily dose of either 9 ug of vitamin K2 plus 10 ug of a vitamin D or 10 ug of vitamin D only. There were no significant changes of renal function during the study. There was a significant increase of serum OC in patients with low dose vitamin D but not in the K + D group. CAC score increased in both groups, numerically less in vitamin K+D treated patients. In 5 of 26 patients (about 1/5) treated with vitamin K, there was a regression of CAC scores. They concluded that vitamin K2 therapy may slow the progression of atherosclerosis and vascular calcification in non-dialyzed CKD patients. In a later study, they were able to demonstrate that those subjects who received both vitamin K and D, had significantly less thickening of the carotid artery, the rate of progression in their calcium score was lower, and they showed a significant decreased in the levels of uncarboxylated MGP and OSteocalcin. (Kurnatowska et al, 2015).
The KING trial (vitamin K2 In reNal Graft) is a single-arm study that evaluated the association between the change in vitamin K status and indices of arterial stiffness following 8 weeks of menaquinone-7 (vitamin K2) supplementation (360 mg once daily) among renal transplant recipients (n ¼ 60). Vitamin K2 supplementation was associated with improvement in subclinical vitamin K deficiency and arterial stiffness (Mansour et al, 2017). The VIKI (vitamin K Italian) study showed that vitamin K status improved and there were lower levels of inactive vitamin K dependent proteins within one year after kidney transplantation (Fusaro et al, 2019).
In a later study, Kurnatowska with this group, they evaluated the association between plasma dp-ucMGP, kidney function and cardiovascular risk factors before and after a nine month administration of vitamin K2 in non-dialysis patients with CKD. They found that the vitamin K2 supplementation decreased the dp-ucMGP level by almost 11%. They concluded that poor vitamin K status was associated with kidney damage and may also serve as a marker of cardiovascular risk (Kurnatowska et al, 2016).
Mosa (et al, 2020) investigated the impact of high doses of vitamin K1 (10 mg) administered after each hemodialysis for one year. They found that vitamin K significantly slowed the progress of vascular calcification.
An additional benefit from supplementing with vitamin K may be its beneficial effect on the bone disease that results from CKD. It has been established that vitamin K improves bone health (http://www.k-vitamins.com/index.php?page=Bone) as vitamin K is an essential cofactor for the carboxylation of osteocalcin and other bone matrix proteins (Vermeer et al., 1995).
There are not many studies involving CKD patients and vitamin K supplementation, related to bone health (Kohlmeier et al., 1997). A year-long placebo controlled trial in hemodialysis patients showed a favorable effect of vitamin K supplements on bone density (Akiba et al., 1991). Patients with serum phylloquinone concentrations of 1.2 nmol/liter or less had suffered bone fractures at a rate of more than 6% /year during hemodialysis treatment. More than half of the hemodialysis patients had serum phlloquinone concentrations below this threshold and might benefit from supplemental vitamin K. Preliminary results from a 12 month intervention trial in dialysis patients indicate that vitamin K supplementation helped to conserve bone mineral mass and may thereby decrease bone fracture risk (Akiba et al., 1991).
Researchers believe the evidence points to vitamin K being effective for bone health in CKD. Fusaro (et al., 2011) reviewed the current literature on the relationship between vitamin K2 status, fragility fractures and vascular calcification in CKD patients and believed that Vitamin K could play a key role, as it carboxylates both matrix Gla protein as well as bone Gla protein (osteocalcin), to become biologically active (Fusaro et al, 2011; Chauhan et al., 2012). Vitamin K intake protects against loss of bone mineral density and deterioration in the quality of bone structure. Low vitamin K concentrations are associated with increased risks of fractures and vascular calcification, and frequent complications in dialysis patients. If vitamin K supplementation could prevent bone fractures, that would be an important clinical outcome (Jadoul et al., 2006; Rodriguez-Garcia et al., 2009). Fusaro and her group recommend investigations into supplementing CKD patients with vitamin K to avert both fragility fractures and vascular calcifications.
Fusaro (et al., 2012; Fusaro, Noale et al 2012) and her research group carried out an observational study to establish the prevalence of vitamin K deficiency and to assess the relationship between vitamin K status, vertebral fractures, vascular calcification, and survival in 387 patients on hemodialysis for one or more years and 62 healthy controls. They measured the plasma levels of vitamin K compound, bone-Gla protein, matrix-Gla-protein, and routine biochemistry. They also investigated vertebral fractures and aortic and iliac calcifications in a spine radiograph. Three year patient survival was analyzed. 35.4% of patients had deficiency of MK7, 23.5% had a deficiency of vitamin K1, and 14.5% had a deficiency of MK4. A total of 55.3 of patients had vertebral fractures, 80.6% had abdominal aorta calcification, and 56.1% had iliac calcification. Vitamin K1 deficiency was the strongest predictor of vertebral fractures. MK4 deficiency was a predictor of aortic calcification, and MK7 deficiency was a predictor of iliac calcification. They found the presence of vertebral fractures was also a predictor of vascular calcifications. They felt their study suggests that the vitamin K system may be important for preserving bone mass and avoiding vascular calcification in hemodialysis patients, pointing to a possible role of vitamin K in both bone and vascular health.
Summary
In this section, we have reviewed the research as it pertains to kidney function and vitamin K. Kidneys are a vital organ in the health of your body, and when they begin to fail, the systems they support become dysregulated, hence the new term Chronic Kidney Disease- Bone Mineral Disorder. CKD-BMD is a very new understanding of the systemic dysregulation that takes place in the uremic environment of chronic kidney disease, which actively creates the heart disease and calcification that is the leading cause of death for people with CKD. Since KIDGO recognized the Bone Mineral Disorder of Chronic Kidney Disease, there have been recommendations to conduct clinical trials evaluating calcification inhibitors that would best prevent or delay the calcification, with specific recommendations that vitamin K be evaluated (KDIGO, 2009). Trials are underway now in Germany, the Netherlands (Theusweissen et al., 2013) and other locations to determine how vitamin K could improve the outcomes in kidney failure, and whether vitamin K supplementation could lead to therapeutic strategies that could end vascular calcification as the number one cause of death among people with chronic kidney disease (Schlieper et al, 2011; Schurgers, 2013; Haroon et al, 2020; Holden et al, 2015)). Future clinical trials could explore such questions as determining the optimal dosage for supplementation, as well as determining the safety of supplements for patients on long-term warfarin or coumarin therapy (Fusaro et al., 2011), as well as the delineating the effects of the different vitamin K forms on vascular calcification (menaquinones or phylloquinone) (Shea & Holden, 2012).
Vitamin K is associated with the prevention of heart disease and calcification. Sufficient amounts of vitamin K are necessary to activate the proteins that inhibit calcification. It has been established that people with CKD have a vitamin K deficiency. Active MGP may not only inhibit calcification but may be protective for renal function. There is a compelling need to ensure adequate vitamin K stores (Epstein, 2016).
It is exciting to consider that supplementing with vitamin K, and eliminating that deficiency, may be a simple but potent strategy to actively manage the calcification produced by the uremic environment. Vitamin K may be a new therapeutic approach for promoting renal health, either by increasing the dietary intake of vitamin K or by supplementing with vitamin K (Fusaro et al, 2021). Thankfully, the scientific community is now beginning the necessary research.
1970
Ibels LS, Stewart JH, Mahony JF et al. Deaths from occlusive arterial disease in renal allograft recipients. BMJ. 1974;3:552–554.
In a series of 325 recipients of cadaveric renal transplants sudden occlusive arterial disease was found to be responsible for 12% of deaths. Acute myocardial infarction (9%) occurred 25 times more than expected in the normal population and cerebral thrombosis (3%) 300 times more. The greatest loss was in the initial three-month period after transplantation. Patients with renal failure due to essential hypertension were especially at risk, accounting for six of the 12 deaths.
Tatler GL, Baillod RA, Varghese Z et al. Evolution of bone disease over 10 years in 135 patients with terminal renal failure. BMJ. 1973;4:315–319.
An objective radiographic study of a variety of bone diseases, including erosions, fractures, as well as peri-articular and vascular calcification was made in a series of 135 patients over 10 years of maintenance haemodialysis therapy. The four lesions progressed at different rates, consistent with variation in the response of tissues to a changing biochemical milieu and deficiency in vitamin D metabolites. The half time for development was 3·4 years for vascular calcification, 9 years for fractures, 16 years for periarticular calcification, and 22·9 years for erosions. Calcification of the dorsalis pedis artery seen as a developing ring or tube was an early and valuable sign of disturbed calcium metabolism. In these patients renal osteodystrophy is a chronic condition with a prolonged time course.
Alfrey AC, LeGrandre GR, Kaehny WD. Dialysis encephalopathy syndrome: possible aluminum intoxication. N Engl J Med. 1976;294:184–188.
Early study suggesting that aluminum based phosphate binders were toxic.
Lachmann AS, Spray TL, Kerwin DM, Shugoll GI, Roberts WC. Medial calcinosis of Monckeberg: A review of the problem and a description of a patient with involvement of peripheral, visceral and coronary arteries. Am J of Medicine. 1977;63(4):615-622.
Massive medial calcific deposits (Mönckeberg's calcinosis) are described in the peripheral and visceral arteries, and similar deposits in the coronary arteries of a 41 year old woman with diabetes mellitus. Although fairly commonly during life in the muscular arteries of the legs in middle-aged men, medial calcinosis infrequently involves the visceral arteries and has never, to our knowledge, been documented in the coronary arteries. Although it may be associated with intimal atherosclerosis, medial calcinosis, per se, does not obstruct the lumens of the arteries, and, therefore, does not lead to symptoms or signs of limb or organ ischemia. The cause of medial calcinosis remains a mystery, but it appears to affect people with diabetes more frequently than those without.
Ibels LS, Alfrey AC, Huffer WE et al. Arterial calcification and pathology in uremic patients undergoing dialysis. Am J Med. 1979;66:790–796.
The high prevalence of vascular calcification in patients with CKD was noticed as far back as 1979, when Ibels et al, found that both renal and internal iliac arteries of patients undergoing a renal transplant had increased atherogenic and intimal disease and increased calcification, compared with transplant donors. Further, the medial layer was seen to be thicker and more calcified in the uremic patients compared with that of the donors.
1980
Adrogue HJ, Madias NE. Changes in plasma potassium concentration during acute acid-base disturbances. Am J Med. 1981;71(3):456-67.
Andreoli SP. Kleiman MB, Yum MN, Berfgstein JM. Acute eosinophilic interstitial nephritis and sarcoidosis. Archives of Path and Lab Med. 1981;105(11):626-627.
Price P, Williamson M. Primary structure of bovine matrix Gla protein, a new vitamin K-dependent bone protein. J Biol Chem. 1985;260:14971–14975.
MGP is the first vitamin K-dependent protein to be discovered which has several non gamma-carb oxylated residues. MGP is the second vitamin K dependent protein to be discovered in bone, the first being bone Gla protein (BGP).
Lerner SA, Schmitt BA, Seligsohn R, Matz GJ. Comparative study of ototoxicity and nephrotoxicity in patients randomly assigned to treatment with amikacin or gentamicin. Am J Med. 1986;80(6B):98-104.
Price P, Fraser JD, Metz-Virca G. Molecular cloning of matrix Gla protein: implications for substrate recognition by the vitamin K-dependent gamma-carboxylase. Proceedings of the National Academy of Sciences of the USA. 1987;84(23):8335-9.
Suttie JW, Mummah-Schendel LL, Shah DV, Lyle BJ, Greger JL. Vitamin K deficiency from dietary vitamin K restriction in humans. Am J Clin Nutr. 1988;47:475-480.
Ten college aged male subjects received a vitamin K restricted diet for 40 days. Median phylloquinone intakes dropped in half. Serum phylloquinone concentrations fell from a mean of 87 to .46 ng/mL. Supplementation with 50 micrograms of phylloquinone for twelve days increased the serum levels to 1.66 ng/mL. The vitamin K restricted diet resulted in alterations in functional clotting, and supplementation with either 50 or 500 micrograms of vitamin K1 restored both these indices to near normal values.
Knapen MH, Hamulyak K, Vermeer C. The effect of vitamin K supplementation on circulating osteocalcin (Bone Gla Protein) and urinary calcium excretion. Ann Intern Med. 1989;11(12):1001-1005.
Healthy women took 1 mg. of vitamin K for two weeks. In postmenopausal women, vitamin K induced increased serum immunoreactive osteocalcin concentration, normalization of HAB capacity, a decrease in urinary calcium excretion, and a parallel decrease in urinary excretion. It was concluded that vitamin K may be one factor that plays a role in the loss of bone mass in postmenopausal osteoporosis.
Sadowski JA, Hood SJ, Dallal GE, Garry PJ. Phylloquinone in plasma from elderly and young adults: Factors influencing its concentration. Am J Clin Nutr. 1989;50:100-108.
1990
Akiba T, Kurihara S, Tachibana K, et al. Vitamin K increased bone mass in hemodialysis patients with low turn over bone disease. J Am Soc Nephrol. 1991;2:608.
Jespersen F, Jensen JD, Nielsen HK, Lauridsen IN, Andersen MJ, Poulsen JH, et al., Comparison of calcium carbonate and aluminum hydroxide as phosphate binders on biochemical bone markers, PTH(1-84), and bone mineral content in dialysis patients. Nephrol Dial Transplant. 1991;6(2):98-104.
Moss AH, Holley JL, Upton MB. Outcomes of cardiopulmonary resuscitation in dialysis patients. J Am Soc Nephrol. 1992 (Dec);3(6):1238-43.
Bostrom K, Watson KE, Horn S, Wortham C, Herman IM, Demer LL, et al. Bone morphogenic protein expression in human atherosclerotic lesions. J Clin Invest. 1993;91:1800-09.
Artery wall calcification associated with atherosclerosis frequently contains fully formed bone tissue, including marrow. In this study, bone morphogenetic protein-2a was found in human calcified plaque. In addition cells cultured from the aortic wall formed calcified nodules similar to those found in bone cell cultures. These findings suggest that arterial calcification is a regulated process similar to bone formation
Manfioletti G, Brancolini C, Avanzi G, Schneider C. The protein encoded by a growth arrest-specific gene (gas6) is a new member of the vitamin K-dependent proteins related to protein S, a negative coregulator in the blood coagulation cascade. Moll Cell Biol. 1993 Aug;13(8):4976-85.
This research defined a new member of the vitamin Kl-dependent proteins that is expressed in many human and mouse tissues and may be involved in the regulation of a protease cascade relevant in growth regulation.
Saupe J, Shearer MJ, Kohlmeier M. Phylloquinone transport and its influence on gamma-carboxyglutamate residues of osteocalcin in patients on maintenance hemodialysis. Am J Clin Nutr. 1993 Aug;58(2):204-8.
Plasma concentrations of phylloquinone in 42 fasting hemodialysis patients showed a much wider range than in healthy adults. Phylloquinone concentrations in plasma were related to apolipoprotein E genotype in the order E2 > E3 > E4. The percentage of carboxylated osteocalcin (HBC) was related to the plasma concentration of phylloquinone in patients with the apolipoprotein E genotype E3/3, and in patients with the genotypes E2/3 and E2/2. Overall, plasma triglyceride concentration was a better predictor for HBC than was the plasma concentration of phylloquinone. These results point to the overriding importance of chylomicrons for the transport of phylloquinone to liver and bone. Delivery to osteocalcin-producing osteoblasts seemed impaired in patients with the low receptor-affinity apolipoprotein variant E2, suggesting a major role of receptor-mediated chylomicron-remnant uptake in the transport of phylloquinone to bone.
Szulc P, Chapuy MC, Meunier PJ, Delmas PD. Serum undercarboxylated osteocalcin is a marker of the risk of hipo fracture in elderly women. J Clin Invest. 1993 Apr;91(4):1769-74.
It has been previously shown that the level of circulating undercarboxylated osteocalcin (ucOC) is elevated in elderly women in comparison with young, healthy, premenopausal ones. To understand the mechanism of the increase in the ucOC in the elderly and to assess its potential consequences on bone fragility, we have measured ucOC in the sera of 195 elderly institutionalized women 70-101 yr of age. In conclusion, the increase in ucOC in the elderly reflects not only some degree of vitamin K deficiency but also their poor vitamin D status, suggesting that vitamin D may be important, either directly or indirectly through its effect on bone turnover, for achieving a normal gamma-carboxylation of OC. The ucOC, but not conventional calcium metabolism parameters, predicts the subsequent risk of hip fracture, suggesting that serum ucOC reflects some changes in bone matrix associated with increased fragility.
Duquette RL, Dupuis G, Perrault J. A new approach for qualify of life assessment in cardiac patients: Rationale and validation of the Quality of Life Systemic Inventory. Can J Cardiol. 1994 Jan-Feb;10(1):106-12.
Shanahan CM, Cary NR, Metcalfe JC, Weissberg PL. High expression of genes for calcification-regulating proteins in human atherosclerotic plaques. J Clin Invest. 1994;93:2393-2402.
Little is known about the mechanisms which regulate the calcification process. We show that two bone-associated proteins, osteopontin (OP) and matrix Gla protein (MGP), are highly expressed in human atheromatous plaques. The predominant cell type in these areas was the macrophage-derived foam cell, although some smooth muscle cells could also be identified. The postulated function of OP and MGP as regulators of calcification in bone and the high levels and co-localization of both in atheromatous plaques suggest they have an important role in plaque pathogenesis and stability.
Slatopolsky E, Delmez, JA. Pathogenesis of secondary hyperparathyroidism. Am J Kidney Dis. 1994 Feb;23(2):229-36.
Solomon BL, Schaaf M, Smallridge RC. Psychologic symptoms before and after parathyroid surgery. Am J Med. 1994;96:101–106.
Demer LL. A skeleton in the atherosclerosis closet. Circulation. 1995 Oct;92(8):2029-32.
Osteopontin is expfressed in human aortic valvular lesions.
Nakano T, Higashino K, Kikuchi N, Kishino J, Nomura K, Fuita H, et al., Vascular smooth muscle cell-derived, Gla-containing growth-potentiating factor for Ca(2+) mobilizing growth factors. J Biol Chem. 1995;270:5702-05.
Stim JA, Lowe J, Arruda JA, Dunea G. Once weekly intravenous calcitriol suppresses hyperparathyroidism in hemodialysis patients. ASAIO. 1995;41:M693-698.
US Renal Data System: USRDS 1998 annual data report. Am J Kidney Dis. 1998;32:69–80.
Kohlmeier M, Saupe J, Drossel HJ, Shearer MJ. Variation of phylloquinone (vitamin K1) concentrations in hemodialysis patients. Thromb Haemost. 1995;74:1252-4.
Studied intra-and interindividual variation of vitamin K1 concentrations in hemodialysis patients. Phylloquinone concentrations ranged from 0.1 to 9.0 nmol/L, with a mean of 1.09 – 1.90 nmol/L. Most of the variation in serum phylloquinone concentrations was due to differences between patients: serum triglyceride concentrations and apoE genotype together accounted for 64% of interindividual variation. They concluded that individual disposition is a more important determinant of serum phylloquinone concentrations than dietary phylloquinone intake.
Vermeer C, Jie KS, Knapen MH. Role of vitamin K in bone metabolism. Annu Rev Nutr. 1995;15:1-22.
Vitamin K is a cofactor required for the formation of gamma-carboxyglutamate (Gla) residues in proteins. Osteoblasts produce at least three different Gla-containing proteins: osteocalcin, matrix Gla-protein, and protein S. After cellular secretion of these proteins, the main part of each remains bound to the hydroxyapatite matrix in bone, but their function remains unclear. Part of the newly synthesized osteocalcin is also set free into the bloodstream, where it may be used as a diagnostic marker for bone formation. Several studies have demonstrated that a poor vitamin K status is associated with an increased risk of osteoporotic bone fractures. Whether vitamin K supplementation will reduce the rate of bone loss in postmenopausal women remains a matter of debate.
Bach AU, Anderson SA, Foley AL, Williams EC, Suttie JW. Assessment of vitamin K status in human subjects administered “minidose” warfarin. Am J Clin Nutr. 1996;64:894-902.
The response of various measures of vitamin K insufficiency to the administration of 1 mg/d of the vitamin K antagonist warfarin was studied in two groups of nine older (55-75 y) or younger (20-28 y) subjects. The most consistent and extensive alteration was an increase in the concentration of serum under-gamma-carboxylated osteocalcin followed by increased immunochemical detection of plasma under-gamma-carboxylated prothrombin (PIVKA-II), and by a decreased urinary excretion of gamma-carboxyglutamic acid. The concentration of serum under-gamma-carboxylated osteocalcin was lower when subjects consumed 1 mg vitamin K/d than when they consumed their normal diet.
Braun J, Oldendorf M, Moshage W, Heidler R, Zeitler E, Luft FC. Electron beam computed tomography in the evaluation of cardiac calcification in chronic dialysis patients. Am J Kidney Dis. 1996;27:394 – 401.
Ducy P, Desbois C, Boyce B, Pinero G, Story B, Dunstan C, et al., Increased bone formation in osteocalcin-deficient mice. Nature. 1996 Aug;382(6590);448-52.
Vertebrates constantly remodel bone. The resorption of preexisting bone by osteoclasts and the formation of new bone by osteoblasts is strictly coordinated. To investigate the role of osteocalcin, the most abundant non-collagenous protein, we have generated osteocalcin-deficient mice. These mice develop a phenotype marked by higher bone mass and bones of improved functional quality. Histomorphometric studies done before and after ovariectomy showed that the absence of osteocalcin leads to an increase in bone formation without impairing bone resorption. To our knowledge, this study provides the first evidence that osteocalcin is a determinant of bone formation.
Koshihara Y, Hoshi K, Ishibashi H, Shiraki M. Vitamin K2 promotes 1alpha,25(OH)2 vitamin De-induced mineralization in human periosteal osteoblasts. Calcif Tissue Int. 1996 Dec;59(6):466-73.
Lehto S, Niskanen L, Suhonen M, Ronnemaa T, Laakso M. Medial artery calcification. A neglected harbinger of cardiovascular complications in non-insulin-dependent diabetes mellitus. Arteriosler Thromb Vasc Biol. 1996 Aug;16(8):978-83.
Moore S. 1996. Blood vessels and lymphatics. In: Damjanov I, Linder J, editors. Anderson’s Pathology, 10th edn. St. Louis, Mosby, p. 1401.
Palmer G, Bonjour JP, Caverzasio J. Stimulation of inorganic phosphate transport by insulin-like growth factor I and vanadate in opossum kidney cells is mediated by distrinct protein tyrosine phosphorylation processes. Endrocrinology. 1996;137:4699-705.
Schinke T, Amendt C, Trindl A, Poschke O, Muller-Esterl W, Jahnen-Dechent W. The serum protein alpha2-HS glycoprotein/fetuin inhibits apatite formation in vitro and in mineralizating calvaria cells. A possible role in mineralization and calcium homeostasis. J Biol Chem. 1996 Aug;271(34):20789-96.
They present data suggesting that fetuin interferes with calcium salt precipitation. Fetuins inhibit apatite formation in both cell culture and in the test tube. Fetuins account for roughly half of the capacity of serum to inhibit salt precipitation.
Shearer MJ, Bach A, Kohlmeier M. Chemistry, nutritional sources, tissue distribution and metabolism of vitamin K with special reference to bone health. J Nutr. 1996;126(4 suppl): 1181S-1186S.
Both vitamin K1 and K2 are bioactive in hepatic gamma-carboxylation but long-chain vitamin K2 are less well absorbed. Liver stores of vitamin K are relatively small and predominantly are the menquinones 7-13. The hepatic reserves of vitamin K1 (approx 10% of total) are labile and turn over at a faster rate than menaquinones. Bone contains substantial concentrations of both. The majority (60-70%) of daily dietary intake of vitamin K1 is lost to the body by excretion, which emphasizes the need for a continuous dietary supply to maintain tissue reserves.
Thijssen HH, Drittij-Reijinders MJ. Vitamin K status in human tissues: tissue-specific accumulation of phylloquinone and menaquinone 4. Br J Nutr. 1996;75(1:121-7.
We measured the vitamin K status in postmortem human tissues (brain, heart, kidney, liver, lung, pancreas) to see if there is a tissue-specific distribution pattern. Phylloquinone (K1) was recovered in all tissues with relatively high levels in liver, heart and pancreas; low levels were found in brain, kidney and lung. Menaquinone-4 (MK-4) was recovered from most of the tissues; its levels exceeded the K1 levels in brain and kidney and equalled K1 in pancreas. Liver, heart and lung were low in MK-4. The higher menaquinones, MK-6-11, were recovered in the liver samples, traces of MK-6-9 were found in some of the heart and pancreas samples. The results show that in man there are tissue-specific, vitamin-K distribution patterns comparable to those in the rat. Furthermore, the accumulation of vitamin K in heart, brain and pancreas suggests a hitherto unrecognized physiological function of this vitamin.
Wheeler DC. Cardiovascular disease in patients with chronic renal failure. Lancet. 1996;348:1673-1674.
Amann K, Wolf B, Nichols C, Tornig J, Schwarz U, Zeier M, Mall G, Ritz E. Aortic changes in experimental renal failure: Hyperplasia or hypertrophy of smooth muscle cells? Hypertension. 1997;29:770-775.
Chertow GM, Burke SK, Lazarus JM, Stenzel KH, Wombolt D, Goldberg D, et al. Poly [allylaine hydrochloride] (RenaGel): a noncalcemic phosphate binder for the treatment of hhperphosphatemia in chronic renal failure. Am J Kidney Dis. 1997;299(1):66-71.
Dietary phosphate restriction and the oral administration of calcium and aluminum salts have been the principal means of controlling hyperphosphatemia in individuals with end-stage renal disease over the past decade. Although relatively well-tolerated, a large fraction of patients treated with calcium develop hypercalcemia, In this study they explored alternative binders.
Goldsmith DJ, Covic A, Sambrook PA, Ackrill P. Vascular calcification in long-term haemodialysis patients in a single unit: A retrospective analysis. Nephron. 1997;77(1):37-43.
We were able to analyze the natural history of VC and to determine which clinical parameters were linked with progression. We found that VC became steadily more prevalent-at dialysis onset present in 39% of the patients, with a mean onset 9.7 years after starting dialysis. As well as becoming more prevalent, the calcification became progressively more severe in most patients. There were two patterns of VC: axial (aorta and iliac and femoral arteries), seen alone in 32% of the patients, and peripheral (digital arteries), seen alone in 3% of patients. Most patients (65%) had evidence of both types. Better understanding of these pathological processes may permit intervention and possibly lead to a reduction in cardiovascular mortality.
Jahnen-Dechent W, Schinke T, Trindl A, et al. Cloning and targeted deletion of the mouse fetuin gene. J Biol Chem. 1997;272:31496-31503.
Kohlmeier M, Saupe J, Shearer MJ, Schaefer K, Asmus G. Bone health of adult hemodialysis patients is related to vitamin K status. Kidney Int. 1997;51:1218-21.
Bone health of adult hemodialysis patients is related to vitamin K status. Investigated 68 hemodialysis patients, ages 33 to 91, analyzed the association of biochemical indicators of vitamin K nutriture and bone metabolism, and related both to past bone fracture history and prospective bone fracture risk. Phylloquinone concentrations were significantly lower in the 23 patients with previous fractures and a smaller percentage of their serum osteocalin was carboxylated. The 41 patients who never had fractures had nearly three times higher phylloquinone concentrations. Concluded that suboptimal vitamin K nutriture in hemodialysis patient is associated both with increased bone fracture risk and a high prevalence of hyperparathyroidism.
Luo G, Ducy P McKee MD, Pinero GJ, Loyer E, Behringer RR, Karsenty G. Spontaneous calcification of arteries and cartilage in mice lacking matrix GLA protein. Nature. 1997 Mar;386(6620):78-81.
Matrix Gla protein is a mineral binding ECM (extracellular matrix) protein synthesized by vascular smooth-muscle cells and chondrocytes. Mice that lack MGP develop but die with two months from arterial calcification. Chondrocytes that elaborate a typical cartilage matrix can be seen in the affected arteries. The results indicate that ECM calcification must be actively inhibited in soft tissues.
Watson KE, Abrolat ML, Malone LL, Hoeg JM, Doherty T, Detrano R, Demer LL. Active serum vitamin D levels are inversely correlated with coronary calcification. Circulation. 1997 Sep;96(6):1755-60.
Block GA, Hulbert-Shearon TE, Levin NW, Port FK. Association of serum phosphorus and calcium x phosphate product with mortality risk in chronic hemodialysis patients: a national study. Am J Kidney Dis. 1998;31:607-617.
Coates T, Kirkland GS, Dymock RB, Murphy BF, Brealey JK, Mathew TH, Disney AP. Cutaneous necrosis from calcific uremic arteriolopathy. Am J Kidney Dis. 1998;32:384-391.
Davidson RT, Foley AL, Engelke JA, Suttie JW. Conversion of dietary phylloquinone to tissue menaquinone-4 in rats is not dependent on gut bacteria. J. Nutr. 1998;128(2):220-3.
Rats fed only phylloquinone (K1) showed increased tissue MK4 concentrations in the liver, heart, kidney, brain and salivary glands. This study offered conclusive proof that the tissue-specific formation of MK4 from vitamin K1 is a metabolic transformation that does not require bacterial transformation to menadione as an intermediate.
Ferland G. The vitamin K-dependent proteins: An update. Nutr Rev. 1998;56(8):223-30.
Historically known for its role in blood coagulation, vitamin K also has been shown to be required for the physiologic activation of numerous proteins that are not involved in hemostasis. Over the last 20 years, vitamin K-dependent proteins have been isolated in bone, cartilage, kidney, atheromatous plaque, and numerous soft tissues. Although the precise mechanism of action of many of these proteins remains to be determined, their discovery has proven important from a physiologic point of view.
Foley R, Parfrey P, Sarnak M. Epidemiology of cardiovascular disease in chronic renal disease. J Am Soc Nephrol. 1998 Dec 9;(Supplement12):S16-23.
Jono S, Nishizawa Y, Shioi A, Morii H. 1,25-Dihydroxyvitamin D3 increases in vitro vascular calcification by modulating secretion of endogenous parathyroid hormone-related peptide. Circulation. 1998;98:1302-1306.
Martinez I, Saracho R, Moina I, Montenegro J, Llach F. Is there a lesser hyperparathyroidism in diabetic patients with chronic renal failure? Nephrol Dial Transplant. 1998;13 (Suppl3:9-11.
Nagasawa Y, Fujii M, Kajimoto Y, Imai E, Hori M. Vitamin K2 and serum cholesterol in patients on continuous ambulatory dialysis. The Lancet. 1998a;351:724.
Nagasawa Y, Fujii M, Kajimoto Y, Imai E, Hori M. Vitamin K supplementation in patients on continuous ambulatory peritoneal dialysis. The Lancet. 1998b;352:1735. Authors reply.
Price PA, Faus SA, Williamson MK. Warfarin causes rapid calcification of the elastic lamellae in rat arteries and heart valves. Arterioscler Thromb Vasc Biol. 1998;18:1400-1407.
High doses of warfarin cause focal calcification in the media of major arteries and in aortic heart valves in as early as two weeks, and progressively increased. It appears that warfarin induces artery calcification by inhibiting carboxylation of matrix Gla protein.
Savage T, McMahon AC, Mullen AM, Nott CA, odd SM, Tribe RM, et al. Increased myogenic tone precedes structural changes in mild experimental uraemia in the absence of hypertension in rats. Clin Sci (Long). 1998; 95(6):681-6.
US Renal Data System: USRDS 1998 annual data report. Am J Kidney Dis. 1998;332:69-80.
Vychytil A, Druml W. Vitamin K supplementation in patients on continuous ambulatory peritoneal dialysis. The Lancet. 1999;351:1734– 1735.
Blacher J, Guerin AP, Pannier B, Marchais SJ, Safar ME, London GM. Impact of arotic stiffness on survival in end-stage renal disease. Circulation. 1999;99:2434-2439.
Bleyer AJ, Russell GB, Satko SG. Sudden and cardiac death rates in hemodialysis patients. Kidney Int. 1999;55(4):1553-9.
Lai M, Hung K, Huang J, et al. Clinical findings and outcomes of intra-hemodialysis cardiopulmonary resuscitation. Am J Nephrol. 1999;19:468-73.
Linderg JS, Moe SM. Osteoporosis in end-state renal disease. Semin Nephrol. 1999 Mar;19(2):115-22.
Prasad GV, Abidi SM, McCauley J, Johnston JR. Vitamin K deficiency with hemorrhage after kidney and combined kidney-pancreas transplantation. Am J Kidney Dis. 1999;33:963–965.
Rostand SG, Drueke, TB. Parathyroid hormone, vitamin D, and cardiovascular disease in chronic renal failure. Kidney Int. 1999;56(2):383-92.
Shanahan CM, Cary NR, Salisbury JR, Proudfoot D, Weissberg PL, Edmonds ME. Medial localization of mineralization-regulating proteins in association with Monckeberg’s sclerosis: Evidence for smooth muscle cell-mediated vascular calcification. Circulation. 1999;100(21):2168-76.
These data indicate that medial calcification in Monckeberg’s sclerosis lesions is an active process potentially orchestrated by phenotypically modified VSMCs.
Simon M, Maresh JG, Harris SE, Hernandez JD, Arar M, Olson MS, Abboud HE. Expression of bone morphogenetic protein-7mRNA in normal and ischemic adult rat kidney. Am J Physiol. 1999;276(3 Pt2):F382-9.
Tsaioun, KL. Vitamin K-dependent proteins in the developoing and aging nervous sytem. Nutr Rev. 1999 Aug;57(8):231-40.
The role of vitamin K in the brain has not been studied systematically. The discovery of the vitamin K dependent growth factor, Gas6, in the central nervous system, provides compelling evidence of a biologic role of vitamin K during the development of the nervous system. Gaining more knowledge of the biologic role of vitamin K, and specifically Gas6, in the brain may be important in understanding the development and aging of the nervous system.
Wada T, McKee MD, Steitz S, Giachelli CM. Calcification of vascular smooth muscle cell cultures: Inhibition by osteopontin. Circ Res. 1999 ;84(2):166-78.
2000
Alem AM, Sherrard DJ, Gillen DL, et al. Increased risk of hip fracture among patients with end-stage renal disease. Kidney Int. 2000;58:396-9.
Block GA, Port FK. Re-evaluation of risks associated with hyperphosphatemia and hyperparathyroidism in dialysis patients: Recommendations for a change in management. Am J Kidney Dis. 2000;35(6):1226-37.
Coco M, Rush H. Increased incidence of hip fractures in dialysis patients with low serum parathyroid hormone. Am J Kidney Dis. 2000;36:1115-21.
Goodman WG, Goldin J, Kuizon BD, Yoon C, Gales B, Sider D., et al. Coronary-artery calcifiÂÂÂÂcation in young adults with end-stage renal disease who are undergoing dialysis. N Engl J Med. 2000;342:1478–1483.
Guerin AP, London GM, Marchais SJ, Metvier F. Arterial stiffening and vascular calcifications in end-stage renal disease. Nephrol Dial Transplant. 2000;15(7):1014-21.
Jono, S, McKee MD, Murry CE, Shioi A, Nishizawa Y, Mori K, et al. Phosphate regulation of vascular smooth muscle cell calcification. Circ Res. 2000;87(7):E10-7.
Vascular calcification is a common finding in atherosclerosis and a serious problem in diabetic and uremic patients. Because of the correlation of hyperphosphatemia and vascular calcification, the ability of extracellular inorganic phosphate levels to regulate human aortic smooth muscle cell (HSMC) culture mineralization in vitro was examined. These data suggest that elevated phosphate may directly stimulate HSMCs to undergo phenotypic changes that predispose to calcification and offer a novel explanation of the phenomenon of vascular calcification under hyperphosphatemic conditions.
Rubenstein MH, Harrell LC, Sheynberg BV, Schunkert H, Bazari H, Palacios IF: Are patients with renal failure good candidates for percutaneous coronary revascularization in the new device era? Circulation. 2000;102(24):2966-2972.
Schwarz U, Buzello M, Ritz E et al. Morphology of coronary atherosclerotic lesions in patients with end-stage renal failure. Nephrol Dial Transplant 2000;15:218–223.
Shanahan CM, Proudfoot D, Tyson KL, Cary NR, Edmonds M, Weissberg PL. Expression of mineralization-regulating proteins in association with human vascular calcification. Z Kardiol. 2000;89 Suppl 2:63-8.
In association with both medial and intimal calcification, the temporal changes in expression of mineralisation-regulating proteins are similar. Some bone-associated proteins, including matrix Gla protein (MGP), are down-regulated in association with calcification while expression of a number of bone-associated proteins, not normally expressed in the vessel wall, are induced including alkaline phosphatase (ALK), bone sialoprotein (BSP) and bone Gla protein (BGP). In medial calcification the source of expression of these mineralisation-regulating proteins is VSMCs while in intimal lesions both VSMCs and macrophages express them. Furthermore, these bone-associated proteins are spontaneously expressed by VSMCs in vitro suggesting that human VSMCs are capable of simultaneously exhibiting smooth muscle and osteogenic-like properties. These studies imply that both medial and intimal ascular calcification are regulated processes; however the aetiology of each pathology differs.
Shearer MJ. Role of vitamin K and Gla proteins in the pathophysiology of osteoporosis and vascular calcification. Curr Opin Clin Nutr Metab Care. 2000;3:433-8.
Among the proteins in bone and vascular biology are several members of the vitamin K dependent Gla protein family. This review focuses on the role of osteocalcin and matrix Gla protein. Osteocalcin metabolism has been implicated in the pathogenesis of osteoporosis through a mechanism that may be linked to suboptimal vitamin K status resulting in its undercarboxylation and presumed dysfunction. Recent studies that have investigated this hypothesis are discussed, as are promising clinical studies of vitamin K supplementation in osteoporosis. A recently delineated function of matrix Gla protein is as a powerful inhibitor of calcification of arteries and cartilage. This review covers several landmark studies using cell systems, whole animals and genetic techniques that have consolidated and extended our knowledge of the role of matrix Gla protein in the prevention of ectopic calcification.
Shioi A, Mori K, Jono S, Wakikawa T, Hiura Y, Koyama H, et al. Mechanism of atherosclerotic calcification. Z Kardiol. 2000;89 Suppl 2:75.
Tukaj C, Kubasik-Juraniec J, Kraszpulski M. Morphological changes of aortal smooth muscle cells exposed to calcitriol in culture. Med Sci Monit. 2000;6(4):668-74.
Wallin R, Cain D, Hutson SM, Sane DC, Loeser R. Modulation of the binding of matrix Gla protein (MGP) to bone morphogenetic protein-2 (BMP-2). Thromb Haemost. 2000;84(6):1039-44.
Blacher J, Guerin AP, Pannier B, Marchais SJ, London GM. Arterial calcifications, arterial stiffness, and cardiovascular risk in end-stage renal disease. Hypertension. 2001;38:938–942.
Bostrom K, Tsao D, Shen S, Wang Y, Demer LL. Matrix GLA protein modulates differentiation induced by bone morphogenetic protein-2 in C3H10T1/2 cells. J Biol Chem. 2001;276:14044-52.
Chang L, Feng T, Li J, Dou C, Wei J, Yinghu G. Regulation of osteopontin expression in a rat model of urolithiasis. Chinese Medical J. 2001;114(8):829-832.
Investigated the relationship between the expression and regulation of osteopontin and kidney stones. Treated rats with vitamin D3, vitamin K, testosterone or estradiol for 7 days. The results showed that vitamin K, testosterone and estradiol up-regulated the expression of OPN mRNA and its protein, thus decreasing the precipitation of calcium oxalate in rat kidneys. D3, increased the concentration of calcium in urine and accelerated the sedimentation of calcium oxalate in rat kidneys. The findings indicated that vitamin K, testosterone and estradiol inhibit the formation of stones via up-regulating the expression of OPN in kidneys, while D3 overdose may accelerate the process.
Dhore CR, Cleutjens JP, Lutgens E, et al. Differential expression of bone matrix regulatory proteins in human atherosclerotic plaques. Arterioscler Thromb Vasc Biol. 2001;21:1998-2003.
Ganesh SK, Stack AG, Levin NW, Hulbert-Shearon T, Port FK. Association of elevated serum PO 4 , Ca, PO 4 product, and parathyroid hormone with cardiac mortality risk in chronic hemodialysis patients. J Am Soc Nephrol. 2001;12:2131–2138.
Gopalakrishnan R, Ouyang H, Somerman MJ, McCauley LK, Franceschi RT. Matrix gamma-carboxyglutamic acid protein is a key regulator of PTH-mediated inhibition of mineralization in MC3T3-E1 osteoblast-like cells. Endocrinology. 2001;142:4379-88.
Guerin AP, Blacher J, Pannier B, Marchais SJ, Safar ME, London GM. Impact of aortic stiffness attenuation on survival of patients in end-stage renal failure. Circulation. 2001;103:987-992.
Iwamoto J, Takeda T, Ichimura S. Effect of menatetrenone on bone mineral density and incidence of vertebral fractures in postmenopausal women with osteoporosis: a comparison with the effect of etidronate. J Orthop Sci. 2001;6(6):487-92.
Miyake N, Hoshi K, Sano Y, Kikuchi K, Tadano K, Koshihara Y. 1,25-Dihydroxyvitamin D3 promotes vitamin K2 metabolism in human osteoblasts. Osteoporos Int. 2001;12(8):680-7.
Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY, et al. Effect of parathyroid hormone (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med. 2001 May;344(19):1434-41.
Newman B, Gigout LI, sudre L, Grant ME, Wallis GA. Coordinated expression of matrix Gla protein is required during endochondral ossification for chondrocyte survival. J Cell Biol. 2001;154(3):659-66.
Schurgers LJ, Dissel PE, Spronk HM, Soute BA, Dhore CR, Cleutjens JP, et al., Role of vitamin K and vitamin K-dependent proteins in vascular calcification. Z Kardio. 2001;90Suppl 3:57-63.
This is the first report demonstrating the association between MGP and vascular calcification. The hypothesis is put forward that undercarboxylation of MGP is a risk factor for vascular calcification and that the present RDA values are too low to ensure full carboxylation of MGP.
Schwarz U, Buzello M, Ritz E et al. Morphology of coronary atherosclerotic lesions in patients with end-stage renal failure. Nephrol Dial Transplant 2000;15:218–223.
Steitz SA, Speer MY, Curinga G, Yang HY, Haynes P, Aebersold R, et al. Smooth muscle phenotypic transition associated with calcification: upregulation of Cbfa1 and downregulation of smooth muscle lineage markers. Circ Res. 2001;89(12):1147-54.
Suwelack B, Gerhardt U, Witta J, et al. Effect of parathyroid hormone levels on carotid intima media thickness after renal transplantation. Am J Hypertens. 2001;14:1012-1018.
Beddhu S, Allen-Brady K, Cheung AK, et al: Impact of renal failure on the risk of myocardial infarction and death. Kidney Int. 2002; 62(5):1776-1783.
Canfield AE, Farrington C, Dziobon MD, Boot-Handford RP, Heagerty AM, et al. The involvement of matrix glycoproteins in vascular calcification and fibrosis: an immunohistochemical study. J Pathol. 2002;196(2):228-34.
Cannata-Andia JB and Gomez Alonso C. Vitamin D deficiency: a neglected aspect of disturbed calcium metabolism in renal failure. Nephrol Dial Transplant. 2002;17(11):1875-8.
Chen X, Kidder LS, Lew WD. Osteogenic protein-1 induced bone formation in an infected sesgmental defect in the rat femur. J Orthop Res. 2002;20(1):142-50.
Chertow GM, Burke SK, Raggi P. Sevelamer attenuates the progression of coronary and aortic calcification in hemodialysis patients. Kidney Int. 2002;62:245-252.
Crowther MA, Clase CM, Margetts PJ, Julian J, Lambert K, Sneath D, Nagai R, Wilson S, Ingram AJ. Low-intensity warfarin is ineffective for the prevention of PTFE graft failure in patients on hemodialysis: A randomized controlled trial. J Am Soc Nephrol. 2002;13:2331–2337.
Elder G. Pathophysiology and recent advances in the managementof renal osteodystrophy. J Bone Miner Res. 2002;17(12):2094-105.
Jara A, Chacon C, Felsenfeld AJ. Hyperphosphatemia modestly retards parathyroid hormone suppression during calcitriol-induced hypercalcemia in normal and azotemic rats. Nephron. 2002;92(4):883-8.
Kato A, Yasuda H, Togawa A, et al. Measurement of des-gamma-carboxy prothrombin levels in hemodialysis patients positive for anti-hepatitis virus C antibody. Clin Nephrol. 2002; 58: 296–300.
Malyszyko J, Wolczynski S, Skrzydlewska E, Malyszko JS, Mysliwiec M. Vitamin K status in relation to bone in patients with renal failure. Am J Nephrol. 2002;22:504-8.
Vitamin K abnormalities may be involved in the pathogenesis of bone disease in patients with advanced renal failure since vitamin K plays a role in the synthesis of osteocalcin, a marker of bone formation. Vitamin K may also indirectly suppress parathyroid function. The aim of this study was to evaluate vitamin K status in patients with renal failure and in healthy volunteers in relation to some biochemical markers of bone turnover. We found that vitamin K concentrations did not differ significantly between all the groups studied. Only in renal failure patients was the vitamin K concentation low, almost reaching statistical significance when compared to the healthy volunteers (p = 0.05) and correlated positively with age, serum calcium and osteonectin. In patients after renal replacement therapy, the only significant positive correlation was found between phylloquinne and osteonectin (r = 0.027, p = 0.004). The same applied when we also included healthy volunteers.
Moe SM, O’Neill KD, Duan D, Ahmed S, Chen NX, Leapman SB, et al. Medial artery calcification in ESRD patients is associated with deposition of bone matrix proteins. Kidney Int. 2002;61:638-647.
In patients with ESRD undergoing renal transplantation, their research found that vascular calcification of the medial layer of the inferior epigastric artery is common (44%), can be detected by spiral CT, and is associated with deposition of bone matrix proteins. This implies an active cell-mediated process, raising hope that directed intervention can arrest this process.
Muntner P, He J, Hamm L, Loria C, Whelton PK: Renal insufïciency and subsequent death resulting from cardiovascular disease in the United States. J Am Soc Nephrol. 2002;13(3):745-753.
National Kidney Foundation (2002). K/DOQI clinical practice guidelines for chronic kidney disease. Retrieved 2013-6-29.
Naveh-Many T, Bell O, Silver J, Kilav R. Cis and Trans acting factors in the regulation of parathyroid hormone (PTH) mRNA stability by calcium and phosphate. FEDBS LETT. 2002;529(1):60-4.
Oh J, Wunsch R, Turzer M, Bahner M, Raggi P, Querfeld U, Mehls O, Schaefer F. Advanced coronary and carotid arteriopathy in young adults with childhood-onset chronic renal failure. Circulation. 2002;106:100 –105.
Proudfoot.D, Davies JD, Skepper JN, Weissberg PL, Shanahan CM. Acetylated low-density lipoprotein stimulates human vascular smooth muscle cell calcification by promoting osteoblastic differentiation and inhibiting phagocytosis. Circulation. 2002 Dec;106(2):3044-50.
Raggi P, Boulay A, Chasan-Taber S, Amin N, Dillon M, et al. Cardiac calcification in adult hemodialysis patients. A link between end-stage renal disease and cardiovascular disease? J Am Coll Cardiol. 2002;39:695-701.
Rebsamen MC, Sun J, Norman AW, Liao JK. 1alpha,25-dihydroxyvitamin D3 induces vascular smooth muscle cell migration via activation of phosphatidylinositol 3-kinase. Circ Res. 2002;91(1):17-24.
Sugimoto T, Yamakado M, Matsushita K, Iwamoto T, Tagawa H. Pharmacodynamics of menatetrenone and effects on bone metabolism in continuous ambulatory peritoneal dialysis patients. J Int Med Res. 2002;30:566-75.
They administered 15 mg of vitamin K2 to ambulatory peritoneal dialysis patients for twelve months. No side effects with giving vitamin K to CKD patients. Felt that the K2 protected against bone mineral loss.
Schurgers LJ, Vermeer C. Differential lipoprotein transport pathways of K-vitamins in healthy subjects. Biochim Biophys Acta. 2002;1570:27-32.
Researched whether the distribution pattern of K1 and K2 can be explained by the different liposolubility of the K vitamers, leading to different lipoprotein particles. They found that during the first four hours after intake, all K-vitamins were associated predominantly with triacylglycerol-rich lipoprotein (TGRLP) fraction, which is mainly cleared by the liver. In contrast to K1, both MK4 and MK9 were found in TGRLP and in low-density lipoproteins and MK4 was even present in high-density lipoprotein.
National Academy of Sciences, Institute of Medicine, Food and Nutrition Board (2001). Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. National Academy Press, Washington, D.C.
Ushiroyama T, Ikeda A, Ueki M. Effect of continuous combined therapy with vitamin K(2) and vitamin D(3) on bone mineral density and coagulofibrinolysis function in postmenopausal women. Maturitas. 2002;41(3):211-21.
Gave postmenopausal women combined therapy with vitamin K2 and vitamin D for two years and found markedly increased bone mineral density, more than when gave vitamin K2 alone, or vitamin D alone.
Virmani R, Burke AP, Kolodgie FD, Farb A. Vulnerable plaque: the pathology of unstable coronary lesions. J Interv Cardiol. 2002:15(6):439-46.
Vliegenthart R, Hollander M, Breteler MM et al. Stroke is associated with coronary calcification as detected by electron-beam CT: the Rotterdam Coronary CalcifÂÂÂÂcation Study. Stroke. 2002;33:462–465.
Zebboudj AF, Imura M, Bostrom K. Matrix GLA protein, a regulatory protein for bone morphogenetic protein-2. J Biol Chem. 2002;277(6):4388-94.
Bursztyn M, Motro M, Grossman E, et al. Accelerated coronary artery calcification in mildly reduced renal function of high-risk hypertensives: a 3-year prospective observation. Journal of Hypertension. 2003;21:1953-59.
Chen J, Liu J, Zhang Y, Ye Z, Wang S. Decreased renal vitamin K-dependent gamma-glutamyl carboxylase activity in calcium oxalate calculi patients. Chin Med J. 2003;116(4):569-72.
Studied the activity of vitamin K-dependent carboxylase, and found significantly reduced activity in urolithic patients.
Collins AJ. Cardiovascular mortality in end-stage renal disease. Am J Med Sci. 2003;325:13—167.
Davies MR, Lund RJ, Hruska KA. BMP-7 is an efficacious treatment of vascular calcification in a murine model of atherosclerosis and chronic renal failure. J Am Soc Nephrol. 2003;14(6):1559-67.
Studied uremic animals and treated them with BMP-7. Expression of osteocalcin was assessed and it was shown that is is increased in untreated uremic animals but downregulated to levels similar to non-uremic control animals with treatment. The data demonstrates the efficacy of BMP-7 as a potential treatment of vascular calcification.
Essalihi R, Dao HH, Yamaguchi N, Moreau P. A new model of isolated systolic hypertension induced by chronic warfarin and vitamin K1 treatment. Am J Hypertens. 2003;16(2):103-10.
Fried LF, Shlipak MG, Crump C, et al: Renal insuffiÂÂÂÂciency as a predictor of cardiovascular outcomes and mortality in elderly individuals. J Am Coll Cardiol. 2003;41(8):1364-1372.
Heiss A, Cu Chesne A, Denecke B, Grotzinger J, Yamamoto K, Renne T, et al., Structural basis of calcification inhibition by alpha 2-HS glycoprotein/fetuin-A. Formation of colloidal calciprotein particles. J Biol Chem. 2003;278(15):13333-41.
Iwamoto J, Yeh JK, Takeda T, Ichimura S, Sato Y. Comparative effects of vitamin K and vitamin D supplementation on prevention of osteopenia in calcium-deficient young rats. Bone. 2003 Oct;33(4):557-66.
This study shows the differential effects of vitamin K and vitamin D supplementation on the development of osteopenia in young rats under mild calcium deficiency. Vitamin K supplementation stimulates renal calcium reabsorption, increases maturation-related cancellous bone gain, and retards the reduction in maturation-related cortical bone gain, whereas vitamin D supplementation stimulates intestinal calcium absorption and prevents the reduction in maturation-related periosteal bone gain by inducing accumulation of calcium from cancellous and endocortical bone.
Ketteler M, Bongartz P, Westenfeld R, et al. Association of low fetuin-A (AHSG) concentrations in serum with cardiovascular mortality in patients on dialysis: a cross-sectional study. Lancet. 2003;361:827-833.
Ketteler M, Wanner C, Metzger T, Bongartz P, Westenfeld R, Gladziwa U, Schurgers LJ, Vermeer C, Jahnen-Dechent W, Floege J. Deficiencies of calcium-regulatory proteins in dialysis patients: a novel concept of cardiovascular calcification in uremia. Kidney Int. 2003;84(suppl): S84 –S87.
The correction of hyperphosphatemia was the central target for preventive therapeutic intervention. Recent studies in knockout mice, point to the possibility that deficiencies in calcium-regulatory proteins may represent important pathomechanisms leaving to extraosseous calcifications ( those in tissue rather than bones).
Ketteler M, Bongartz P, Westenfeld R, Wildberger JE, Mahnken AH, Bohm R, Metzger T, Wanner C, Jahnen-Dechent W, Floege J.: Association of low fetuin-A (AHSG) concentrations in serum with cardiovascular mortality in patients on dialysis: A cross-sectional study. Lancet. 2003;361:827–833.
Klawansky S, Komaroff E, Cavanaugh Jr PF et al. Relationship between age, renal function and bone mineral density in the US population. Osteoporos Int. 2003;14:570–576.
Kronenberg F, Mundle M, Langle M, et al. Prevalence and progression of peripheral arterial calcifications in patients with ESRD. Am J Kidney Dis. 2003;41:140-148.
London G, Guerin A, Marchais S, Metivier F, Pannier B, Adda H. Arterial media calcification in end-stage renal disease: Impact on all-cause and cardiovascular mortality. Nephrol Dial Transplant. 2003;18:1731-1740.
Manjunath G, Tighiouart H, Ibrahim H, et al. Level of kidney function as a risk factor for atherosclerotic cardiovascular outcomes in the community. J Am Coll Cardiol. 2003;41(1):47-55.
Moe SM, Duan D, Doehle BP et al. Uremia induces the osteoblast differentiation factor Cbfa1 in human blood vessels. Kidney Int. 2003;63:1003–1011.
Moe SM, Drueke TB. Management of secondary hyperparathyroidism: The importance and the challenge of controlling parathyroid hormone levels without elevating calcium, phosphorus, and calcium-phosphorus product. Am J Nephrol. 2003;23(6):369-79.
Owda A, Elhwairis H, Narra S, Towery H, Osama S. Secondary hyperparathyroidism in chronic hemodialysis patients: Prevalence and race. Ren Fail. 2003;25(4):595-602.
Spronk HM, Soute BA, Schurgers LJ, Thijssen HM, De Mey JG, Vermeer C. Tissue-specific utilization of menaquinone-4 results in the prevention of arterial calcification in warfarin-treated rats. J Vasc Res. 2003;40(6):531-7.
Warfarin-treated rats were fed diets containing K1, MK-4, or both. Both K1 and MK-4 are cofactors for the endoplasmic reticulum enzyme gamma-glutamyl carboxylase but have a structurally different aliphatic side chain. Despite their similar in vitro cofactor activity, they show that MK-4 and not K1 inhibits warfarin-induced arterial calcification. The total hepatic K1 accumulation was threefold higher than that of MK-4, whereas aortic MK-4 was three times that of K1. K1 and MK-4 were both equally utilized in the liver, but the aorta showed a more efficient utilization of MK-4. Therefore, the observed differences between K1 and MK-4 with respect to inhibition of arterial calcification may be explained by both differences in their tissue bioavailability and cofactor utilization in the reductase/carboxylase reaction.
Sweatt A, Sane DC, Hutson SM, Wallin R. Matrix Gla protein (MGP) and bone morphogenetic protein-2 in aortic calcified lesions of aging rats. J Thromb Haemost. 2003;1(1):178-85.
The vitamin K-dependent protein, matrix Gla protein (MGP) is a binding protein for bone morphogenetic protein-2 (BMP-2). Immunohistochemistry showed that calcified lesions in the aortic wall of aging rats contained elevated concentrations of MGP that was poorly gamma-carboxylated and did not bind BMP-2. Age-related arterial calcification may be a consequence of under-gamma-carboxylation of MGP, allowing unopposed BMP-2 activity.
Block GA, Klassen PS, Lazarus JM, et al: Mineral metabolism, mortality, and morbidity in maintenance hemodialysis. J Am Soc Nephrol. 2004;15:2208–2218.
Go AS, Chertow GM, Fan D, McCulloch, CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Eng J Med. 2004;351:1296-1305.
This review evaluates the current evidence about the clinical and subclinical cardiovascular consequences associated with chronic kidney disease of varying levels of severity. In addition, it discusses the predictors of adverse cardiovascular outcomes while also focusing on recent insights into the relationships between chronic kidney disease and cardiovascular disease from the Chronic Renal Insufficiency Cohort Study.
Hao J, Zou B, Narayanan K, George A. Differential expression patterns of the dentin matrix proteins during mineralized tissue formation. Bone. 2004;34(6):932-32.
Moe SM, Duan D, Doehle BP et al. Uremia induces the osteoblast differentiation factor Cbfa1 in human blood vessels. Kidney Int 2003;63:1003–1011.
Schäfer C, Heiss A, Schwarz A, Westenfeld R, Ketteler M, Floege J, Muller-Esterl W, Schinke T, Jahnen-Dechent W. The serum protein alpha 2-Heremans-Schmid glycoprotein/fetuin-A is a systemically acting inhibitor of ectopic calcification. J Clin Invest. 2003;112:357–366.
Sprague SM, Llach F, Amdahl M, Taccetta C, Batile D. Paricalcitol versus calcitriol in the treatment of secondary hyperparathyroidism. Kidney Int. 2003;63(4):1483-90.
Wang AY, Wang M, Woo J, Lam CW, Li PK, Lui SF, Sanderson JE.: Cardiac valve calcification as an important predictor for all-cause mortality and cardiovascular mortality in long-term peritoneal dialysis patients: A prospective study. J Am Soc Nephrol. 2003;14:159–168.
Zebboudj AF, Shin V, Bostrom K. Matrix GLA protein and BMP-2 regulate osteoinduction in calcifying vascular cells. J Cell Biochem. 2003;90(4):756-65.
Abedin M, Tintut Y, Demer LL. Vascular Calcification: Mechanisms and clinical ramifications. Arterioscler Thromb Vasc Biol. 2004;24(7):1161-70.
Vascular calcification, long thought to result from passive degeneration, involves a complex, regulated process of biomineralization resembling osteogenesis. Evidence indicates that proteins controlling bone mineralization are also involved in the regulation of vascular calcification. Artery wall cells grown in culture are induced to become osteogenic by inflammatory and atherogenic stimuli. Furthermore, osteoclast-like cells are found in calcified atherosclerotic plaques, and active resorption of ectopic vascular calcification has been demonstrated. Call for further understanding to yield new therapeutic options.
Adragao T, Pires A, Lucas C, Birne R, Magalhaes L, Goncalves M, Negrao AP.: A simple vascular calcification score predicts cardiovascular risk in haemodialysis patients. Nephrol Dial Transplant. 2004;19:1480–1488.
Block GA, Klassen PS, Lazarus JM, Ofsthun N, Lowrie EG, Chertow GM. Mineral metabolism, mortality, and morbidity in maintenance hemodialysis. J Am Soc Nephrol. 2004;15:2208 –2218.
Chertow GM, Raggi P, Chasen-Taber S, Bommer J, Holzer H, Burke SK. Determinants of progressive vascular calcification in hemodialysis patients. Nephrol Dial Transplant. 2004;19:1489-1496.
Calcium-based phosphate binders are associated with progressive coronary artery and aortic calcification, especially when mineral metabolism is not well controlled. Calcium may directly or indirectly (via PTH) adversely influence the balance of skeletal and extraskeletal calcification in hemodialysis patients.
Chowdhury UK, Airan B, Mishra PK, Kothari SS, Subramaniam GK, Ray R, et al. Histopathology and morphometry of radial artery conduits: basic study and clinical application. Ann Thorac Surg. 2004;78(5):1614-21.
Cunningham J, Sprague SM, Cannata-Andia J, et al. Osteoporosis in chronic kidney disease. Am J Kidney Dis. 2004;43:566-571.
Giachelli CM. Vascular calcification mechanisms. J Am Soc Nephrol. 2004; 15: 2959–2964.
Geleijnse JM, Vermeer C, Grobbee DE, Schurgers LJ, Knapen MH, et al. Dietary intake of menaquinone is associated with a reduced risk of coronary heart disease: the Rotterdam Study. J Nutr 2004;134:3100–3105.
Vitamin K-dependent proteins, including matrix Gla-protein, have been shown to inhibit vascular calcification. Activation of these proteins via carboxylation depends on the availability of vitamin K. We examined whether dietary intake of phylloquinone (vitamin K-1) and menaquinone (vitamin K-2) were related to aortic calcification and coronary heart disease (CHD) in the population-based Rotterdam Study. Vitamin K2 was not related to any of the outcomes and the findings suggest that an adequate intake of menaquinone could be important for CHD prevention.
Go AS, Chertow GM, Fan D, McCulloch, CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Eng J Med. 2004;351:1296-1305.
Gonzalez EA, Sachdeva A, Oliver DA, Martin KJ. Vitamin D insufficiency and deficiency in chronic kidney disease. A single center observational study. Am J Nephrol. 2004;24(5):503-10.
Goodman WG, London G, Amann K, Block GA, Giachelli C, Hruska KA, et al. Vascular calcification in chronic kidney disease. Am J Kid Dis. 2004;43(3):572-579.
There is now abundant evidence that a variety of proteins normally involved in bone and mineral metabolism can be expressed in arterial tissue. These may influence the process of arterial calcifiÂÂÂÂcation. Matrix Gla-protein (MGP) plays a crucial role in preventing the calcifiÂÂÂÂcation of arteries and epiphyseal growth plate cartilage during embryonic and postnatal development, and is a vitamin K dependent protein. An ongoing effort should be undertaken to educate clinicians and nephrologists about calcification inhibitors.
Jono S, Ikari Y, Vermeer C, Dissel P, Hasegawa K, Sioi A, et al. Matrix Gla protein is associated with coronary artery calcification as assessed by electron-beam computed tomography. Thromb Haemost. 2004;91(4):790-4.
They found serum MGP levels to be inversely correlated with the severity of coronary artery calcification, suggesting a role for MGP in the development of vascular calcification.
London GM, Marchais SJ, Guerin AP. Arterial stiffness and function in end-stage renal disease. Adv Chronic Kidney Dis. 2004;11(2):202-9.
Malyszko JS, MaÅ‚yszko J, Skrzydlewska E, Pawlak K, MyÅ›liwiec M. Protein Z and vitamin K in kidney disease. Rocz Akad Med Bialmyst. 2004;49:197–200.
Matsuoka M, Iseki K, Tamashiro M, et al. Impact of high coronary artery calcification score (CACS) on survival in patients on chronic hemodialysis. Clin and Experim Nephrol. 2004;8:54-58.
McCullough, PA, Sandberg KR, Dumler F, Yanez JE. Determinants of coronary vascular calcification in patients with chronic kidney disease and end-stage renal disease: A systematic review. J Nephrol. 2004;17(4):205-15.
Mehrotra R, Budoff M, Christenson P, et al: Determinants of coronary artery calcification in diabetics with and without nephropathy. Kidney Int 2004;66:2022–2031.
Melaragno MG, Cavet ME, Yan C, Tai LK, Jin ZG, Haendeler J, Berk BC. Gas6 inhibits apoptosis in vascular smooth muscle: Role of Axl kinase and Akt. J. Mol. Cell Cardiol. 2004;37:881-887.
Murshed M, Schinke T, McKee MD, Karsenty G. Extracellular matrix mineralization is regulated locally; Different roles of two Gla-containing proteins. J Cell Biol. 2004;165:625-30.
Nakashima A, Yorioka N, Doi S, Masaki T Ito T, Harada S. Effects of vitamin K2 in hemodialysis patients withlow serum parathyroid hormone levels. Bone. 2004;34(3):579-83.
In patients with adynamic bone disease, the bone contains few osteoblasts and bone turnover is slow. The decrease of bone remodeling may also decrease the capacity of bone to buffer calcium, leaning to an increase in calcium x phosphate produce and increased risk of arterial calcification. They investigated vitamin K2 (MK4) on dialysis patients. Changes in bone metabolism markers suggested that vitamin K2 therapy can improve bone remodeling in dialysis patients with lower serum parathyroid levels.
O’Hare AM, Glidden DV, Fox CS, Hsu CY. High prevalence of peripheral arterial disease in persons with renal insufficiency: Results from the National Health and Nutrition Examination Survey 1999-2000. Circulation. 2004;109(3):320-3.
Price PA, Williamson MK, Nguyen TMT, Than TN. Serum levels of the Fetuin-mineral complex correlate with artery calcification in the rat. J Biol Chem. 2004;279(3):1594-600.
Raggi P, Bommer J, Chertow GM. Valvular calcification in hemodialysis patients randomized to calcium-based phosphorus binders or sevelamer. The Journal of Heart Valve Disease 2004;13:134-141.
Ritz E. Managing mineral balance in end-stage renal disease. Nephrol Dial Transplant. 2004;19(Supple 1):i1-i3.
Schurgers LJ, Aebert H, Vermeer C, Bultmann B, Janzen J. Oral anticoagulant treatment: friend or foe in cardiovascular disease. Blood. 2004;194:3231-2.
Calcification is a common complication in cardiovascular disease. Matrix γ-carboxyglutamic acid (Gla) protein (MGP) is a potent inhibitor of vascular calcification, the activity of which is regulated by vitamin K. In animal models, vitamin K antagonists, such as warfarin (oral anticoagulants [OACs]) were shown to induce arterial calcification. To investigate whether long-term OAC treatment may induce calcification in humans also, we have measured the grade of aortic valve calcification in patients with and without preoperative OAC treatment. OAC-treated subjects were matched with nontreated ones for age, sex, and disease. Calcifications in patients receiving preoperative OAC treatment were significantly (2-fold) larger than in nontreated patients.
Stevens LA, Levin A. Translating research findings of chronic kidney disease management to clinical practice: Challenges and opportunities. Adv Ren Replace Ther. 2004;11(1):66-75.
Thompson GR, Partridge J. Coronary calcification score: The coronary-risk impact factor. Lancet. 2004;363(9408):557-9.
Wallin R, Hutson SM. Warfarin and the vitamin K-dependent gamma-carboxylation system. Trends Mol Med. 2004;10:299-302.
Yang H, Curinga G, Giachelli CM. Elevated extracellular calcium levels induce smooth muscle cell matrix mineralization in vitro. Kidney Int. 2004;66:2293-2299. Hyperphosphatemia, elevated calcium x phosphorous and calcium burden , major causes of vascular calcification, are correlated with increased cardiovascular morbidity and mortality in dialysis patients. They conclude that elevated calcium may stimulate smooth muscle cells to mineralize, leading to accelerated and increased calcification.
Asmus HG, Braun J, Krause R, Brunkhorst R, Holzer, Schul W, et al. Two year comparison of sevelamer and calcium carbonate effects on cardiovascular calcification and bone density. Nephrol Dial Transplant. 2004 Aug;20(8):1653-61.
This two year study shows that calcium carbonate use is continuously associated with progressive arterial calcification in hemodialysis patients. In addition, it suggests that it is also associated with decresed bone density.
Barreto DV, Barreto FC, Carvalho AB, Cuppari L, Cendoroglo M, Draibe SA, et al: Coronary calcification in hemodialysis patients: the contribution of traditional and uremia-related risk factors. Kidney Int 2005;67:1576–1582.
Bischoff-Ferrari HA, Zhang Y, Kiel DP, Felson DT. Positive association between serum 25-hydroxyvitamin D level and bone density in osteoarthritis. Arthritis Rheum. 2005;53(6):821-6.
Block GA, Spiegel DM, Ehrlich J, et al. Effects of sevelamer and calcium on coronary artery calcification in patients new to hemodialysis. Kidney Int. 2005;68:1815-1824.
Clowes JA, Riggs BL, Khosla S. The role of the immune system in the pathophysiology of osteoporosis. Immunol Rev. 2005;208:207-27.
Davies MR, Lund RJ, Mathew S, Hruska KA. Low turnover osteodystrophy and vascular calcification are amenable to skeletal anabolism in an animal model of chronic kidney disease and the metabolic syndrome. J Am Soc Nephrol. 2005;16(4):917-28.
Giachelli CM, Speer MY, Li X, Rajachar RM, Yang H. Regulation of vascular calcification: Roles of phosphate and osteopontin. Circ Res. 2005;96(7):717-22.
Moe SM, Reslerova M, Ketteler M, et al: Role of calcification inhibitors in the pathogenesis of vascular calcification in chronic kidney disease. Kidney Int. 2005;67:2295–2304.
The majority of patients with chronic kidney disease (CKD) have excessive vascular calcification; however, most studies demonstrate that a subset of CKD patients do not have, nor develop, vascular calcification despite similar exposure to the uremic environment. This suggests protective mechanisms, or naturally occurring inhibitors, of calcification may be important. These data demonstrate that three inhibitors, fetuin-A, OPG, and MGP play an important role in the pathogenesis of uremic vascular calcification.
Ishimura E, Shioi A. Mechanism of arterial calcification with regards to atherosclerotic calcificiation and medial artery calcification. Clin Calcium. 2005;15(7):137-42.
Ivanovski O, Szumilak D, Nguyen-Khoa T, Dechaux M, Massy ZA, Phan O, et al. Dietary salt restriction accelerates atherosclerosis in apolipoprotein E-deficient mice. Atherosclerosis. 2005;280(2):271-6.
Ketteler M, Gross, M-L, Ritz, E. Calcification and cardiovascular problems in renal failure. Kidney Int. 2005;47:S-120-S127.
Calcification outside of the bone has plagued management of renal failure since the beginning of hemodialysis, but was neglected because the impact on survival was thought to be limited. Recognition that hyperphostemia is associated with and a predictor of all –cause mortality has transformed the situation. Stringent guidelines have been proposed for the management of hyperphosphatemia. Vascular calcification impacts cardiac death not only by complicating coronary atherosclerosis, but also by increasing the stiffness of central arteries. Recent studies show that hyperphostamea is also mediated by an active process and is modulated by calcification inhibitors.
Ketteler M, Westenfeld R, Schlieper G, Brandenburg V, Floege J. “Missing” inhibitors of calcification: general aspects and implications in renal failure. Pediatr Nephrol. 2005;20:383–388.
Mechanisms inhibiting precipitation must be operative to prevent extraosseous calcification. A number of local and systemic calcification inhibitors, including fetuin-A, matrix Gla protein, and osteoprotegerin, have been identified in recent years. The biological and clilnical roles of deficiency and dysregulation of calcification inhibition in uremia are reviewed.
Ketteler M, Westenfeld R, Schlieper G, Brandenburg V. Pathogenesis of vascular calcification in dialysis patients. Clin Exp Nephrol. 2005;9: 265–270.
Koos R, Mahnken AH, Muhlenbruch G, Brandenburg V, Pflueger B, Wildberger JE, Kuhl HP.: Relation of oral anticoagulation to cardiac valvular and coronary calcium assessed by multislice spiral computed tomography. Am J Cardiol. 2005;96:747–749.
K/DOQI clinical practice guidelines for bone metabolism and disease in children with chronic kidney disease. Am J Kidney Dis. 2005;46(Suppl 1):121-33.
London GM, Marchais SU, Geurin AP, Metivier F. Arterioslerosis, vascular calcifications and cardiovascular disease in uremia. Current Opion in Nephr & Hypert. 2005 Nov;14(6):525-531.
Arterial calcification in chronic kidney disease (CKD) is associated with increased cardiovascular risk. The mechanisms responsible for arterial calcification include alterations of mineral metabolism and expression of mineral-regulating proteins. Arterial calcification is similar to bone formation, involving differentiation of vascular smooth muscle cells (VSMCs) into phenotypically distinct osteoblast-like cells. Elevated phosphate and/or calcium trigger calcium precipitates in VSMC in vitro. The presence of serum prevents these changes, indiciating the presence of calcification inhibitors. Arterial disease in CKD patients is characterized by extensive calcification. Evidence has accumulated pointing to the active and regulated nature of the calcification process.
Moe SM, Reslerova M, Ketteler M, O'neill K, Duan D, et al. Role of calcification inhibitors in the pathogenesis of vascular calcification in chronic kidney disease (CKD). Kidney Int. 2005;67:2295–2304.
National Kidney Foundation. K/DOQI clinical practice guidelines for bone metabolism and disease in children with chronic kidney disease. Am J Kidney Dis. 2005;46(Suppl 1):S1–S103.
Ninomiya T, Kiyohara Y, Kubo M, et al: Chronic kidney disease and cardiovascular disease in a general Japanese population : the Hisayama Study. Kidney Int. 2005;68(1):228-236.
Norman PE, Powell JT. Vitamin D, shedding light on the development of disease in peripheral arteries. Arterioscler Thromb Vasc Biol. 2005;25(1):39-46.
Odamaki M, Shibata T, Takita T, Kumagai H: Serum fetuin-A and aortic calcification in hemodialysis patients. Kidney Int. 2005; 68: 2915.
Pannier B, Guerin AP, Marchais SJ, Safar ME, London GM. Stiffness of capacitive and conduit arteries: prognostic significance for end-stage renal disease patients. Hypertension. 2005;45(4):592-6.
Qunibi WY. Reducing the burden of cardiovascular calcification in patients with chronic kidney disease. J Am Soc Nephrol. 2005; 16 Supple2:S95-102.
Raggi P, James G, Burke SK, et al. Decrease in thoracic vertebral bone attenuation with calcium-based phosphate binders in hemodialysis. J Bone Miner Res. 2005;20:764-772.
Rattazzi M, Bennett BJ, Bea F, Kirk EA, Ricks JL, Speer M, et al. Calcification of advanced atherosclerotic lesions in the innominate arteries of ApoE-deficient mice: potential role of chondrocyte-like cells. Arterioscler Thromb Vasc Biol. 2005;25(7):1420-5.
Razzaque M, St-Arnaud R, Taguchi T, Lanske B. FGF-23, vitamin D and calcification: The unholy triad. Nephrol Dial Transplant. 2005;20:2032-2035.
Reynolds JL, Skepper JN, McNair R, Kasama T, Gupta K, Weissberg PL, et al., Multifunctional roles for serum protein fetuin-a in inhibition of human vascular smooth muscle cell calcification. J Am Soc Nephrol. 2005;16(10):2920-30.
Sasaki N, Kusano E, Takahashi H, Ando Y, Yano K, Tsuda E, Asano Y. Vitamin K2 inhibits glucocorticoid-induced bone loss partly by preventing the reduction of osteoprotegerin (OPG). J Bone Miner Metab. 2005;23(1):41-7.
The study demonstrated that the inhibition exerted by vitamin K2 of the reduction in osteoprotegerin induced by GC may play a role in the prevention and treatment of glucocorticoid-induced bone loss.
Schurgers LJ, Teunissen KJ, Knapen MH, Kwaijtaal M, van Diest R, et al. (2005) Novel conformation-specific antibodies against gamma-carboxyglutamic acid (gla) protein: Undercarboxylated matrix gla protein as marker for vascular calcification. Arterioscler Thromb Vasc Biol 25: 1629–1633.
Shanahan C Vascular calcification. Curr Opn Nephrol Hypertens. 2005;14(4):361-7.
Accumulating evidence suggests that the high cardiovascular mortality observed in patients with end-stage renal disease is due in part to the effects of vascular calcification that develops over time on dialysis. Clinical studies demonstrate that high circulating levels of phosphate or calcium predict vascular calcification. Recent cell biological studies have provided novel insights into how vascular smooth muscle cells regulate calcification in response to such insults. Vascular smooth muscle cell damage and create an environment permissive for the nucleation of basic calcium phosphate mineral. This, combined with osteogenic conversion of vascular smooth muscle cells and consequent loss of their normal inhibitory processes/pathways, results in calcification.
Slinin Y, Foley RN, Collins AJ. Calcium, phosphorus, parathyroid hormone, and cardiovascular disease in hemodialysis patients: The USRDS waves 1, 3 and 4 study. J Am Soc Nephrol. 2005.;16(6):1788-93.
Teng M, Wolf M, Ofsthun MN, et a. Activated injectable vitamin D and hemodialysis survival: a historical cohort study. J Am Soc Nephrol. 2005;16:1115-25.
Tonelli M, Sacks F, Pfeffer M, Gao Z, Curhan G, et al. Relation between serum phosphate level and cardiovascular event rate in people with coronary disease. Circulation. 2005;112:2627–2633.
Vliegenthart R, Oudkerk M, Hofman A, Oei HH, van Dijck W, van Rooij FJ, et al. Coronary calcification improves cardiovascular risk prediction in the elderly. Circu. 2005;112(4):572-7.
Wang MC, Tsai WC, Chen JY, Huang JJ. Stepwise increase in arterial stiffness corresponding with the stage of chronic kidney disease. Am J Kidney Dis. 2005;45:494-501.
Young EW, Albert JM, Satayathum S, Goodkin DA, Pisoni RL, Akiba T, et al. Predictors and consequences of altered mineral metabolism: The Dialysis Outcomes and Practice Patterns Study. Kidney Int. 2005;67:1179-87.
Branley P. Use of phosphate binders in chronic kidney disease. The CARI Guidelines. Nephrology. 2006;11(Suppl 1):S245-S262.
Chen NX, Duan D, O’Neill KD, Wolisi GO, Koczman JJ, Lacair R, Moe SM. The mechanisms of uremic serum-induced expression of bone matrix proteins in bovine vascular smooth muscle cells. Kidney Int. 2006:70:1046-53.
Das M, Aronow WS, McClung JA, et al., Increased prevalence of coronary artery disease, silent myocardial ischemia, complex ventricular arrhythmias, atrial fibrillation left ventricular hypertrophy, mitral annular calcium, and aortic valve calcium in patients with chronic renal insufficiency. Cardiol Rev. 2006;14:14-17.
Hsu CY, Go AS, McCulloch CE, Darbinian J, Iribarren C. Exploring secular trends in the likelihood of receiving treatment for end-stage renal disease. Clin J Am Soc Nephrol. 2006;2(1):81-8.
Jadoul M, Albert JM, Akiba T, et al., Incidence and risk factors for hip or other bone fractures among hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study. Kidney Int. 2006;70:1358-66.
Ketteler M, Giachelli C. Novel insights into vascular calcification. Kidney Int Suppl. 2006 Dec;(105):S5-9.
Vascular calcification is not just a hallmark of uremic arterio- and atherosclerosis, but also is a significant cardiovascular risk factor in patients with chronic kidney disease. In contrast to the previous assumption that vascular calcification predominantly occurs by passive precipitation of calcium and phosphate ions, recent research led to the insight that extraosseous calcification is a highly regulated process. High serum phosphate and calcium levels may induce a process of osteogenic 'bone-like' differentiation of vascular smooth muscle cells, while deficiencies of calcification inhibitors or a disturbed balance towards calcification inducers may have a relevant pathophysiological influence on the initiation and progression of calcified lesions. This overview summarizes some of the best explored novel risk factors for disturbances of calcium and phosphate homeostasis and points to hyperphosphatemia as a modifiable key trigger in calcification processes.
Ketteler M, Schlieper G, Floege J. CalcifiÂÂÂÂcation and cardiovascular health: New insights into an old phenomenon. Hypertension 2006;47:1027–1034.
Kimoto E, Shoji T, Shinohara K, Hatsuda S, Mori K, Fukumoto S, Koyama H, Emoto M, Okuno Y, Nishizawa Y. Regional arterial stiffness in patients with type 2 diabetes and chronic kidney disease. J Am Soc Nephrol. 2006;17:2245-52.
Libby, P. Inflammation and cardiovascular disease mechanisms. Am J Clin Nutr. 2006;83(2):456S-460S.
Mathew S, Davies M, Lund R, Saab G, Hruska KA. Function and Mathew S, Davies M, Lund R, Saab G, Hruska KA. Function and effect of bone morphogenetic protein-7 in kidney bone and the bone-vascular links in chronic kidney disease. Eur J Clin Invest. 2006;36(Suppl 2):43–50.
Mazzini MJ, Schulze PC. Proatherogenic pathways leading to vascular calcification. Eur J Radiol. 2006;57(3):384-9.
Miller LM, Hopman WM, Garland JS, Yeates KE, Pilke RM. Cardioprotective medication use in hemodialysis patients. Can J Cardiol. 2006;22(9):755-60.
Moe S. Vascular calcification: Hardening of the evidence. Kidney Int. 2006;70(9):1535-1536.
Moe OW. Kidney stones: pathophysiology and medical management. Lancet. 2006;367:333-344.
National Kidney Foundation KDOQI. Clinical Practrice Guidelines. update 2006.
Saller F, Burnier L, Schapira M, Angelillo-Scherrer A. Role of growth arrest-specific gene 6 (gas6) product in thrombus stabilization. Blood Cells Mol Dis. 2006;36:373-378.
Savica V, Calo LA, Monardo P, Santoro D, Bellinghieri G. Phosphate binders and management of hyperphosphataemia in end-stage renal disease. Nephrol. Dial. Transplant. 2006 August;21(8):2065-68.
Sigrist M, Bungay P, Taal MW, McIntyre CW. Vascular calcification and cardiovascular function in chronic kidney disease. Nephrol Dial Transplant. 2006;21:707-14.
Son BK, Kozaki K, Iijima K, Eto M, Kojima T, Ota H, Senda Y, et al. Statins protect human aortic muscle cells from inorganic phosphate-induced calcification by restoring Gas6-Axl survival pathway. Circ Res. 2006:98(8):1024-31.
Sosnov J, Lessard D, Goldberg RJ, Yarzebski J, Gore JM. Differential symptoms of acute myocardial infarction in patients with kidney disease: A community-wide perspective. Am J Kidney Dis. 2006;47(3):378-84.
Thijssen HH, Vervoort LM, Schurgers, LJ, Shearer MJ. Menadione is a metabolite of oral vitamin K. Br J Nutr. 2006;95(2):2560-6.
Phylloquinone is converted into menaquinone-4 and accumulates in extrahepatic tissues. Neither the route nor the function of the conversion is known. One possible metabolic route might be the release of menadione from phylloquinone by catabolic activity.
Yao Y, Zebboudj AF, Shao E, Perez M, Bostrom K. Regulation of bone morphogenetic protein-4 by matrix GLA protein in vascular endothelial cells involves activin-like kinase receptor 1. J Biol Chem. 2006;281(45):33923-30.
Bolton-Smith C, McMurdo ME, Paterson CR, Mole PA, Harvey JM, Fenton ST, et al. Two-year randomized controlled trial of vitamin K1 (phylloquinone) and vitamin D3 plus calcium on the bone health of older women. J Bone Miner Res. 2007;22(4):590-19.
Dietary supplementation with vitamin K1, with vitamin D3 and calcium, or their combination was examined in healthy older women during a two year trial. Women who took combined vitamin K and vitamin D plus calcium showed a significant and sustained improvement in bone health. As well, serum vitamin K1 increased by 157%, the percentage of undercarboxylated osteocalcin decreased by 51%, serum vitamin D increased by 17% and PTH decreased by 11%.
Boonen S, Lips P, Bouillon R, Bischoff-Ferrari HA, Vanderschuren D, Haentjens P. Need for additional calcium to reduce the risk of hip fracture with vitamin d supplementation: Evidence from a comparative metaanalysis of randomized controlled trials. J Clin Endocrinol Metab. 2007;92(4):1415-23.
Bellosta S, Baetta R, Canavesi M, Comparato C, Granata A, Monetti M, et al. Reloxifene inhibits matrix metalloproteinases expression and activity in macrophages and smooth muscle cells. Pharmacol Res. 2007;56(2):160-7.
Bleuming SA, He XC, Kodach LL, Hardwick, JC, Koopman FA, Ten Kate FJ, et al. Bone morphogenetic protein signaling suppresses turmoigenesis at gastric epithelial transition zones in mice. Cancer Res. 2007;67(17):8149-55.
Block GA, Raggi P, Bellasi A, Kooienga L, Spiegel DM. Mortality effect of coronary calcification and phosphate binder choice in incident hemodialysis patients. Kidney Int 2007;71:438–441.
Coresh J, Selvin E, Stevvens LA et al., Prevalence of chronic kidney disease in the United States. JAMA. 2007 Nov;293(17):2038-47.
Craver L, Marco MP, Martinez I, Rue M, Borras M, Martin ML et al. Mineral metabolism parameters throughout chronic kidney disease stages 1-5 achievement of K/DOQI target ranges. Nephrol.Dial Transpl. 2007;22:1171-1176.
de Boer IH, Ioannou GN, Kestenbaum B, Brunzell JD, Weiss NS. 25-hydroxyvitamin D levels and albuminuria in the Third National Health and Nutrition Examination Survey (NHANES III). Am J Kidney Dis. 2007;50:69-77.
Ensrud KE, Lui LY, Taylor BC, et al. Osteoporotic Fractures Research Group. Renal function and risk of hip and vertebral fractures in older women. Arch Intern Med. 2007 Jan 22;167(2):133-9.
The SOF study of 9000+ postmenopausal women found that in women with no intrinsic renal disease, age-related decline in kidney function was responsible for a near doubling of fracture risk in women with eGFR of less than 65 ml/min/1.73 m2 as compared to age-matched women with normal GFR.
Felsenfeld AJ, Rodriguez M, Aguilera-Tejero E. Dynamics of parathyroid hormone secretion in health and secondary hyperparathyroidism. Clin J Am Soc Nephrol. 2007;2(6):1283-305.
Gao B, Yasui T, Itoh Y, Tozawa K, Hayashi Y, Kohri K. A polymorphism of matrix Gla protein gene is associated with kidney stones. J Urol. 2007;177:2361–2365.
Matrix Gla protein (MGP) is a molecular determinant regulating the extracellular matrix calcification. This study investigated the association of genetic polymorphisms of MGP with kidney stone in the Chinese Han population. An SNP was found to be associated with kidney stone in the Chinese Han population. The association was confirmed in the Chinese and Japanese populations. This finding highlighted the importance of vitamin K dependent proteins in kidney function.
Gal-Moscovici A, Sprague, SM. Bone health in chronic kidney disease-mineral and bone disease. Adv Chronic Kidney Dis. 2007;14(1):27-36.
Gross ML, Meyer HP, Ziebart H et al. CalcifiÂÂÂÂcation of coronary intima and media: Immunohistochemistry, backscatter imaging, and x-ray analysis in renal and nonrenal patients. Clin J Am Soc Nephrol. 2007;2:121–134.
Hermans MM, Vermeer C, Kooman JP, Brandenburg V, Ketteler M, Gladziwa U, Rensma PL, Leunissen KM, Schurgers LJ. Undercarboxylated matrix GLA protein levels are decreased in dialysis patients and related to parameters of calcium-phosphate metabolism and aortic augmentation index. Blood Purif. 2007;25:395–401.
Vascular calcifications are related to cardiovascular mortality and morbidity in dialysis patients. Limited data exist on the role of calcification inhibitors, such as matrix-carboxyglutamic acid protein (MGP) in dialysis patients. This study found significantly lower serum ucMGP levels in dialysis patients compared to healthy controls. ucMGP levels were inversely associated with phosphate and positively associated with serum fetuin-A levels. Furthermore ucMGP levels were inversely associated with the aortic augmentation index.
Holden RM, Sanfilippo AS, Hopman WM, Zimmerman D, Garland JS, Morton AR. Warfarin and aortic valve calcification in hemodialysis patients. J Nephrol. 2007;20:417-22.
Ix et al., 2007. Levin A, Bakris GL, Molitch M, et al. Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: results of the study to evaluate early kidney disease. Kidney Int. 2007;71:31-38.
Levey AS, Atkins R, Coresh J, et al. Chronic kidney disease as a global public health problem: Approaches and initiatives—a position statement from Kidney Disease Improving Global Outcomes. Kidney Int. 2007;72(3):247–259.
Levin A, Bakris GL, Molitch M, et. al. Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: results of the study to evaluate early kidney disease. Kidney Int. 2007 Jan;71(1):31-8.
Maree AO, Jneid H, Palacios IF, Rosenfield K, MacRae CA, et al. Growth arrest specific gene (GAS) 6 modulates platelet thrombus formation and vascular wall homeostasis and represents an attractive drug target. Curr Pharm Dex. 2007;13(26):2656-2661.
Okuno S, Ishimura E, Kitatani K, Fujino Y, Kohno K, Maeno Y. Presence of abdominal aortic calcification is significantly associated with all-cause and cardiovascular mortality in maintenance hemodialysis patients. Am J Kidney Dis. 2007;49:417-425.
Pilkey RM, Morton AR, Boffa MB, Noordhof C, Day AG, Su Y, Miller LM, Koschinsky ML, Booth SL. Subclinical vitamin K deficiency in hemodialysis patients. Am J Kidney Dis. 2007;49:432–439.
Subclinical vitamin K deficiency increasingly is associated with extraosseous calcification in healthy adults. Nondietary determinants of vitamin K status include apolipoprotein E (apoE) genotype, which may influence vitamin K transport to peripheral tissues. Serum phylloquinone concentrations, percentage of unOC were measured, and ApoE phenotype was determined. The data indicated suboptimal vitamin K status in dialysis patients. The apoE4 gene allele influences osteocalcin gamma-carboxylation in dialysis patients.
Russo D, Corrao S, Miranda I, et al. Progression of coronary artery calcification in predialysis patients. Am J Nephrol 2007;27:152-158.
Schrier RW. Cardiorenal versus renocardiac syndrome: is there a difference? Nat Clin Pract Nephrol. 2007;3(12):637.
Schlieper G, Westenfeld R, Brandenburg V, Ketteler M. Inhibitors of calcification in blood and urine. Semin Dial. 2007;20:113–121.
In bone and teeth formation, coordinated calcification is a highly desirable biological process. However, heterotopic calcification at unwanted tissue sites leads to dysfunction, disease and, potentially, to death and therefore requires prevention and treatment. With the recent discovery of calcification inhibitors we now know that biological calcification is not passive but a complex, active and highly regulated process. Atherosclerosis is often accompanied by intimal plaque calcification, whereas arteriosclerosis is characterized by calcification of the media. Patients with chronic kidney disease are at especially increased risk for both intimal and medial calcification. In this context, it is currently thought that calcium-regulatory factors including fetuin-A, matrix Gla protein, osteoprotegerin, and pyrophosphates act in a local or systemic manner to prevent calcifications of the vasculature, and that dys-regulations of such calcification inhibitors may contribute to progressive calcifications.
Schiffrin E, Lipman M, Mann J. Chronic kidney disease: Effects on the cardiovascular system. Circulation. 2007;116(1):85-97.
Schurgers LJ, Spronk HM, Skepper JN, Hackeng TM, Shanahan CM, Vermeer C, et al. Post-translational modifications regulate matrix Gla protein function: Importance for inhibition of vascular smooth muscle cell calcification. J Thomb Haemost. 2007;5(12):2503-11.
Matrix Gla protein (MGP) is a small vitamin K-dependent protein containing five gamma-carboxyglutamic acid (Gla) residues that are believed to be important in binding Ca(2+), calcium crystals and bone morphogenetic protein. MGP has been shown to be a potent inhibitor of vascular calcification; however, the precise molecular mechanism underlying the function of MGP is not yet fully understood. We investigated the effects of MGP in human vascular smooth muscle cell (VSMC) monolayers that undergo calcification after exposure to an increase in Ca(2+) concentration. Increased calcium salt deposition was found in cells treated with the vitamin K antagonist warfarin as compared to controls, whereas cells treated with vitamin K(1) showed decreased calcification as compared to controls. These data demonstrate that both gamma-glutamyl carboxylation and serine phosphorylation of MGP contribute to its function as a calcification inhibitor and that MGP may inhibit calcification via binding to VSMC-derived vesicles.
Schroff RC, Shanahan CM. Vascular calcification in patients with kidney disease: The vascular biology of calcification. Seminars in Dialysis. 2007;20(2):103-109.
Vascular calcification is an active, cell-mediated process that results from an imbalance between the promoters and inhibitors of mineralization. The process of vascular calcification shares many similarities with that of skeletal mineralization. However, while skeletal mineralization is a regulated process induced by complex, well-timed developmental cues, vascular calcification is a pathological process, occurring in response to dysregulated/inappropriate environmental cues. Damage inducing agents present in the uremic milieu such as a mineral imbalance, induce vascular smooth muscle cell (VSMC) apoptosis, and vesicle release resulting in mineral nucleation and the deposition of hydroxyapatite. Under normal conditions, inhibitors of soft-tissue mineralization such as matrix γ-carboxyglutamic acid protein are expressed locally within the vessel wall while others such as fetuin-A are present in the circulation. Down-regulation or perturbation of these proteins leads to a phenotypic transformation of VSMC into osteo/chondrocytic-like cells that have the capacity to modulate the mineralization process. Many aspects of the mechanisms underlying vascular calcification have been defined through in vitro studies and molecular biological techniques; however, there are still unanswered questions, particularly with respect to the relationship between bone and vascular calcification, processes that appear to be inversely related. A better understanding of the complex mechanisms regulating tissue calcification may have therapeutic potential in reducing the cardiovascular disease-associated morbidity and mortality in patients with renal disease.
Shea MK, Booth SL. Role of vitamin K in the regulation of calcification. International Congress Series: Nutritional Aspects of Osteoporosis. 2007;1297:165-178.
Observational studies are promising in terms of associations between vitamin K and bone health. The level of evidence from randomized, double-blind, placebo-controlled trials with phylloquinone is very limited. In contrast, there is strong evidence of a protective effect of menaquinone-4 in pharmacological doses on age-related bone loss and fracture risk. This effect appears to be enhanced by vitamin D supplementation, and is supportive of the premise that all studies should be considered in the context of beneficial effects of vitamin K above and beyond that attained by calcium and vitamin D supplementation alone.
Sigrist MK, Taal MW, Bungay P, et al. Progressive vascular calcification over 2 years is associated with arterial stiffening and increased mortality in patients with stages 4 and 5 chronic kidney disease. Clin J Am Soc Nephrol. 2007;2:1241-1248.
Suki WN, Zabaneh R, Cangiano JL, Reed J, Fischer D, Garrett L,et al. Effects of sevelamer and calcium-based phosphate binders on mortality in hemodialysis patients. Kidney Int. 2007;72(9):1130-7.
US Renal Data System, RSRDS 2007. Annual Data Report: Atlas of End-Stage Renal Disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD. 2007.
Zoungas S, Cameron JD, Kerr PG, Wolfe R, Muske C, McNeil JJ. Association of carotid intima-medial thickness and indices of arterial stiffness with cardiovascular disease outcomes in CKD. Am J Kidney Dis. 2007;50(4):622-30.
Westenfeld R, Jahnen-Dechent W, Ketteler, M. Vascular calcification and fetuin-A deficiency in chronic kidney disease. Trends Cardiovasc Med. 2007;17(4):124-128.
Yamada K, Fujimoto S, Nishiura R, Komatsu H, Tatsumoto M, Sato Y, et al. Risk factors of the progression of abdominal aortic calcification in patients on chronic haemodialysis. Nephrol Dial Transplant. 2007;22(7):2032-7.
Zehnder D, Landray MJ, Wheeler DC, et al. Cross-sectional analysis of abnormalities of mineral homeostasis, vitamin D and parathyroid hormone in a cohort of pre-dialysis patients. The chronic renal impairment in Birmingham (CRIB) study. Nephron Clin Pract. 2007;107:c109-116.
Zitterman A, Schleithoff SS, Koerfer R. Letter by Zitterman et al regarding article, “Calcium/vitamin D supplementation and cardiovascular events”. Circulation. 2007;116(3):3i5, author reply e87.
Amann K. Media calcification and intima calcification are distinct entities in chronic kidney disease. Clin J Am Soc Nephrol. 2008;3:1599-1605.
Barreto DV, Barreto Fde C, de Carvalho AB, et al. Phosphate binder impact on bone remodeling and coronary calcification—results from the BRiC study. Nephron Clin Pract. 2008;110:c273-c283.
Bolland MJ, Barber PA, Doughty RN, Mason B, Home A, Ames R, et al. Vascular events in healthy older women receiving calcium supplementation: randomized controlled trial. BMJ. 2008;336(7638):262-6.
Cauley JA, LaCroix AZ, Wu L, Horwitz M, Danielson ME, Bauer DC, et al. Serum 25-hydroxyvitamin D concentrations and risk for hip fractures. Ann Intern Med. 2008 Aug;149(4):242-5024.
Chonchol M, Whittle J, Desbien A, Orner MB, Petersen LA, Kressin NR. Chronic kidney disease is associated with angiographic coronary artery disease. Am J Nephrol. 2008; 28(2):354-60.
We evaluated the relationship between CKD and severe coronary artery disease (CAD) in 261 male veterans with imaging tests suggesting coronary ischemia. Patients with CKD were more likely than those without CKD to have at least one significant coronary obstruction (75.9 vs. 60.7%, p = 0.016). Patients with CKD also had more significant CAD, that is, were more likely to have three-vessel and/or left main disease than those without CKD (34.9 vs. 16.9%, p = 0.0035). In logistic regression analysis, controlling for demographics and comorbidity, CKD continued to be independently associated with the presence of significant CAD. We concluded that CKD patients have a high prevalence of obstructive coronary disease, which may contribute to their high cardiovascular mortality.
Danziger J. Vitamin K-dependent proteins, warfarin, and vascular calcification. Clin J Am Soc Nephrol. 2008;3(5):1504–1510.
This article reviews the general physiology of VKDPs and explores a potential relationship between warfarin and vascular calcification in susceptible individuals. Vitamin K-dependent proteins (VKDPs) require carboxylation to become biologically active. Matrix Gla Protein (MGP) and Growth Arrest Specific Gene 6 (Gas-6) are two particularly important VKDPs. MGP prevents vascular calcification and Gas-6 affects vascular smooth muscle cell apoptosis and movement. Unlike the coagulant factors, which undergo hepatic carboxylation, MGP and Gas-6 are carboxylated within the vasculature, at the blood vessel level. This peripheral carboxylation process is distinct from hepatic carboxylation, yet both are inhibited by warfarin administration. Warfarin prevents the activation of MGP and Gas-6, and in animals, induces vascular calcification. Given the high risk of vascular calcification in those patients with chronic kidney disease, the importance of understanding warfarin's effect on VKDPs is paramount.
D'Andrea G, D'Ambrosio R, Margaglione M. Oral anticoagulants: Pharmacogenetics relationship between genetic and non-genetic factors. Blood Rev. 2008;22:127–140.
Dobnig H, Pilz S, Scharnagl H, et al. Independent association of low serum 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D levels with all-cause and cardiovascular mortality. Arch Intern Med. 2008; 168:1340-9.
Fernandez-Fernandez L, Bellido-Martin L, Garcia de Frutos P. Growth arrest-specific gene 6 (GAS6). An outline of its role in haemostasis and inflammation. Thromb Haemost. 2008;100(4):604-10.
Garland JS, Holden RM, Groome PA, et al: Prevalence and associations of coronary artery calcification in patients with stages 3 to 5 CKD without cardiovascular disease. Am J Kidney Dis. 2008; 52: 849–858.
Giovannucci E, Liu Y, Hollis BW, Rimm EB. 25-hydroxyvitamin D and risk of myocardial infarction in men: A prospective study. Arch Intern Med. 2008;168:1174-80.
Heinrich T, Heidt H, Hafner V, Schmidt-Gayk H, Jenetzky E, Walter-Sack I, et al., Calcium load during administration of calcium carbonate or sevelamer in individuals with normal renal function. Nephrol dial Transplant. 2008;23(9):2861-7.
Holden RM, Iliescu E, Morton AR et al. Vitamin K status of Canadian peritoneal dialysis patients. Perit Dial Int. 2008; 28: 415–418.
Their study indicated that a significant proportion of peritoneal-dialysis patients have subclinical vitamin K deficiency.
Holick MF. The vitamin D deficiency pandemic and consequences for nonskeletal health: Mechanisms of action. Mol Aspects Med. 2008 Dec;29(6):361-8.
Hsu JJ, Tintut Y, Demer LL. Vitamin D and osteogenic differentiation in the artery wall. Clin J Am Soc Nephrol. 2008;3(5):1542-7.
LaCroix AZ, Lee JS, Wu L, Cauley JA, Shlipak MG, Ott SM, et al. Cystatin-C renal function and incidence of hip fracture in postmenopausal women. J Am Geriatr Soc. 2008;56(8):1434-41.
London GM, Marchais SJ, Guerin AP, Boutouyrie P, Metivier F, de Vernejoul MC. Association of bone activity, calcium load, aortic stiffness, and calcifications in ESRD. J Am Soc Nephrol. 2008;19(9):1827-35.
McCullough PA, Agrawal V, Danielewicz E, Abela GS. Accelerated atherosclerotic calcification and Monckeberg’s sclerosis: A continuum of advanced vascular pathology in chronic kidney disease. Clin J Am Soc Nephrol. 2008;3:1585-1598.
Moe SM, Chen NX. Mechanisms of vascular calcification in chronic kidney disease. J Am Soc Nephrol. 2008;19(2):213-6.
Musial K, Formalczyk K, Zwoliriska D. Osteopontin (OPN), PDGF-BB (platelet-derived growth factor), and BMP-7 (bone morphogenetic protein) as markers of atherogenesis in children with chronic kidney disease (CKD) treated conservatively-preliminary results. 2008;24 Suppl 4:25-7.
Okano T, Shimomura Y, Yamane M, Suhara Y, Karnao M, Sugiura M, et al.,Conversion of phylloquinone (Vitamin K1) into menaquinone-4 (Vitamin K2) in mice: Two possible routs for menaquinone-4 accumulation in cerebra of mice. J Biol Chem. 2008;283(175):11270-9.
Phylloquinone (vitamin K(1)) is a major type of dietary vitamin K, but its concentrations in animal tissues are remarkably low compared with those of the menaquinones, especially menaquinone-4 (vitamin K(2)), the major form of vitamin K in tissues. Despite this great difference, the origin of tissue menaquinone-4 has yet to be exclusively defined. It is postulated that phylloquinone is converted into menaquinone-4 and accumulates in extrahepatic tissues. To clarify this, phylloquinone with a deuterium-labeled 2-methyl-1,4-naphthoquinone ring was given orally to mice, and cerebra were collected for analyses. Our results suggest that cerebral menaquinone-4 originates from phylloquinone intake and that there are two routes of accumulation, one is the release of menadione from phylloquinone in the intestine followed by the prenylation of menadione into menaquinone-4 in tissues, and another is cleavage and prenylation within the cerebrum.
Pilz S, Dobnig H, Fischer JE, et al. Low vitamin D levels predict stroke in patients referred to coronary angiography. Stroke. 2008;39:2611-3.
Quinibi W, Moustafa M, Muenz LR, et al. CARE-2 Investigators. A 1-year randomized trial of calcium acetate versus sevelamer on progression of coronary artery calcification in hemodialysis patients with comparable lipid control: the Calcium Acetate Renagel Evaluation-2 (CARE-2) study. Am J Kidney Dis. 2008;51:952-965.
Schlieper G, Kruger T, Djuric Z, Damjanovic T, Markovic N, Schurgers LJ, et al. Vascular access calcification predicts mortality in hemodialysis patients. Kidney Int. 2008;74:1582–1587.
Schroff RC, McNair R, Figg N, Skepper JN, Schurgers L, Ashmeet G, et al. Dialysis accelerates medial vascular calcification in part by triggering smooth muscle cell apoptosis. Circulation. 2008;118:1748-1757.
While vascular calcification is associated with increased morbidity and mortality in chronic kidney disease, the early mechanisms are poorly understood. In this study, they measured the calcium load in arteries of children with chronic kidney disease, before and after dialysis, and correlated it with clinical, biochemical and vascular measures. They found that the calcium load was present before dialysis began, and that once dialysis was initiated, then vascular smooth muscle cell apoptosis, VSMC, (or cell death) began, and the children presented with increased carotid thickening and aortic stiffness. They concluded that the dialysis was a factor in disabling the VSMC defense mechanisms, leading to overt calcification.
Schurgers LJ, Cranenburg EC, Vermeer C. Matrix Gla-protein: The calcification inhibitor in need of vitamin K. Thromb Haemost. 2008;100:593-603.
Suliman Me, Garcia-Lopez E, Anderstam B, Lindholm B, Stenvinkel P. Vascular calcification inhibitors in relation to cardiovascular disease with special emphasis on fetuin-A in chronic kidney disease. Adv Clin Chem. 2008;46:217-62.
Surman-Schmitt C, Dietz U, Kireva T, Adam N, Park J, Tarariello A. Ucma, a novel secreted cartilage-specific protein with implications in osteogenesis. J of Biol Chem. 2008;283:7082-93.
Tomasello S. Secondary hyperparathyroidism and chronic kidney disease. Diabetes Spectrum. 2008;21(1):19-25.
Verdalles Guzmán Ú., De La Cueva P., Verde E., De Vinuesa S.G., Goicoechea M., Mosse A., López Gómez J.M., Luño J. Calciphylaxis: Fatal complication of cardiometabolic syndrome in patients with end stage kidney disease. Nefrologia. 2008;28:32–36.
In a retrospective clinical study including patients on haemodialysis who developed calciphylaxis, 6/8 patients were on VKAs therapy. This suggests VKAs therapy as one of the factors involved in the development of calciphylaxis, which is a rare but fatal complication in CKD patients, characterized by ischemic skin ulceration due to mineralization affecting subcutaneous small arterioles.
Wang TJ, Pencina MJ, Booth SL, et al. Vitamin D deficiency and risk of cardiovascular disease. Circulation. 2008;117:503-11.
Wallin R, Schurgers LJ, Wajih N. Effects of the blood coagulation vitamin K as an inhibitor of arterial calcification. 2008;122(3):411-7.
The findings suggest that MK4 acts as an anti-calcification component in the vessel wall.
Barreto DV, Barreto FC, Liabeuf S, Temmar M, Boitte F, Choukroun G, et al. Vitamin D affects survival independently of vascular calcification in chronic kidney disease. Clin J Am Soc Nephrol. 2009;4(6):1128-35.
Beulens JW, Bots ML, Atsma F, Bartelink ML, Prokop M, et al. High dietary menaquinone intake is associated with reduced coronary calcification. Atherosclerosis. 2009;203:489–493.
The study showed that high dietary menaquinone intake, but probably not phylloquinone, is associated with reduced coronary calcification. Adequate menaquinone intakes could therefore be important to prevent cardiovascular disease.
Brandenburg VM, Jahnen-Dechent W, Ketteler M. Sevelamer and the bone-vascular axis in chronic kidney disease: Bone turnover, inflammation, and calcification regulation. Kidney Int Suppl. 2009;(114):S26-33.
Chan KE, Lazarus JM, Thadhani R, Hakim RM. Warfarin use associated with increased risk for stroke in hemodialysis patients with atrial fibrillation. J Am Soc Nephrol. 2009;20:2223–2233.
Cranenburg EC, Brandenburg VM, Vermeer C, Stenger M, Muhlenbruch G, Mahnken AH, et al. Uncarboxylated matrix Gla protein (ucMGP) is associated with coronary artery calcification in haemodialysis patients. Thromb Haemost. 2009;101:359–366.
Foley RN, Collins AJ, Herzog CA, Ishani A, Kalra PA.. Serum phosphorus levels associate with coronary atherosclerosis in young adults. J Am Soc Nephrol. 2009;20(2):397.
Hutchison AJ, Barnett ME, Krause R, Siami GA, Lanthanum Carbonate Study Group. Lanthanum carbonate treatment, for up to 6 years, is not associated with adverse effects on the liver in patients with chronic kidney disease Stage 5 receiving hemodialysis. Clin Nephrol. 2009;71(3):286-95.
KDIGO® Clinical Practice Guideline for 92 Supplemental Tables Chronic Kidney Disease-Mineral & Bone Disorder. June 2009.
Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group. KDIGO Clinical Practice Guideline for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD).Kidney Int Suppl. 2009;113:S1-130).
Kruger T, Floege J. Coumarin use in dialysis patients with atrial fibrillation: More harm than benefit? Nephrol Dial Transplant. 2009;24:3284–3285.
Krueger T, Westenfeld R, Ketteler M, Schurgers LJ, Floege J. Vitamin K deficiency in CKD patients: A modifiable risk factor for vascular calcification? Kidney Int. 2009;76:18-22.
The purpose of this review is to summarize currently available evidence implicating vitamin K in the pathogenesis of vascular calcification (VC), in particular arterial medial calcification. In doing so, we try to provide a rationale for an interventional clinical study testing whether vitamin K supplementation can retard VC or even affect cardiovascular mortality in chronic kidney disease patients. Additionally, we give an overview of the literature indicatging the adverse effects of long-term vitamin K antagonists in this population.
Krueger T, Westenfeld R, Schurgers L, Brandenburg V. Coagulation meets calcification: The vitamin K system. Int J Artif Organs. 2009a;32:67-74.
Bone disease and vascular disease are two typical entites in CKD contributing to excess morbidity and mortality. Vitamin K and vitamin K-dependent-proteins are osteocalcin (regulating bone mineralization) and matrix-Gla protein (MGP, local calcification inhibitor in the vessel wall). Vitamin K deficiency impairs the physiological function of osteocalcin and MGP, and presumably contributes to bone demineralization and vascular calcification (the so-called calcification paradox). In this context, the usage of vitamin K antagonists might be especially risky in CKD patients.
Lerner RG, Aronow WS, Sekhri A, et al. Warfarin use and the risk of valvular calcification. J Thromb Haemost. 2009;7:2023-27.
Warfarin affects the synthesis and function of the matrix Gla-protein, a vitamin K-dependent protein, which is a potent inhibitor of tissue calcification. Objectives: To investigate the incidence of mitral valve calcium (MVC), mitral annular calcium (MAC) and aortic valve calcium (AVC) in patients with non-valvular atrial fibrillation (AF) treated with warfarin vs. no warfarin. There was a significant association between the use of warfarin and the risk of calcification
Li M, Batuman V. Vitamin D: A new hope for chronic kidney disease? Kidney Int. 2009;76(12):1219-21.
Mizobuchi M, Towler D, Slatopolsky E. Vascular calcification: the killer of patients with chronic kidney disease. J Am Soc Nephrol. 2009;20:1453-1464.
Parker BD, Ix JH, Cranenburg EC, Vermeer C, Whooley MA, Schurgers LJ, et al. Association of kidney function and uncarboxylated matrix Gla protein: data from the Heart and Soul Study. Nephrol Dial Transplant. 2009;24;2095-2101.
Vitamin K can be measured by desphospho-uncarboxylated-MGP levels, a high level of MGP reflects a decreased level of vitamin K that seems to be related to both kidney damage and cardiovascular risks in patients with CKD. The carboxylation status of MGP may be improved by vitamin K2 supplementation.
Mehrota R, Kermah DA, Salusky IB, Wolf MS, Thadhani RI, Xhiu YQ, et al. Chronic kidney disease, hypovitaminosis D, and mortality in the United States. Kidney Intern. 2009;76:977-983.
Moe SM, Chen NX, Seifert MF, Sinders RM, Duan D, Chen X, et al. A rat model of chronic kidney disease-mineral bone disorder. Kidney Int. 2009;75(2):176084.
Nerlander M, Voong K, Manghat P, Hampson G, Harrington D, Shearer M, Goldsmith D. Subclinical deficiency of vitamin K status in chronic kidney disease. World Congress of Nephrology (Poster session), Milan. 2009; May 22–26.
Vitamin K is an essential cofactor for the enzyme gamma glutamyl carboxylase, which is pivotal to the formation of Gla residues on a small family of proteins, which can then bind calcium. Matrix Gla Protein is one of these proteins and is an important tissue-bound inhibitor of vascular calcification, which is greatly incrased in CKD. In this study they verified the vitamin K status in patients with CKD. The results indicated that low-level vitamin K functional abnormalities can be detected in healthy ambulant CKD stage 1-5 patients.
Ravani P, Malberti F, Tripepi G, et al. Vitamin D levels and patient outcome in chronic kidney disease. Kidney Int. 2009:75(1):88-95.
Rodriguez-Garcia M, Gomex-Alonso C, Naves-Diaz M, Diaz-Lopez JB, Diaz-Corte C, Cannata-Andia JB, Asturias Study Group. Vascular calcifications, vertebral fractures and mortality in haemodialysis patients. Nephrol Dial Transplant. 2009;24:239-46.
Schlieper G, Brandenburg V, Djuric Z, Damjanovic T, Markovic N, Schurgers L, et al. Risk factors for cardiovascular calcifications in non-diabetic Caucasian haemodialysis patients. Kidney Blood Press Res. 2009;32:161–168.
In our cohort of non-diabetic Caucasian haemodialysis patients, age, male gender, dialysis vintage, smoking, calcium-phosphate product, high-sensitivity CRP and lower Kt/V were independent risk factors for cardiovascular calcifications. Whether lowering the calcium-phosphate product and increasing dialysis efficiency can reduce cardiovascular calcifications in dialysis patients remains to be determined.
Shea MK, O'Donnell CJ, Hoffman U, Dallal GE, Dawson-Hughes B, Ordovas JM, Price PA et al. Vitamin K supplementation and progression of coronary artery calcium in older men and women. Am J Clin Nutr. 2009;89:1799-1807.
Coronary artery calcification (CAC) reflects the calcium burden within the intima and media of the coronary arteries. In population-based studies, CAC independently predicts cardiovascular disease (CVD) and mortality. A preventive role for vitamin K in vascular calcification has been proposed based on its role in activating matrix Gla protein (MGP), a calcification inhibitor that is expressed in vascular tissue. Vascular calcification is highly prevalent in certain patient populations, especially in those with chronic kidney disease (CKD), and it is plausible that vitamin K may contribute to reducing vascular calcification in patients at higher risk. Subclinical vitamin K deficiency has been reported in CKD patients, but studies linking vitamin K status to calcification outcomes in CKD are needed to clarify whether or not improving vitamin K status is associated with improved vascular health in CKD. This review summarizes the available evidence of vitamin K and vascular calcification in population-based studies and clinic-based studies, with a specific focus on CKD patients. .
Speer MY, Yang HY, Brabb T, Leaf E, Look A, Lin WL, Frutkin A,et al. Smooth muscle cells give rise to osteochondrogenic precursors and chondrocytes in calcifying arteries. Circ Res. 2009;104(6):733-41.
Viegas. CS, Cavaco S, Neves PL, Ferreira A, Joao A, Williamson MK, et al. Gla-rich protein is a novel vitamin K-dependent protein present in serum that accumulates at sites of pathological calcifications. Am J Pathol. 2009;175(6):2288-98.
Yao Y, Watson AD, Ji S, Bostrom KI. Heat shock protein 70 enhances vascular bone morphogenetic protein-4 signaling by binding matrix Gla protein. Circ Res. 2009;105(6):575-84.
2010
Bagshaw SM, Cruz DN. Fluid overload as a biomarker of heart failure and acute kidney injury. Contrib Nephrol. 2010;164:54-58.
Cozzolino M, Missaglia E, Ortiz A, Bellasi A, Adragao T, Apostolous T. Vascular calcification in chronic kidney disease. Recenti Prog Med. 2010 Nov;101(11):442-52.
Cranenburg EC, Koos R, Schurgers LJ, Magdeleyns EJ, Schoonbrood TH, et al. Characterisation and potential diagnostic value of circulating matrix gla protein (MGP) species. Thromb Haemost. 2010;104:811–822.
Drechsler C, Pilz S, Obermayer-Pietsch B, Verduign M, Tomaschitz A, Krane V, Espe K, et al. Vitamin D deficiency is associated with sudden cardiac death, combined cardiovascular events, and mortality in haemodialysis patients. Eur Heart J. 2010 Sep;31(18):2253-61.
Drueke TB, Massy ZA. Atherosclerosis in CKD: Differences from the general population. Nat Rev Nephrol. 2010; 6(12)723-35.
Gao B, Yasui D, Lu X et al. Matrix Gla protein expression in NRK-52E cells exposed to oxalate and calcium oxalate monohydrate crystals. Urol Int. 2010; 85: 237–241.
Holden RM, Morton AR, Garland JS, et al. Vitamins K and D status in stages 3-5 chronic kidney disease. Clin J Am Society Nephrol. 2010;5:590–597.
Vitamin K and D status was measured as dietary intake, plasma phylloquinone, serum percent uncarboxylated osteocalcin (%ucOC), proteins induced by vitamin K absence (PIVKA-II), VKOR (vitamin K Epoxide Reductase), apolipoprotein E genotype (apoE), and plasma 25-hydroxyvitamin D in 172 subjects with stage 3 to 5 CKD. Subclinical vitamin K deficiency criteria was met by 6% (phylloquinone), 60% (%ucOC), and 97% (PIVKA-II) of subjects, whereas 58.3% and 8.6% had 25(OH)D insufficiency and deficiency, respectively. Dietary vitamin K intake was associated with higher phylloquinone and lower PIVKA-II. There were positive correlations between phylloquinone and the presence of stable weight, and the absence of subcutaneous fat loss or muscle wasting. 25(OH)D levels were positively associated with stable weight and albumin (P < 0.001). PIVKA-II levels were associated with apolipoprotein E genotype. Higher %ucOC and lower 25(OH)D were similarly associated with CKD stage, parameters of mineral metabolism, and urine albumin to creatinine ratio. They concluded that a suboptimal vitamin K and D status is prevalent in patients with CKD. Proteinuria was associated with both a suboptimal vitamin D status as well as worse peripheral vitamin K status.
Kalantar-zadeh K, Gutekunst L, Mehrota R, Kovesdy CP, Bross R, Shinaberger CS, et al. Understanding sources of dietary phosphorus in the treatment of patients with chronic kidney disease. Clin J Am Soc Nephrol. 2010;5(3):519-30.
London G, Coyne D, Hruska K, Malluche HH, Martin KJ. The new kidney disease: Improving global outcomes (KDIGO) guidelines - expert clinical focus on bone and vascular calcification. Clin Nephrol. 2010 Dec;74(6):423-32.
Chronic kidney disease-mineral and bone disorder (CKD-MBD) defines a triad of interrelated abnormalities of serum biochemistry, bone and the vasculature associated with chronic kidney disease (CKD). The new kidney disease: improving global outcomes (KDIGO) guidelines define the quality and depth of evidence supporting therapeutic intervention in CKD-BMD. They also highlight where patient management decisions lack a strong evidence base. The body of evidence linking poor bone health and reservoir function (the ability of bone to buffer calcium and phosphorus) with vascular calcification and cardiovascular outcomes is growing. Treating renal bone disease should be one of the primary aims of therapy for CKD. Evaluation of the biochemical parameters of CKD-BMD (primarily phosphorus, calcium, parathyroid hormone and vitamin D levels) as early as CKD Stage 3, and an assessment of bone status (by the best means available), should be used to guide treatment decisions. Early reduction of phosphorus load may ameliorate these adverse effects. Evidence that calcium laod may influence progressioin of vascular calcificaiton with effects on mortality should also be considered when choosing which phosphate binder to be used. The risks, benefits, and strength of evidence for various treatment options for the abnormalities of CKD-BMD are considered.
Nakano T, Ninomiya T, Sumiyoshi S, Fujii H, Doi Y, Hirakata H, et al. Association of kidney function with coronary atherosclerosis and calcification in autopsy samples from Japanese elders: The Hisayama study. Am J Kidney Dis. 2010 Jan;55(1):21-30.
O’Neill W, Lomashvili K. Recent progress in the treatment of vascular calcifiÂcation. Kidney Int. 2010;78:1232–1239.
Vascular calcification is common in patients with advanced chronic kidney disease and is associated with poorer outcomes. It is clear that it is a multi-factorial process involving altered mineral metabolism, as well as changes in systemic and local factors that can promote or inhibit vascular calcification, and all of these are potential therapeutic targets. Current therapy is closely linked to strategies for preventing disordered bone and mineral metabolism in advanced kidney disease and involves lowering the circulating levels of both phosphate and calcium. The efficacy of compounds that specifically target calcification, such as bisphosphonates and thiosulfate, has been shown in animals but only in small numbers of humans, and safety remains an issue. Additional therapies, such as pyrophosphate, vitamin K, and lowering of pH, are supported by animal studies, but are yet to be investigated clinically.
Rennenberg RJ, de Leeuw PW, Kessels AG, Schurgers LJ, Vermeer C, et al. Calcium scores and matrix gla protein levels: Association with vitamin K status. Eur J Clin Invest. 2010;40:344–349.
In this study they measured arerial calcium scores, the osteocalcin ratio as a proxy for vitamin K status, and ucMGP. They found a positive association of total arterial calcium score and a high OCR (reflecting low vitamin K status) with ucMGP serum levels.
Rennenberg RJMW, van Varik BJ, Schurgers LJ, Hamulyak K, Ten Cate H, et al. Chronic coumarin treatment is associated with increased extracoronary arterial calcification in humans. Blood. 2010;115:5121–5123.
Ronco C, McCullough PA, Anker SD, Anand I, Aspromonte N, Bagshaw SM, et al. Cardiorenal syndromes: An executive summary from the consensus conference of the Acute Dialysis Quality Initiative (ADQI). Contrib Nephrol. 2010;165:54-67.
Schurgers LJ, Barreto DV, Barreto FC, Liabeuf S, Renard C, Magdeleyns EJ, Vermeer C, Choukroun G, Massy ZA. The circulating inactive form of matrix Gla protein is a surrogate marker for vascular calcification in chronic kidney disease: A preliminary report. Clin J Am Soc Nephrol. 2010;5:568–575.
Shroff RC, McNair R, Skepper JN, et al. Chronic mineral dysregulation promotes vascular smooth muscle cell adaptation and extracellular matrix calcification. J Am Soc Nephrol. 2010;21:103-112.
Stenvinkel P. Chronic kidney disease: A public health priority and harbinger of premature cardiovascular disease. J Internal Med. 2010;268:456-457.
Chronic kidney disease has remained a ‘silent’ epidemic. Early diagnosis of renal disease based on proteinuria and/or reduced estimated glomerular filtration rate could enable early intervention to reduce the high risks of cardiovascular events, ESRD and death that are associated with CKD. Leading causes of CKD are hypertension, obesity and diabetes mellitus. CKD may be regarded as a clinical model of accelerated vascular disease and premature ageing, and the risk factor profile changes during the progression from mild/moderate CKD to ESRD. Novel treatment strategies are needed in ESRD.
Takagi K, Masuda K, yamazaki M, Kiyohara C, Itho S, Wasaki M, et al. Metal ion and vitamin absorption profiles of phosphate binder ion-exchange resins. Clin Nephrol. 2010;73(1):30-5.
Wizemann V, Tong L, Satayathum S, et al. Atrial fibrillationin hemodialysis patients: clinical features and associations with anticoagulant therapy. Kidney Int. 2010;77:1098-106.
Fusaro M. Vitamin K: Bone vascular axis in CKD. CIN ‘2011 – 6th Congress of Nephrology in Internet. Available at http://cin2011.uninet.edu/en/trabajos/379.html as of 7-1-2013.
An important point about calcium, and vitamin D supplementation, both in the general population and in the CKD population: without an adequate vitamin K2 intake, calcium will have low chances of being deposited in the bone matrix, but instead will favor the onset or worsening of vascular calcification and cardiovascular disease. No data are available on the survival benefits of calcium supplements and some studies suggest that calcium might be detrimental. The protective role of vitamin k2 on both vascular clacification and vertebral fractures should be studied, in combination with vitamin D treatment and dietary calcium. Adequate levels of vitamin k2 in the circulation could favor a better handling of serum calcium, to maintain bone and vessel health.
Fusaro M. Osteocalcin (Vitamin K-Dependent Protein) Levels are associated with high prevalence of vertebral fractures and vascular calcifications in dialysis patients (EVERFRACT study). Poster session: 2011 Sept 9.
The association of BGP with vetebral fractures and vascular calcification was studied. In 18 Italian dialysis centers, 387 hemodialysis patient,s mean age 64, median dialytic age 49 months, biochemicalmarkers of bone were assessed including Osteocalcin, BGP, ucGP, MGP. The prevalence of asymptomatic VF was determined with a computerized analysis. Bone and mineral parameters indicated that 55% of patients had verbebral fractures and 31% had borderline fractures. Vertebral fractures were associated with age and with reduced BGP. Prevalence of vascular calcification was 80.6% in the aorta and 55.1% in the iliac arteries. Concluded that BGP is an important biomarker of both vertebral fractures and vascular calcification in dialysis patients. They hypothesize that the association between vertebral fractures and vascular calcification is probably due to a common mechanism – vitamin K2 deficiency.
Fusaro M, Crepaldi G, Maggi S, Galli F, D’Angelo A, Calò L, Giannini S, Miozzo D, Gallieni M. Vitamin K, bone fractures, and vascular calcifications in chronic kidney disease: An important but poorly studied relationship. J Endocrinol Invest. 2011;34:317–323.
In patients with chronic kidney disease (CKD), cardiovascular mortality is the first cause of death. Some pathogenetic mechanisms of vascular calcification (such as hyperparathyroidism, hyperphosphatemia, hypercalcemia, role of vitamin D) have been widely investigated, but the potential role of vitamin K is still uncertain. Vitamin K could play a key role, as it transforms glutamic acid residues into γ-carboxyglutamic acid, through a carboxylation process, making both MGP (cMGP) and BGP (cBGP) biologically active. cMGP inhibits vascular calcifications (VC), while cBGP has an important role for a proper mineralization process. Uncarboxylated MGP and BGP (ucMGP and ucBGP) concentrations are indirect markers of vitamin K2 deficiency. The purpose of this review is to analyze the current literature to understand the relationship between vitamin K2 status, fragility fractures and VC in CKD patients. This analysis could be of help in planning investigations of Vitamin K status and its possible supplementation in CKD patients to avert fragility fractures and VC.
Garcia-Canton C, Bosch E, Ramirez A, Gonzalez Y, Auyanet I, Guerra R, et al. Vascular calcification and 250hydroxyvitamin D levels in non-dialysis patients with chronic kidney disease stages 4 and 5. Nephrol Dial Transplant. 2011;28(7):2250-8.
Neven D, D'Haese PC. Calcification in chronic renal failure: What have we learned from animal studies? Circ Res. 2011;108(2):249-64.
The focus for treatment is shifting towards intervening on the circulating concentration of calcification inhibitors that is often disturbed in CKD patients. One promising therapy might be vitamin K, a cofactor responsible for the gamma-carboxylation of MGP and the biological activation of this potent calcification inhibitor. Vitamin K deficiency, as well as increased circulating inactive MGP have been reported in CKD patients and have been associated with a higher degree of vascular calcification. In rats, prevention of calcification from warfarin and regression of calcification with high intake of both vitamin K1 and K2 has been established.
Brandenburg VM, Cozzolino M, Ketteler M. Calciphylaxis: a still unmet challenge. J Nephrol. 2011;24(2):142-8.
Chatrou MLL, Reutelingsperger CP, Schurgers LJ. Role of vitamin K-dependent proteins in the arterial vessel wall. Hamostaseologie. 2011;31(4):251-7.
For many years, the role of vitamin K was ascribed to coagulation. This view has changed dramatically with the discovery of vitamin K-dependent proteins outside the coagulation cascade. Vitamin K-depndent proteins are involved in the regulation of vascular smooth muscle cell migration, apoptosis, and calcification. Vitamin K-antagonists induce inactivity of inhibitors of vascular calcification , leading to accelerated calcification. This review focuses on the effect of vitamin K-dependent proteins in vascular disease.
Fusaro M, Crepaldi G, Maggi S, Galli F, D’Angelo A, Calo L, et al. Vitamin K, bone fractures and vascular calcifications in chronic kidney disease: An important but poorly studied relationship. J Endrocrinol Invest. 2011;34(4):317=23.
Herzog CA, Asinger RW, Berger AK, Charytan DM, Diez J, Hart RG, et al. Cardiovascular disease in chronic kidney disease. A clinical update from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2011;80:572-586.
Hurtado B, Munoz X, recarte-Pelz P, Garcia N, Luque A, Krupinski J, et al. Expression of the vitamin K-dependent proteins GAS6 and protein S and the TAM receptor tyrosine kinases in human atherosclerotic carotid plaques. Thromb Haemost. 2011;105(5):873-82.
The GAS6/ProS-TAM system is composed of two vitamin K-dependent ligans and their three protein tyrosine kinase receptors, TYRO3, AXL, and MERTK. The system plays a prominent role in conditions of injury, inflammation and repair. In murine models, mutations in its components affect atherosclerosis severity. They studied human arteries with different degrees of atherosclerosis and believe the ProS-MERTKreceptors were active in advanced stages of atherosclerosis, while AXL signaling was down-regulated.
Idelevich A, Rais Y, Monsonego-Oman E. Bone Gla protein increases HIF-1alpha-dependent glucose metabolism and induces cartilage and vascular calcification. Arterioscler Thromb Vasc Biol. 2011 Sep;31(9):e55-71.
Ketteler M, Rothe H, Kruger T, biggar PH, Schlieper G. Mechanisms and treatment of extraosseous calcification in chronic kidney disease. Nat Rev Nephrol. 2011;7(9):509-16.
Kapustin AN, Shanahan CM. Osteocalcin: a novel vascular metabolic and osteoinductive factor? Arteriosclerosis, Thrombosis and Vascular Biology. 2011;31:2169-71.
Liu Y, Shanahan, CM. Signalling pathways and vascular calcification. Front Biosci. 2011;l16:1302-14.
London G, Covic A, Goldsmith D, Wiecek A, Suleymanlar G, Ortiz A, et al. Arterial aging and arterial disease: Interplay between central hemodynamics, cardiac work, and organ flow – implications for CKD and cardiovascular disease. Kidney Int Sup. 2011;1:10-12.
Cardiovascular disease is an important cause of morbidity and mortality in patients with chronic kidney disease (CKD) and endpstage renal disease (ESRD). All epidemiological studies have clearly shown that accelerated arterial and cardiac aging is characteristic of these populations.
Mazzaferro S, Pasquali M, Cozzolino M. Treatment of cardiovascular calcification in uremia. Curr Vasc Pharmacol. 2011 Nov;9(6):741-9.
Vascular calcification in uremic subjects is a complex biologic and incompletely understood process that deserves further research, in order to develop specific therapeutic strategies. In general, once established, these calcifications are not considered to be reversible; therefore, prevention is the main treatment option. With this aim, it is now recommended to adopt restricted ranges of serum concentrations for calcium, phosphate and parathyroid hormone which are associated with a lower rate of calcification. Moreover new possible pathogenetic pathways are considered (e.g. vitamin K deficiency).
Neven E, D’Haese PD. Vascular calcification in chronic renal failure: What have we learned from animal studies? 2011 Jan;108(2):249-64.
O’Young J, Liao Y, Xiao Y, Jalkanen J, Lajoie G, Karttunen M, et al. Matrix Gla protein inhibits ectopic calcification by a direct interaction with hydroxyapatite crystals. J Am Chem Soc. 2011;133(45):18406-12.
Pilz S, Tomaschitz A, Friedl C, Amrein K, Drechsler C, et al. Vitamin D status and mortality in chronic kidney disease. Nephrol Dial Transplant. 2011;26(11):3603-3609.
Rezg R, Barreto FD, Barreto DV, Liabeuf S, Drueke TB, Massy ZA. Inhibitors of vascular calcification as potential therapeutic targets. J Nephrol. 2011; 24(04): 416-427. Vascular calcification is frequent in the general population and it contributes to cardiovascular morbidity and mortality in patients with advanced atherosclerosis, in the presence or absence of diabetes mellitus and chronic kidney disease (CKD). Both diabetes and CKD aggravate its degree of severity and accelerate its progression. Vascular calcification is the result of both passive and active processes of calcium phosphate deposition in the arterial wall. These processes are more or less successfully opposed by inhibitory proteins and nonpeptidic factors. In the present overview we discuss the roles of several vascular calcification inhibitors which represent potential therapeutic targets. One possibility could be the administration of vitamin K2.
Ross EA. Evolution of treatment strategies for calciphylaxis. Am J Nephrol. 2011;34(5):460-7.
Schlieper G, Westenfeld R, Kruger T, Cranenburg EC, Magdeleyns EJ, Brandenburg VM, et al. Circulating nonphosphorylated carboxylated Matrix gla protein predicts survival in ESRD. J Am Soc Nephrol. 2011 February;22(2):387–395.
The mechanisms for vascular calcification and its associated cardiovascular mortality in patients with ESRD are not completely understood. Dialysis patients exhibit profound vitamin K deficiency, which may impair carboxylation of the calcification inhibitor matrix gla protein (MGP). Here, we tested whether circulating inactive vitamin K–dependent proteins associate with all-cause or cardiovascular mortality. We observed higher levels of both desphospho-uncarboxylated MGP (dp-ucMGP) and desphospho-carboxylated MGP (dp-cMGP) among 188 hemodialysis patients compared with 98 age-matched subjects with normal renal function. Levels of dp-ucMGP correlated with those of PIVKA-II.. We found increased PIVKA-II levels in (64%) dialysis patients, indicating pronounced vitamin K deficiency. Analysis showed that patients with low levels of dp-cMGP had an increased risk for all-cause and cardiovascular mortality. In 17 hemodialysis patients, daily supplementation with vitamin K2 for 6 weeks reduced dp-ucMGP levels by 27% but did not affect dp-cMGP levels. In conclusion, the majority of dialysis patients exhibit pronounced vitamin K deficiency. Lower levels of circulating dp-cMGP may serve as a predictor of mortality in dialysis patients. Vitamin K supplementation may be a viable pharmacological treatment option for CKD patients with vitamin K deficiency.
Schroff R, Quinlan C, Mitsnefes M. Uraemic vasculopathy in children with chronic kidney disease: prevention or damage limitation? Pediatr Nephrol. 2011 Jun;26(6):853-65.
Shanahan CM, Crouthamel MH, Kapustin A, Giachelli CM. Arterial calcification in chronic kidney disease: Key roles for calcium and phosphate. Circ Res. 2011;109:697-711.
Vascular calcification contributes to the high risk of cardiovascular mortality in chronic kidney disease (CKD) patients. Dysregulation of calcium (Ca) and phosphate (P) metabolism is common in CKD patients and drives vascular calcification. In this article, we review the physiological regulatory mechanisms for Ca and P homeostasis and the basis for their dysregulation in CKD. In addition, we highlight recent findings indicating that elevated Ca and P have direct effects on vascular smooth muscle cells (VSMCs) that promote vascular calcification, including stimulation of osteogenic/chondrogenic differentiation, vesicle release, apoptosis, loss of inhibitors, and extracellular matrix degradation. These studies suggest a major role for elevated P in promoting osteogenic/chondrogenic differentiation of VSMC, whereas elevated Ca has a predominant role in promoting VSMC apoptosis and vesicle release. Furthermore, the effects of elevated Ca and P are synergistic, providing a major stimulus for vascular calcification in CKD. Unraveling the complex regulatory pathways that mediate the effects of both Ca and P on VSMCs will ultimately provide novel targets and therapies to limit the destructive effects of vascular calcification in CKD patients.
Stankowiak-Kulpa H, Krzyzanowska P, Koziol L, Grzymislawski M, Wanic-Kossowski M, Moczko J, Walkowiak J. Vitamin K status in peritoneally dialyzed patients with chronic kidney disease. Acta Biochimica Polonica. 2011;58(4):617-20.
In the present study we aimed to evaluate vitamin K status in patients with CKD who are treated with continuous ambulatory peri-dialysis. Twenty-eight patients entered into the study. Dialysis vintage ranged from 3 to 89 months. Vitamin K status was assessed in all subjects using undercarboxylated prothrombin measurement (PIVKA-II). In addition, total protein and albumin levels, total cholesterol, LDL cholesterol, triglyceride, calcium, urea and creatinine concentrations were determined. PIVKA-II concentrations were abnormal in 13 (46.4 %) subjects. BMI values and LDL cholesterol concentrations were significantly higher in patients with vitamin K deficiency than those without vitamin K deficiency. Moreover, PIVKA II levels correlated with BMI values, LDL cholesterol and creatinine concentrations. In conclusion, vitamin K deficiency is a frequent condition in peritoneally dialyzed patients. Assessment of vitamin K status should become a standard procedure in this group of patients.
2011 US Renal Data System Annual Data Report, 15.1% of the US adult population has CKD.6- 6. US Renal Data System. USRDS 2011 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2011.
Weijs B, Blaauw Y, Rennenberg RJ, Schurgers LJ, Timmermans CC, et al. Patients using vitamin K antagonists show increased levels of coronary calcification: An observational study in low-risk atrial fibrillation patients. Eur Heart J. 2011;32: 2555–62.
Vitamin K antagonists (VKA) are currently the most frequently used drug to prevent ischaemic stroke in Afib patients. However, VKA use has been associated with increased vascular calcification. We investigated VKA use and coronary artery calcification use in low risk AF patients. The data indicated that patients using VKA show increased levels of coronary calcification. Age and VKA treatment were independently related to increased coronary calcium score.
Zak-Golab A, Okopien B, Chudek J. Vitamin K, bone metabolism and vascular calcification in chronic kidney disease. Przegl Lek. 2011;68(9):629-32.
Atherosclerosis is the main cause of premature death in patients with chronic kidney disease, especially if on dialysis. Vitamin K dependent proteins play an essential role in the pathogenesis of mineral and bone disorders related to kidney disease, including vascular calcification. Vitamin K dependent proteins require carboxylation for biological activation. The role of matrix Gla protein (MGP), Growth Arrest Specific Gene 6 (Gas-6) and osteocalcin has been recently discovered. MGP prevents vascular calcification and Gas-6 affects vascular smooth muscle cell apoptosis and movement. Carboxylation of osteocalcin promotes bone formation. The restrictive diet recommended for dialysis patients increases the chance for vitamin K deficiency. More research needs to be done on the clinical consequences of vitamin K deficiency for the peripheral tissues
Zebger Gong H, Muller D, Diercke M, Haffner D, Hocher B, Verberckmoes S, et al. 1,25-Dihydroxyvitamin D3-induced aortic calcifications in experimental uremia: Up-regulation of osteoblast markers, calcium-transporting proteins and osterisx. J Hypertens. 2011;29(2):339-48.
Al Rajabi A, Booth SL, Peterson JW, Choi SW, Suttie JW, Shea MK, et al. Deuterium-labeled phylloquinone has tissue-specific conversion to menaquinone-4 among Fischer 344 male rats. J Nutr. 2012 May;142(5):841-5.
Phylloquinone is converted into menaquinone-4 (MK4) via side chain removal-addition. Following a 14 day phylloquinone deficient diet, male rats were fed phylloquinone with deuterium. Both deuterium phylloquione and deuterium labeled MK$ were detected in tissues. Whereas some tissues had an overall increase in MK4 in response to deuterium phylloquinone, total brain, testes, and fat concentrations did not. The data demonstrate that MK4 is the predominant form of vitamin K in multiple tissues, but there appears to be a tissue-specific regulation for the conversion of phylloquinone to MK4.
Bacchetta J, Salusky IB. Evaluation of hypophosphatemia: Lessons from patients with genetic disorders. Am J Kidney Dis. 2012;59(1):152-9.
Block GA, Wheeler DC, Persky MS, Kestenbaum B, Ketteler M, spiegel DM, et al. Effects of phosphate binders in moderate CKD. J Am Soc Nephrol. 2012 Aug; 23(8):1407-15.
Some propose using phosphate binders in the CKD population given the association between higher levels of phosphorus and mortality, but their safety and efficacy in this population are not well understood. In this study we looked at the effects of phosphate binders on mineral metabolism and vascular calcification among patients with moderate to advanced CKD. We randomly assigned 148 patients to calcium acetate, lanthanum carbonate, sevelamer carbonate, or placebo. Active therapy with these binders significantly increased the calcification of the coronary arteries and the abdominal aorta. In conclusion, phosphate binders did significantly lower serum and urinary phosphorus and attenuate the progression of secondary hyperparathyroidism among patients with CKD, however they also promoted the progression of vascular calcification.
Boxma, P.Y., van den Berg. E, Geleijnse, J.M., Laverman, G.D., Schurgers, L.J, Vermeer, C., Kema, I.P., Muskiet, F.A., Navis, G., Bakken, S.J.L., de Borst, M.H. Vitamin K intake and plasma desphospho-uncarboxylated Matrix gla-protein levels in kidney transplant recipients. PloS One. 2012;7(10):e47991.
The objective of this study was to determine the intake of vitamin K1, vitamin K2 and total vitamin K and vascular vitamin K status, by measuring desphospho-ucMGP (dp-ucMGP) levels, in kidney transplant recipients. Insufficient vitamin K intake leads to production of uncarboxylated, mostly inactive proteins and contributes to an increased cardiovascular risk. In kidney transplant recipients, cardiovascular risk is high but K intake and status have not been defined. Vascular vitamin K status was assessed by measuring plasma desphospho-uncarboyxlated MGP. Total vitamin K intake was below the recommended level in 50% of patients. Indeed, in our study even the subjects with adequate vitamin K intake according to U.S. guidelines still had median dp-ucMGP levels above the recommended level, suggesting vascular vitamin K insufficiency and suggesting that the dietary guidelines are grossly inadequate. Analysis identified creatinine clearance, coumarin use, body mass index, high sensitivity CRP and sodium excretion as independent determinants of dp-ucMGP levels. Concluded vitamin K intake is too low for maximal carboxylation of vascular MGP. The high dp-ucMGP levels may result in an increased risk for arterial calcification. This suggests that either kidney transplant recipients should be recommended to increase their dietary vitamin K intake beyond amounts recommended to the general population, or these patients should be supplemented with extra vitamin K.
Busch M, Stein A, Stein G. How to manage functional vitamin K deficiency in CKD. American J of Kid Dis. 2012 July;60(1):168.
We determined undercarboxylated and carboxylated osteocalcin levels, as well as vitamin K1 (phylloquinone) in 39 hemodialysis patients with biopsy-proven high-turnover renal osteodystrophy; 25 men, 14 women and 71 age-matched controls. Compared with controls, hemodialysis patients had significantly higher levels of not only undercarboxylated osteocalcin, but also carboxylated osteocalcin (and consequently, total osteocalcin; P < 0.001), probably related to increased bone turnover. Similar to other findings, undercarboxylated osteocalcin constituted 49% ± 22% of the total osteocalcin in hemodialysis patients, which was not significantly different from controls. Phylloquinone levels were significantly higher in hemodialysis patients (P < 0.001), probably due to accumulation. Apparently, the conversion from vitamin K1 to K2 is disturbed in chronic kidney disease. Because vascular calcification and also vitamin K status are related to bone turnover, the question arises of whether supplementation would benefit all hemodialysis patients or only certain subgroups, depending on their bone turnover status.
Cancela AL, Santos RD, Titan SM, Goldenstein PT, Rochitte CE, Lemos PA. Phosphorus is associated with coronary artery disease in patients with preserved renal function. PloS One. 2012;7(5):e36883.
Chatrou ML, Winckers K, Hackeng TM, Reutelingsperger CP, Schurgers LJ. Vascular calcification: the price to pay for anticoagulation therapy with vitamin K-antagonists. Blood Rev. 2012 Jul;26(4):155-66.
Several lines of evidence indicate that VKA-vitamin K antagonists- inhibit not only post-translational activation of vitamin K-dependent coagulation factors but also synthesis of functional extra-hepatic vitamin K-dependent proteins, thereby eliciting undesired side-effects. Vascular calcification is one of the recently revealed side-effects of VKA. This review addresses vitamin K-cycle and vitamin K-dependent processes of vascular calcification that are affected by VKA. We conclude there is a growing need for better understanding of the effects of anticoagulants on calcification and atherosclerosis.
Chauhan V, Kelepouris E, Chauhan N, Vaid M. Current concepts and management strategies in chronic kidney disease-mineral and bone disorder. Southern Med J. 2012 Sept;105(9):479-85.
Cozzollino M, Rizzo, MA, Stucchi A, Cusi D, Gallieni M. Sevelamer for hyperphosphataemia in kidney failure: Controversy and perspective. Ther Adv Chronic Dis. 2012 (Mar;3(2):59-68.
Cranenburg EC, Schurgers LJ, Uiterwijk HH, Beulens JW, Dalmeijer GW, et al. Vitamin K intake and status are low in hemodialysis patients. Kidney Int. 2012;82:605–610.
Vitamin K is essential for the activity of γ-carboxyglutamate (Gla)-proteins including matrix Gla protein and osteocalcin; an inhibitor of vascular calcification and a bone matrix protein, respectively. Insufficient vitamin K intake could contribute to the high risk of vascular calcification in hemodialysis patients. In this study, we measured vitamin K1 and K2 intake (4-day food record), and the vitamin K status in 40 hemodialysis patients. The intake was low in these patients (median 140 μg/day), especially on days of dialysis and the weekend. Non-carboxylated bone and coagulation proteins were found to be elevated in 33 hemodialysis patients, indicating subclinical hepatic vitamin K deficiency. Additionally, very high non-carboxylated matrix Gla28 protein levels, endemic to all patients, suggest vascular vitamin K deficiency. Thus, compared to healthy individuals, hemodialysis patients have a poor overall vitamin K status due to low intake. A randomized controlled trial is needed to test whether vitamin K supplementation reduces the risk of arterial calcification and mortality in hemodialysis patients.
Diener HC, Eikelboom J, Connolly SJ, Joyner CD, Hart RG, Lip GY, et al. AVERROES Steering Committee and Investigators. Apixaban versus aspirin in patients with atrial fibrillation and previous stroke or transient ischaemic attack: a predefined subgroup analysis from AVERROES, a randomised trial. Lancet Neurol. 2012;11:225–231.
Fusaro M, D’Angelo A, Gallieni M. Consequences of vitamin k2 deficiency in hemodialysis patients. Am J Kidney Dis. 2012 Jul;60(1):169.
They respond to a previous publication, mentioning that vitamin K intake can affect not only matrix Gla protein activity, which is relevant to cardiovascular calcification, but also osteocalcin (bone Gla protein) activity. The latter pathway, may protect against loss of bone mineral density and deterioration in the quality of bone structure. In a randomized controlled study of 334 early menopausal Norweigian women, half of whom were treated with vitamin K2 (360 ug of MK7), at 12 months there was no signficant effect on bone loss, but there was a significant reduction in levels of undercarboxylated osteocalcin. Therefore we suggest that adequate levels of circulating vitamin K could be important to maintain vascular health as well as bone health in patients with CKD, and possibily in the general population.
Fusaro M, Noale M, Viola V, Galli F, Tripepi G, Vajente N, et al. Vitamin K, vertebral fractures, vascular calcifications, and mortality: Vitamin K Italian (VIKI) dialysis study. J Bone Miner Res. 2012 Nov;27(11):2271-8.
Low vitamin K concentrations are associated with increased risks of fractures, vascular calcification and frequent complications in hemodialysis patients. This study looked at the prevalence of vitamin K deficiency and the relationship between fractures, calcifications and survival in 387 patients on hemodialysis. 35% had MK7 deficiency, 24% had vitamin K1 deficiency, and 15% had MK4 deficiency. K1 deficiency was the strongest predictor of vertebral fractures. MK4 deficiency was a predictor of aortic calcification and MK7 deficiency was a predictor of iliac calcification. They concluded that the vitamin K system was important to preserve bone mass and avoid vascular calcification in hemodialysis patients.
Gao B, Yasui T, Tozawa K, Hayashi Y, Kohri K. A polymorphism of matrix Gla protein is associated with kidney stones in the Chinese Han population. Gene. 2012;511(2):127-130.
Matrix Gla protein, a potent calcification inhibitor in arterial vessels, is also expressed in the kidney and is up-regulated following the administration of ethylene glycol, a precursor of oxalate. Considering the analogous characteristics between arterial calcification and kidney stones, we identified variants of the human matrix Gla protein gene and investigated whether there is an association between MGP genetic polymorphisms and kidney stones.
Hayashi M, Takamatsu I, Kanno Y, Yoshida T, Abe T, Sato Y et al. A case-control study of calciphylaxis in Japanese end-stage renal disease patients. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc- Eur Ren Assoc. 2012;27(4):1580-4.
Hill KM, Martin BR, Wastney ME, McCabe GE, Moe SM, Weaver CM, et al. Oral calcium carbonate affects calcium but not phosphorus balance in stage 3–4 chronic kidney disease. Clinical Trial Kidney International. advance online publication 19 December 2012.
Jamal SA, Moe SM. Calcium builds strong bones, and more is better –correct? Well, maybe not. Clin J Am Soc Nephrol. 2012 Nov;7(11):1877-83.
Calcium supplementation has been considered the gold standard therapy for osteoporosis in the general population. It is given in both the placebo and treatment groups of trials that evaluate antifracture efficacy of new therapies. Similarly, calcium-based phosphate binders have been considered the gold standard comparator for all new phosphate binders. However, large randomized trials demonstrate conflicting data on the antifracture efficacy of calcium supplementation, particularly in high doses, in patients with osteoporosis without CKD. In addition, recent data suggest an increased risk for cardiovascular events. These new studies raise safety concerns for the general approach with calcium supplementation and binders. This review describes recent data on the adverse effects of calcium supplementation for osteoporosis and how these new data should affect the strategy for phosphate binder use in CKD.
Koizumi M, Fukagawa M. Kidney and bone update: The 5-year history and future of CKD-MBD. The changes after the introduction of CKD-MBD as a new entity. Clin Calcium. 2012 Jul;22(7):969-77.
Recent clinical studies have indicated that mineral metabolism disorder in chronic kidney disease (CKD) is not a disease confined to bone, but a systemic disease that determines prognosis by promoting vascular calcification. In the context of this paradigm shift, KDIGO (Kidney Disease: Improving Global Outcomes) introduced a new disease entity "CKD-bone and mineral disorder (MBD) " in 2005, and released clinical practice guidelines on the management of CKD-MBD in 2009. This guideline is based on strict systemic evidence review and has had considerable effect on clinical practice. However, on the other hand, it became apparent that only a few clinical studies could support the recommendation of this guideline with high-quality evidence. There is a compelling need for accumulation of clinical findings with high-quality evidence.
Lee IJ, Hilliard B, Swami A, Madara JC, Rao S, Patel T, et al. Growth arrest-specific gene 6 (Gas6) levels are elevated in patients with chronic renal failure. Nephrol Dial Transplant. 2012;27(11):4166-72.
Dysregulation of circulating Gas6 is associated with renal disease and inversely proportional to renal function.
Lewis R. Mineral and bone disorders in chronic kidney disease: New insights into mechanism and management. Ann Clin Biochem. 2012 Sep; 49(pt 5):432-40.
Chronic kidney disease (CKD) is now recognized as a major public health issue. One consequence of this condition is disturbance of mineral and bone homeostasis. Bone disease (renal osteodystrophy) as a consequence of CKD has long been recognized. However, it is now appreciated that the mineral and bone disturbances of CKD (and perhaps treatment of them) lead to vascular calcification, which is a cause of significant morbidity. In recognition of the widespread nature of the condition, the term CKD-mineral bone disorder (CKD-MBD) is now in general use to describe the biochemical, skeletal and vascular changes that occur in CKD. This review describes the classification of CKD and current understanding of the mechanisms underlying CKD-MBD.
Li R, Li X, Zhou M, Han H, Zhang Q. Quantitative determination of matrix Gla protein (MGP) and BMP-2 during the osteogenic differentiation of human peridontal ligament cells. Arch Oral Biol. 2012 Oct;57(10):1408-17.
Lu X, Gao B, Liu Z, Tian X, Mao X, Emmanuel N, Zhu Q, Xiao C. A polymorphism of matrix Gla protein gene is associated with kidney stone in the Chinese Han population. Gene. 2012;511:127–130.
Matrix Gla protein (MGP) is a molecular determinant regulating the extracellular matrix calcification. To further confirm whether the MGP genetic polymorphism was universally associated with the risk of kidney stone, we investigated the association of genetic polymorphisms of MGP with kidney stone in the Chinese Han population. Our findings showed that SNPrs4236 of the MGP gene is associated with kidney stones in the Chinese Han population, and influences the genetic susceptibility to kidney stones.
Lu x, Gao B, Yasui T, Li Y, Liu T, Mao X, et al. Matrix gla protein is involved in crystal formation in kidney of hyperoxaluric rats. Kidney Blood Press Res. 2013;37(1):15-23.
Matrix Gla protein (MGP is a molecular determinant regulating vascular calcification of the extracellular matrix. An animal study suggests that MGP are involved in crystal formation by continuous expression, distributing it in the renal tubular cells and binding directly to the crystals.
Nemczik, J, Kiss, I, Tisler A. Arterial stiffness, vascular calcification and bone metabolism in chronic kidney disease. World J Nephrol. 2012 Feb 6;1(1):25-34.
Patients with CKD have an extremely poor cardiovascular outome. Arterial stiffness, a strong independent predictor of survival in CKD is connected to arterial media calcification, a process which is in parallel with impaired bone metabolism. Due to growing evidence, the definition of “CKD mineral bone disorder” was created underlying the strong connection of the two phenomena. They review the up-to-date data of the bone-vascular axis in CKD.
O'Seaghda CM, Hwang SJ, Holden R, Booth SL, Fox CS. Phylloquinone and vitamin D status: Associations with incident chronic kidney disease in the Framingham Offspring cohort. Am J Nephrol. 2012;36(1):68-77.
Cardiovascular risk factors are associated with the development of chronic kidney disease (CKD), and chronic kidney disease and vascular disease are etiologically linked. Evidence suggests deficiencies of vitamins D and K may adversely affect the cardiovascular system, but data from longitudinal studies are lacking. They hypothesized that deficiencies of vitamins D and K may be associated with incident CKD and/or incident albuminuria amongst the general population. They analyzed 1,442 Framingham Heart Study participants (mean age 58 years; 50.5% women), free of CKD with a mean follow-up of 7.8 years in 2005-2008. Baseline plasma phylloquinone (vitamin K(1)) and vitamin D levels,were related to risk of incident CKD and incident albuminuria. They found that participants in the highest phylloquinone quartile had an increased risk of CKD and albuminuria at follow-up, whereas no association was observed with continuous phylloquinone levels for either endpoint. Deficiency of 25(OH)D was not associated with incident CKD or albuminuria in either analysis.
Schurgers et al., 2012. Schurgers LJ, Joosen IA, Laufer EM, Chatrou MLL, Herfs M, et al. Vitamin K-antagonists accelerate atherosclerotic calcification and Induce a vulnerable plaque phenotype. PLoS ONE 2012;7(8): e43229.
Vitamin K-antagonists (VKA) are treatment of choice and standard care for patients with venous thrombosis and thromboembolic risk. In this study, they investigated the effect of VKA on coronary calcification in patients and on calcification of atherosclerotic plaques in the ApoE−/− model of atherosclerosis. Significanct VKA use is associated with coronary artery plaque calcification in patients with suspected CAD and causes changes in plaque morphology with features of plaque vulnerability in ApoE−/−mice. Warfarin significantly increased frequency and extent of vascular calcification. Also plaque calcification comprised microcalcification of the intimal layer. Our findings underscore the need for alternative anticoagulants that do not interfere with the vitamin K cycle.
Shea, MK, Holden RM. Vitamin K status and vascular calcification: Evidence from observational and clinical studies. Adv Nutr. 2012 Mar; 3:158-165.
The available observational, population-based evidence, based on dietary intake measures, suggests menaquinone intake may be more likely to protect against vascular calcification than phylloquinone intake. There are no published intervention studies yet, of menaquinone, that measures vascular calcification as an outcome and this should be clarified in future trials. Patients with chronic kidney disease represent a rapidly growing segment of increased risk for vitamin K deficiency, and the role of vitamin K in reducing vascular calcification merits exploration.
Thompson B, Towler DA. Arterial calcification and bone physiology: Role of the bone-vascular axis. Nat Rev Endocrinol. 2012 Sep;8(9):529-43.
Bone never forms without vascular interactions. The vascularture is the location for nutrient exchange between bone and the rest of the body. The second most calcified structure in humans after the skeleton is the vasculature. Vascular calcification has emerged as an actively regulated form of tissue biomineralization. Skeletal morphogens and osteochondrogenic transcription factors are expressed by cells within the vessel wall, which regulates the deposition of vascular calcium. Hormones, including the parathyroid hormone regulate both vascular and skeletal mineralization. Cellular, endocrine and metabolic signals flow bidirectionally between the vasculature and bone and are necessary for both bone health and vascular health. Dysmetabolic states including diabetes, uremia and hyperlipidaemia perturb the bone-vascular axis, giving rise to vascular and skeletal disease. A detailed understanding of these interactions is necessary to address the unmet clinical needs of an increasingly aged and dysmetabolic population.
Westenfeld, R., Krueger, T., Schlieper, G., Cranenburg, E.C.M., Magdeleyns, E.J., Heidenreich, S., Holzmann, S., Vermeer, C. Jahnen-Dechent, W., Ketteler, M., Floege, J., Schurgers, L.J. Effect of vitamin K2 supplementation on functional vitamin K deficiency in hemodialysis patients: A randomized trial. Am. J. Kidney Dis. 2012;59:186-195.
Vascular calcification is a predictor of cardiovascular morbidity and mortality. Hemodialysis patients experience severe vascular calcifications. Matrix Gla protein (MGP) is a central calcification inhibitor of the arterial wall; its activity depends on vitamin K carboxylation. Recent studies suggest poor vitamin K status in hemodialysis patients. They aimed to investigate whether daily vitamin K supplementation improves the bioactivity of vitamin K-dependent proteins in hemodialysis patients. 54 long-term hemodialysis patients in stable conditions, 18 years or older were studied along with 50 healthy age-matched individuals as the control group. Menoquinone-7 (vitamin K2) treatment at 45, 135 or 360 ug/d was given for 6 weeks. The study confirms that most hemodialysis patients have a functional vitamin K deficiency. More importantly, it is the first study showing that inactive MGP levels can be decreased markedly by daily vitamin K2 supplementation. Their study provides the rationale for intervention trials aimed at decreasing vascular calcification in hemodialysis patients by vitamin K supplementation.
Aggarwal KP, Narula K, Kakkar M et al. Nephrolithias: molecular mechanism of renal stone formation and the critical role played by modulators. Bio Med Res Int. 2013;2013:1-21.
Bansal N, Fan D, et al. Incident atrial fibrillation and risk of end-stage renal disease in adults with chronic kidney disease. Circulation. 2013;127(5):569-574.
Gallieni M, Rizzo MA, Maggi S, Regalia A, Molfino I, Crepaldi G, et al. Vitamin K and bone metabolism in the elderly with normal and reduced kidney function. European Ger Med. 2013 Feb;4(1):32-38.
The geriatric population, who is often affected by bone disorders frequently related to aging itself, could benefit from a supplementation of vitamin K, but further studies are necessary to prove actual benefits, both in CKD patients and in the general population. In patients at risk of vascular calcifications and fractures, in particular elderly patients affected by CKD, the possible beneficial role of vitamin K supplementation, as well as more a selected administration of vitamin K inhibitors for anticoagulation should be considered.
Goiko M, Dierolf J, Gleberzon JS, et al. Peptides of matrix Gla protein inhibit nucleation and growth of nydroxyapatite and calcium oxalate monohydrate crystals. PloS One. 2013;8:e80344.
Matrix Gla protein prevents the deposits of crystals in the walls blood vessels. MGP is active in the kidney and mya inhibit the formation of kidney stones. This study looked at how MGP prevents soft-tissue calcification, and concluded it inhibits the formation of the crystals. Based on these findings, they proposed that MGP prevent blood vessell calcification but also inhibits kidney stone formation.
Hill KM, Martin BR, Wastney ME, McCabe GP, Moe SM, Weaver CM, Peacock M. Oral calcium carbonate affects calcium but not phosphorus balance in stage 3-4 chronic kidney disease. Kidney Int. 2013;83:959-966.
This 3-week placebo-controlled balance and kinetic study demonstrated that stage 3/4 CKD patients were in neutral calcium balance while consuming a diet adequate in calcium containing 957 mg per day. Increasing calcium intake with 500 mg calcium from calcium carbonate taken with three daily meals produced positive calcium balance, and was stored in bodily tissues. This study is the first balance study in CKD to include both calcium and phosphorus balance and calcium kinetics, and to evaluate the effects of calcium carbonate on these measures. These results challenge the rationale for using calcium-based phosphate binders in stage 3/4 CKD patients to prevent negative calcium balance, reduce PTH, reduce serum phosphate, and prevent phosphorus retention because: (1) patients were not in negative calcium balance or positive phosphorus balance on placebo and (2) calcium carbonate did not affect serum PTH, serum phosphate, or phosphorus balance. Although it is unknown whether the calcium retained from calcium carbonate is deposited into bone or soft tissue in these patients, it is unlikely that bone could serve as the sole reservoir considering the magnitude of the positive calcium balance and the patients’ age. Therefore, the positive calcium balance produced by calcium carbonate cautions against its use as a phosphate binder in stage 3/4 CKD patients.
Holden RM, Booth SL, Day AG, Clase CM, Zimmerman D, Moist L, et al. Inhibiting the progression of arterial calcification with vitamin K in Hemodialysis patients (iPACK-HD) Trial: Rationale and study design for a randomized trial of vitamin K in patients with end stage kidney disease. Can J Kidney Health Dis. 2013;2:17.
Krueger T, Schlieper G, Schurgers L, Cornelis T, Cozzolino M, Jacobi J, et al. Vitamin K1 to slow vascular calcification in haemodialysis patients (vitavask trial): A rationale and study protocol. Nephrol. Dial Transplant. 2013;29:1633-38.
Kurnatowska L, Grzelak P, Kaczmarska, Masajtix-Zagajewska A, Kaczmarska M, Stefancyzk L, Nowick M. Effect of vitamin K substitution on vascular calcification and early atherosclerotic changes in patients with chronic kidney disease - preliminary results. Nephrol Dial Transplant. 2013;28(Suppl 1):1352-57.
Although vitamin K2 may be protective against vascular calcification, the role of vitamin D in promoting atherosclerosis and vascular calcification remains much more controversial. In this study, patients with CKD stage 3-5 not requiring dialysis who also had coronary artery calcification (CAC score >30) were studied. The subjects received a daily dose of either 90 ug of menaquinone (vitamin K2) + 10 of ug of cholecalciferol (K+D group) or 10 ug of cholecalciferol on (D group) for 270 days. Intima media thickness in carotid artery was measured, and CAC score was assessed at baseline and at end of the treatment. Serum calcium, phosphate, parathyroid, lipids, uric acid and C-reactive protein were also measured. There were no significant changes of renal function during the study. There was a significant increase of serum phosphate in patients of the low dose vitamin D group, but not in the K+D group. Parathyroid tended to increase in the K+D group, but remained unchanged in the D group. CAC score increased in both groups during the treatment, numerically less in the vitamin K+D patients. In 5 of 26 patients treated with vitamin K there was a regression of the CAC score, and in 2 of 26 patients treated with vitamin K, their CAC remained stable and did not increase. In contrast, all subjects treated only with vitamin D experienced a progression of calcification. The thickening of the carotid artery was significantly less in the K+D group. Vitamin K2 therapy may slow the progression of atherosclerosis and vascular calcification in non-dialyzed CKD patients.
Lu X, Gao B, Yasui T, Li Y, Liu T, Mao X et al. Matrix Gla protein is involved in crystal formation in kidney of hyperoxaluric rats. Kidney Blood Press Res. 2013;37:15-23.
McCabe KM, Booth SL, Fu X, Shobeir N, Pang JJ, Adams MA, Holden RM. Dietary vitamin K and therapeutic warfarin alter the susceptibility to vascular calcification in experimental chronic kidney disease. Kidney International. 2013;83(5):835-44.
The leading cause of death in patients with chronic kidney disease (CKD) is cardiovascular disease, with vascular calcification being a key modifier of disease progression. A local regulator of vascular calcification is vitamin K. This γ-glutamyl carboxylase substrate is an essential cofactor in the activation of several extracellular matrix proteins that inhibit calcification. Warfarin, a common therapy in dialysis patients, inhibits the recycling of vitamin K and thereby decreases the inhibitory activity of these proteins. In this study, we sought to determine whether modifying vitamin K status, either by increasing dietary vitamin K intake or by antagonism with therapeutic doses of warfarin, could alter the development of vascular calcification in male Sprague–Dawley rats with adenine-induced CKD. Treatment of CKD rats with warfarin markedly increased pulse pressure and pulse wave velocity, as well as significantly increased calcium concentrations in the thoracic aorta (3-fold), abdominal aorta (8-fold), renal artery (4-fold), and carotid artery (20-fold). In contrast, treatment with high dietary vitamin K1 increased vitamin K tissue concentrations (10–300-fold) and blunted the development of vascular calcification. Thus, vitamin K has an important role in modifying mechanisms linked to the susceptibility of arteries to calcify in an experimental model of CKD.
McCabe KM, Adams MA, Holden RM. Vitamin K status in chronic kidney disease. Nutrients. 2013 Nov;5110;4390-98.
This review summarizes the research on vitamin K status in chronic kidney disease (CKD), including the link between vitamin K deficiency in CKD and bone dynamics. It also describes two ongoing clinical trials evaluating vitamin K treatment in CKD patients. Patients with CKD are at a marked risk for cardiovascular disease and bone fracture. There is also a high prevalence of vitamin K deficiency within the CKD population. The type of vitamin K, MK4, appears to be the major form which protects against vascular calcification and bone loss. And vitamin K may represent a risk factor that can be modified through supplementation. These randomized, placebo-controlled trials examine whether vitamin K supplementation prevents the progression of calcification in this population. The European study (VitaVasK) is randomizing hemodialysis patients to 5 mg of vitamin K three times weekly for 18 months. The Canadien study (iPack-HD study) is randomizing incident hemodialysis patients to 10 mg of vitamin K thrice weekly for 12 months.
National Kidney and Urologic Diseases Information Clearinghouse (NKUDIC). 2013. Retrieved July 1, 2013, from http://kidney.niddk.nih.gov/kudiseases/pubs/yourkidneys.
Shanahan CM. Mechanisms of vascular calcification in CKD—evidence for premature ageing? Nat Rev Nephrol. 2013; 9: 661–670.
Stenvinkel P, Larsson TE.. Chronic kidney disease: a clinical model of premature aging. Am J Kidney Dis. 2013; 62: 339–351.
Premature aging is a process associated with a progressive accumulation of deleterious changes over time, an impairment of physiologic functions, and an increase in the risk of disease and death. Chronic kidney disease is a common condition that promotes cellular senescence and premature aging through toxic alterations in the internal milieu. This occurs through several mechanisms, including DNA and mitochondria damage, increased reactive oxygen species generation, persistent inflammation, stem cell exhaustion, phosphate toxicity, decreased klotho expression, and telomere attrition.
Textbook of Orthopaedics. 2013. Retrieved July 1, 2013 from http://WheelessOnline.com.
Theusweissen E, Teunissen K, Spronk H, Hamulyak K, Cate HT, Shearer M, et al. Effect of low-dose supplements of menaquinone-7 (vitamin k2 on the stability of oral anticoagulant treatment: Dose-response relationship in healthy volunteers. J Thromb Haemost. 2013 Mar 26. Epub ahead of print).
Despite the worldwide use of vitamin K antagonists (VKA), there is limited knowledge of the influence of dietary vitamin k on anticoagulation control. In view of the increasing availability of MK7 for bone and cardiovascular health, it is important to determine the posology. After rendering healthy men and women anticoagulated, and then giving 45 ug of MK7, circulating ucOC and dp-ucMGP were not affected. They did find that MK7 supplementation at doses as low as 10 ug significantly influenced anticoagulation sensitivity in some individuals.
Schurgers LJ. Vitamin K: Key vitamin in controlling vascular calcification in chronic kidney disease. Kidney Int. 2013;83:782-784.
Vascular calcification has emerged as an independent risk factor for cardiovascular morbidity and mortality, especially in chronic kidney disease. Deficiencies in calcium-regulatory proteins directly related to development of calcifications. McCabe and colleagues report that vitamin K is a key regulator of vascular calcification, via carboxylation of vitamin K-dependent proteins such as matrix Gla protein. Knowledge about vitamin K status may propel therapeutic strategies to prevent and treat vascular calcification with high vitamin K supplementation.
Vaziri, ND, Wong J, Pahl M, Piceno YM, Yuan, J, DeSantis TZ, et al. Chronic kidney disease alters intestinal microbial flora. Kidney International. 2013;83:308-315.
The population of microbes in the intestine is a symbiotic ecosystem conferring trophic and protective functions. They determined that uremia and/or dietary and pharmacologic interventions in CKD alters the microbiome. They found marked differences between people with CKD and a healthy population, with decreases in the abundance of Lactobacillaceae and Prevotellaceae families. They concluded that uremia profoundly alters the composition of gut microbiome.
Voong K, Harrington D, Goldsmith D. Vitamin K status in chronic kidney disease: A report of a study and a mini-review. International Urology and Nephrology. 2013 Jan 8; Epub ahead of print)
Vitamin K-dependent proteins (e.g., Factors II, VII, IX and X) form part of the clotting cascade. Vitamin K is also required for the normal function of Matrix Gla Protein (MGP)—one of several non-clotting related extra-hepatic vitamin K-dependent proteins. MGP is known to have protective action against vascular calcification—indeed it is a powerful tissue-bound inhibitory mechanism and can be found in blood vessel walls. MGP is also dependent on activation by γ-glutamyl carboxylase enzyme to convert Glu residues in its amino acid sequence to Gla. This reaction can only take place when the enzyme is activated in the presence of vitamin K . It is of great potential interest to investigate whether subtle deficiencies of vitamin K may, through its effect on the action of MGP, be a contributing factor to vascular calcification in CKD patients, in whom CV disease is greatly accelerated and in whom vascular calcification is not only common, but progresses aggressively, and is something for which as yet there is no clinically applicable remedy.
Yamashita T., Okano K., Tsuruta Y., Akiba T., Nitta K. Serum osteocalcin levels are useful as a predictor of cardiovascular events in maintenance hemodialysis patients. Int. Urol. Nephrol. 2013;45:207–214.
Caluwe R, Vandecasteele S, Van Vlem B, Vermeer C, De Vriese AS. Vitamin K2 supplementation in haemodialysis patients: a randomized dose-finding study. Nephrol Dial Transplant. 2014;29(7):1385-1390.
Haemodialysis patients suffer from accelerated vascular calcification. The vitamin K-dependent matrix Gla protein (MGP) is one of the most powerful inhibitors of vascular calcification. Haemodialysis patients have high levels of the inactive form of MGP. In this study, 200 chronic dialysis patients received 360, 720 or 1080 ug of MK7 three times weekly for 8 weeks. The MK7 supplementation dose dependently reduced the level of inactive MGP, by 17, 33, and 46% in the respective groups. The researchers concluded that MK7 (menaquinone) supplementation may be a novel approach to prevent vascular calcification in chronic dialysis patients.
Cheung CL, Sahni S, Cheung BM. Vitamin K intake and mortality in people with chronic kidney disease from NHANES III. Clin Nutr. 2014;pii: S0261-5614(14)00086-7. doi:10.1016/j.clnu.2014.03.011, in press.
This study looked at the association between intakes of vitamin K with all cause and CVD mortality among CKD patients from the Third National Health and Nutrition Examination Survey (NHANES). The mean age was 61.9 years, and 2/3 of the sample were women. The mean dietary intake was 97.5 ug, which is lower than the general population intake. 72% had lower vitamin K intake. Participants with inadequate vitamin K intake had significantly higher all cause and CVD mortality compared to those with adequate intake. They found that adequate vitamin K intake was robustly associated with mortality, supporting the possibility that vitamin K intake may have a threshold effect. Achieving adequate vitamin K intake may be important in CKD patients.
Elliott MJ, Booth SL, Hopman WM, Holden RM. Assessment of potential biomarkers of subclinical vitamin K deficiency in patients with end-stage kidney disease. Can J Kidney Heal Dis. 2014;1:13.
In this study, they found that a significant proportion of HD patients met criteria for subclinical vitamin K deficiency. Of the biomarkers measured, PIVKA-II may be superior given its independence of renal function or dyslipidemia, both of which may confound the other vitamin K biomarkers. Studies in patients with End Stage Kidney Disease linking biomarkers of vitamin K status to important patient outcomes, including cardiovascular disease, nutritional status and mortality, are required in order to determine the optimal biomarker for evaluating vitamin K status in this particular population.
Gallieni M, Fusaro M. Vitamin K and cardiovascular calcification in CKD: is patient supplementation on the horizon. Kidney International. 2014;86:232-234.
The vitamin K-dependent proteins, such as matrix Gla protein and osteocalcin protect from cardiovascular calcifications and bone fractures. Kidney disease can interfere with vitamin K dependent proteins, contributing to vitamin K deficiency. Current clinical trials in Europe and in Canada are evaluating whether vitamin K1 supplementation will reduce the progression of coronary artery calcifications for folks with chronic kidney disease. Additional research investigating the effect of vitamin K2 for people with CKD is recommended.
Kaesler N, Magdeleyns E, Herts M, Schettgen T, Brandenburg V, Fliser D. Impaired vitamin K recycling in uremia is rescued by vitamin K supplementation. Kidney International. 2014 Aug;86(2):286-293.
In chronic kidney disease, vitamin K deficiency may contribute to the uremic vascular calcification. In this study, uremia was induced in rats. As expected, their undercarboxylated matrix Gla protein increased, indicating vitamin K deficiency. Within seven weeks, there was overt calcification in the aorta, heart and kidneys. When supplementation of vitamin K began, within four weeks, the carboxylation of mGp was restored and the aortic and renal calcium content was reduced.
Ketteler M, Rothe H, Brandenburg VM, Westenfeld R. The K-factor in chronic kidney disease: biomarkers of calcification inhibition and beyond. Nephrol Dial Transplant. 2014 Jul;29(7):1267-70.
There is a huge body of unambiguous evidence that cardiovascular calcification represents one of the most stringent mortality risk factors for patients suffering from chronic kidney disease (CKD). A key calcification inhibitor is vitamin K-dependent matrix Gla protein (MGP). MGP function appears to be sub-optimal in CKD patients and thus MGP may be an appealing and promising target for a treatment intervention.
Kooman JP, Kotanko P, Schols A. et al. Chronic kidney disease and premature ageing. Nat Rev Nephrol 2014; 10: 732–742.
Chronic kidney disease (CKD) shares many phenotypic similarities with other chronic diseases, including heart failure, chronic obstructive pulmonary disease, HIV infection and rheumatoid arthritis. The most apparent similarity is premature ageing, involving accelerated vascular disease and muscle wasting. We propose that in addition to a sedentary lifestyle and psychosocial and socioeconomic determinants, four major disease-induced mechanisms underlie premature ageing in CKD: an increase in allostatic load, activation of the 'stress resistance response', activation of age-promoting mechanisms and impairment of anti-ageing pathways. The most effective current interventions to modulate premature ageing-treatment of the underlying disease, optimal nutrition, correction of the internal environment and exercise training-reduce systemic inflammation and oxidative stress and induce muscle anabolism.
Mac-Way F., Poulin A., Utescu M.S., De Serres S.A., Marquis K., Douville P., Desmeules S., Larivière R., Lebel M., Agharazii M. The impact of warfarin on the rate of progression of aortic stiffness in hemodialysis patients: A longitudinal study. Nephrol. Dial. Transpl. 2014;29:2113–2120.
An observational study reported that the use of VKAs is related with increased aortic stiffness in end-stage CKD patients undergoing haemodialysis (HD).
Nagata Y, Inaba M, Imanishi Y, Okazaki H, Yamada S, Mori K et al. Increased undercarboxylated osteocalcin/intact osteocalcin ratio in patients undergoing hemodialysis. Osteoporosis Int. 2014;26:1053-61.
Serum ucOC/iOC ratio >1.0 was observed in as high as 71.4% of HD patients, preferentially with high bone turnover state, in comparison with pre-dialysis CKD patients. These data suggested that serum ucOC/iOC ratio might lose its significance as a bone metabolic marker to indicate vitamin K deficiency in HD patients.
Keyzer CA, Vermeer C, Joosten MM, Knapen MH, Drummen NE, Navis G et al. Vitamin K status and mortality after kidney transplantation: a cohort study. Am J Kidney Dis. 2015 Mar;65(3):474-83.
Vitamin K modulates calcification by activating calcification inhibitors such as matrix Gla protein (MGP). In kidney transplant recipients, vitamin K insufficiency is common, but implications for long-term outcomes are unclear. 518 stable kidney transplant recipients were studied for their levels of dephosphorylated-uncarboxylated MGP (dp-ucMGP) levels, which are thought to reflect vitamin K status. Patients in the top quartile of dp-ucMGP, meaning they had the lowest amount of vitamin K, were at a higher risk of developing transplant failure and dying. Future studies should address whether vitamin K supplementation may lead to improved outcomes after kidney transplantation.
Delanaye P, Krzesinski JM, Warling X, Moonen M, Smelten N, Medart L, et al. Dephosphorylated-uncarboxylated Matrix Gla protein concentration is predictive of vitamin K status and is correlated with vascular calcification in a cohort of hemodialysis patients. BMC Nephrol. 2014 Sep 4;15:145.
Matrix Gla protein acts as a potent inhibitor of vascular calcifications, if activated by vitamin K. This study focused on the inactive form of MGP in a population of hemodialyzed (HD) patients, some being treated with a vitamin K antagonist (VKA), like warfarin and some not. 160 patients were enrolled. The study confirmed that patients being treated with VKA had a higher concentration of uncarboxylated MGP (dp-ucMGP), and they found a significant correlation between dp-ucMGP and the calcification score.
Delanaye P, Liabeuf S, Bouqueqneau A, Cavalier E, Massy ZA. The matrix-gla protein awakening may lead to the demise of vascular calcification. Nephrol Ther. 2014 Mar 17; epub ahead of print.
Matrix gla protein (MGP) is secreted mainly by chondrocytes and smooth vascular muscle cells. Like other Gla proteins, it is vitamin K dependent. A link exists between MGP, vitamin K, vascular calcifications and cardiovascular disease. This link is even more evident in patients suffering from chronic kidney diseases and notably, hemodialysis patients. MGP concentrations could allow the monitoring of treatment for these patients with vitamin K. There are trials using this treatment currently ongoing. This review summarizes the role of MGP, and describes the different clinical studies on MGP and vascular calcifications in the general population and in CKD patient.
Mac-Way F., Poulin A., Utescu M.S., De Serres S.A., Marquis K., Douville P., Desmeules S., Larivière R., Lebel M., Agharazii M. The impact of warfarin on the rate of progression of aortic stiffness in hemodialysis patients: A longitudinal study. Nephrol. Dial. Transpl. 2014;29:2113–2120.
An observational study reported that the use of VKAs is related with increased aortic stiffness in end-stage CKD patients undergoing haemodialysis (HD).
Delanaye P, Liabeuf S, Bouguegneau A, Cavalier E, Massy ZA. The matrix-gla protein awakening may lead to the demise of vascular calcification. Nephrol Ther. 2015 Jul;11(4):191-200.
Matrix-gla-protein (MGP) is mainly secreted by chondrocytes and smooth vascular muscle cells, and is a potent inhibitor of vascular calcification, depending on vitamin K availability. This review summarizes the role of MGP in the vascular calcifications process, and the clinical studies on MGP and vascular calcification in the general population and in CKD patients.
Fusaro M, Tripepi G, Noale M, Plebani M, Zaninotto M, Piccoli A, et al. Prevalence of vertebral fractures, vascular calcification,s and mortality in warfarin treated hemodialysis patients. Curr Vasc Pharmacol. 2015;13:248-258.
Warfarin inhibits vitamin-K dependent proteins involved in bone mineralization and the prevention of vascular calcification (bone Gla protein BGP, matrix Gla protein MGP). In this multicenter, cross-sectional study with 3-year follow-up, data from 387 patients on hemodialysis for ≥1 year at 18 dialysis units were analyzed. Patients on warfarin treatment for > 1 year (11.9% of the population) were compared with the remaining cohort for vertebral fractures, vascular calcifications and mortality. In univariate Cox regression analysis, patients on warfarin had a higher risk of all-cause mortality (HR 2.42, 95% CI 1.42-4.16, p=0.001) when compared with those untreated.
Giangola MD, Yang W-L, Rajayer SR, Kuncewitch M, Molmenti E, Nicastro J, et al. Growth arrest-specific Protein 6 protects again renal schemia-reperfusion injury. J Surg Res. 2015 Dec;199(2):572-579.
Gas6 suppresses the NF-κB pathway and promotes cell proliferation, leading to reduction of inflammation and protection of renal injury induced by I/R.
Holden RM, Booth, SL, Day AG, Clase CM, Zimmerman D, Moist L, et al. Inhibiting the progression of arterial calcification with vitamin k in hemodialysis patients (iPACK-HD) trial: Rationale and study design for a randomized trial of vitamin K in patients with end stage kidney disease. Can J Kidney Heal Dis. 2015;2:53.
Hallajzadeh J, Ghorbanihaghjo A, Argani H, Dastmalchi S, Rashtchizadeh N. Growth arrest-specific 6 protein and matrix Gla protein in hemodialysis patients. Iranian J of Kidney Dis. 2015 May;9(3):249-255.
Plasma protein growth arrest-specific 6 (GAS6) and matrix Gla protein (MGP) are crucial mediators of vascular calcification and are involved in the development of vascular complications in chronic kidney diseases. This study investigated the relationship between plasma GAS6 levels and MGP in patients with end-stage renal disease on maintenance hemodialysis. Plasma GAS6 levels were significantly higher in the hemodialysis patients as compared with the control group. Plasma MGP concentration was significantly lower in the hemodialysis patients than the control. The levels of GAS6 were inversely associated with MGP (r = -0.341, P = .02) in the hemodialysis patients. their inverse correlation may suggest that there might be a role in increased calcification process in hemodialysis patients or only as a secondary phenomenon of advanced kidney failure. Their direct role on vascular calcification needs further studies in the future.
Kurnatowska I, Grzelak P, Masajtis-Zagajewska M, Kaczmarska M, Stefarnczyk L, Vermeer C, et al. Effect of vitamin K2 on progression of atherosclerosis and vascular calcification in nondialyzed patients with chronic kidney disease stages 3-5. Pol Arch med Wewn. 2015;125(9):631-640.
In this study 42 patients with CKD were given either 90 ug of vitamin K2 (MK7) together with 10 ug of vitamin D, or 10 ug of vitamin D alone. In the K&D group, they found that the increase of the common carotid intima-media thickness was significantly less, the increase in the calcium score was slightly lower, and there was a significant decrease in the levels of uncarboxylated MGP and total Osteocalcin. They felt that a 270 days course of MK7 and vitamin D may reduce the progress of atherosclerosis.
Piven E, Pruijm M, Ackermann D, Guessous I, Ehret G, Pecher-Bertschi A, et al. ID.03: Inactive matrix gla protein is associated with renal resistive index in a population-based study. J Hypertens. 2015 Jun;33 Suppl1, e15. 10.1097/01.hjh.0000467389.43721.16
Renal Resistive Index assesses renal arterial disease, including renal vascular stiffness and pulse pressure. The Index correlates positively with arteriosclerosis in damaged kidneys and predicts progressive renal dysfunction. Matrix Gla protein is a vascular calcification inhibitor that needs vitamin K to be activated. Matrix Gla protein that is inactive is measured as dephospho-uncarboxylated MGP, dp-ucMGP. This study looked at whether an increased RRI is associated with high levels of inactive MGP. They studied 1035 participants in Switzerland and found that RRI was independently and positively associated with inactive MGP, or high levels of dp-ucMGP. They recommend further studies to determine whether vitamin K supplementation can help with renal vascular stiffness and kidney function.
Wyskida K, Zak-Golab A, Labuzek K, Suchy D, Ficek R, Pospeich K, et al. Daily intake and serum concentration of menaquinone-4 (MK-4) in haemodialysis patients with chronic kidney disease. Clin Biochem. 2015 Dec;48(18):1246-51.
This study assessed daily vitamin K1 and MK4 intakes and their relation to serum MK4 concentrations in hemodialysis patients. They found decreased MK4 concentration, and concluded it was due to diminished meat consumption and reduced K1 conversion.
Zhang M., Ni Z., Zhou W., Qian J. Undercarboxylated osteocalcin as a biomarker of subclinical atherosclerosis in non-dialysis patients with chronic kidney disease. J Biomed Sci. 2015;22:75.
Studies in recent years have shown that undercarboxylated osteocalcin (uOC) not only maintains bone mineralization, but is also involved in the regulation of atherosclerosis. However, a correlation between uOC and carotid atherosclerosis in non-dialysis patients with chronic kidney disease (CKD) has not been investigated. The uOC levels of non-dialysis patients with CKD were significantly lower than those of healthy controls. The uOC levels gradually decreased as CKD progressed (P < 0.01). The uOC levels were significantly lower in patients with carotid plaques than in patients without carotid plaques. They concluded that serum uOC levels in non-dialysis patients with CKD are significantly lower than those in healthy individuals, and uOC is closely associated with subclinical atherosclerosis in CKD patients.
Chen L-W, Chen W, Hu Z-q, Bian J-L, Ying L, Hong g-L, et al. Protective effects of Growth Arrest-Specific Protein 6 (Gas6) on sepsis-induced acute kidney injury. Inflammation. 2016 Apr;39(2):575-82.
This study investigated the effects of Gas6 on sepsis-associated AKI in mice. the administration of rmGas6 significantly reduced serum urea nitrogen and creatinine and improved the survival of septic mice. Furthermore, the renal pathological damage induced by CLP was attenuated by rmGas6 treatment. The data suggest that rmGas6 might be used as a potential therapeutic agent for sepsis-induced AKI.
Epstein, M. Matrix Gla-Protein (MGP) Not Only Inhibits Calcification in Large Arteries but Also May Be Renoprotective: Connecting the Dots. EBioMedicine. 2016;4:16–17.
Go AS. Cardiovascular disease consequences of CKD. Semin Nephrol. 2016;36:293-304.
Chronic kidney disease, affects approximately 13% of adult Americans and is linked to a variety of clinical complications. This review evaluates the current evidence about the clinical and subclinical cardiovascular consequences associated with chronic kidney disease of varying levels of severity. In addition, it discusses the predictors of adverse cardiovascular outcomes while also focusing on recent insights into the relationships between chronic kidney disease and cardiovascular disease from the Chronic Renal Insufficiency Cohort study, a large current prospective cohort study of adults from across the spectrum of chronic kidney disease.
Harshman SG, Shea MK. The role of vitamin K in chronic aging diseases: inflammation, cardiovascular disease, and osteoarthritis. Curr Nutr Rep. 2016;5(2):525-7.
Kurnatowska I, Grzelak P, Masajtis-Zagajewska A, Kaczmarska M, Stefanczyk L, Vermeer C, et al. Plasma Desphospho-Uncarboxylated Matrix Gla Protein as a Marker of Kidney Damage and Cardiovascular Risk in Advanced Stage of Chronic Kidney Disease. Kidney & blood pressure research. 2016;41(3):231–9.
Dp-ucMGP is formed as a result of vitamin K insufficiency. The aim of this study was to investigate the association between blood levels of dp-ucMGP, kidney function and cardiovascular risk factors before and after 9-months substitution of vitamin K2 in non-dialysis patients with chronic kidney disease (CKD) stage 4 and 5. They found that high dp-ucMGP level, reflecting a poor vitamin K status seems to be associated with kidney damage and may be also a marker of cardiovascular risk in CKD patients. Supplementation with vitamin K2 may improve the carboxylation status of MGP.
Mayer Jr. O. Matrix Gla protein as a natural inhibitor of vascular calcification and potential treatment target. Cas Lek Cask. 2016;155(4):13-6.
Recently, it has been shown that vascular calcification is a highly regulated and potentially reversible process. Matrix Gla protein (MGP) is a natural inhibitor of tissue calcification and vitamin K is a key factor in the biotransformation of this protein into its active form. This article summarizes recent findings on MGP and the potential benefit of vitamin K supplementation is discussed.
Schlieper G, Schurgers L, Brandenburg V, Reutelingsperger C, Floege J. Vascular calcification in chronic kidney disease: an update. Nephrol Dial Transplant. 2016;31:31-30.
Nigwekar SU, Bloch DB, Nazarian RM, Vermeers C, Booth SL, Xu D, et al. Vitamin K-dependent carboxylation of matrix Gla protein influences the risk of calciphylasix. J Am Soc Nephrol. 2017 Jun;28(6):1717-1722.
Matrix Gla protein (MGP) is a potent inhibitor of vascular calcification. The ability of MGP to inhibit calcification requires the activity of a vitamin K–dependent enzyme, which mediates MGP carboxylation. They investigated how MGP carboxylation influences the risk of calciphylaxis in adult patients receiving dialysis and examined the effects of vitamin K deficiency on MGP carboxylation. They found that patients with calciphylaxis had reduced relative cMGP concentration and a high prevalence of vitamin K deficiency relative to matched controls.
Wei F, Drummen NEA, Staessen JA. Vitamin-K-dependent protection of the renal microvasculature: Histopathological studies in normal and diseased kidneys. Pulse (Basel). 2016(Sep;4(2-3):85-91.
Vitamin K dependent carboxylation of matrix Gla protein (MGP) protects the macrocirculation against calcification. Vitamin K might have a beneficial effect on the renal microcirculation. In this pilot study, they looked at kidney tissue samples and demonstrated that normal kidneys are devoid of microcalcifications, while MGP was found within the microcalcifications in diseased kidneys. They concluded that active MGP may inhibit calcification in renal tissue. Their findings highlight potentially new avenues for promoting renal health by increasing dietary intake of vitamin K. It also extends the protective role of vitamin K from its importance in circulating throughout the body at large, to the microcirculation in organs such as the kidneys, revealing an untapped potential for prevention by supplementation.
Wuyts J, Dhondt A. The role of vitamin K in vascular calcification of patients with chronic kidney disease. Inter J of Clinical and Laboratory Medicine. 2016;71(6):462-467.
In recent years, new insights have been gained pointing to vitamin K as a main actor in vascular calcification. Vitamin K is an essential cofactor for the activation of matrix Gla protein (MGP), a calcification inhibitor. Patients with chronic kidney disease often suffer from vitamin K deficiency. Vitamin K supplementation and going off warfarin are potential treatments.
Wei F, Drummen N, Schuette AE, Thijs L, Jacobs L, et al. Vitamin K dependent protection of renal function in multi-ethnic population studies. EBioMedicine. 2016 Feb;4:162-69.
This study assessed the association between renal microvascular function with circulating uncarboxylated dep-ucMatrix Gla Protein and t-ucMatrix Gla Protein in a multi-ethnic population. High de-ucMGP was a marker of vitamin K deficiency. They found that microvascular function in the kidneys was inversely associated with the amount of uncarboxylated matrix Gla protein in Flemish, black South Africans and all South Africans combined. They believed that impairments in inhibiting calcification might be a major player underlying the high risk of calcification and death in patients with chronic kidney disease.
Wei FF, Drummen NE, Thijs L, Jacobs L, Herfs M, Van’t Hoofd C, Vermeer C, Staessen JA. Vitamin-K-dependent protection of the renal microvasculature: histopathological studies in normal and diseased kidneys. Pulse (Basel). 2016;4:85–91.
Wyskida K, Zak-Golab A, Wajda J, Klein D, Witkowicz J, Ficek R, et al. Functional deficiency of vitamin K in hemodialysis patients in Upper Silesia in Poland. Int Urol Nephrol. 2016 May;48(5):765-71.
Zaragatski E, Grommes J, Schurgers LJ, Langer S, Kennes L, Tamm M, et al. Vitamin K antagonism aggravates chronic kidney disease-induced neointimal hyperplasia and calcification in arterialized veins: role of vitamin K treatment. Kidney Int. 2016 Mar;89(3):601-611.
This study investigated the effects of vitamin K antagonists and vitamin K2 treatment on neointimal hyperplasia development and calcification in rats and in arterialized human veins. Neointimal hyperplasia is defined as the accumulation of smooth muscle cells and extra cellular matrix in the intima and is the main pathological process that occurs one month to one year after graft implantation in CKD. K2 treatment, additional to vitamin K antagonists, significantly reduced neointimal hyperplasia in arterialized veins in healthy rats but not in rats with CKD. Arterialization, CKD, and vitamin K antagonism all significantly increased, whereas K2 supplementation attenuated calcification in healthy rats and rats with CKD. K2 significantly enhanced matrix Gla protein carboxylation in control rats and rats with CKD. Thus, vitamin K antagonists have detrimental effects on AVF remodeling, whereas K2 reduced neointimal hyperplasia and calcification indicating vasoprotective effects. Vitamin K supplementation could represent a promising therapeutic approach for patients prone to vascular calcification and vascular access failure.
Aoun M, Makki M, Azar H, Matta H, Chelala DN. High dephosphorylated-uncarboxylated mGp in hemodialysis patients: risk factors and response to vitamin K2, a pre-post intervention clinical trial. BMC. Nephrol. 2017 Jun 17;18(1):191.
Vascular calcifications are highly prevalent in hemodialysis patients. Dephosphorylated-uncarboxylated MGP (dp-ucMGP) was found to increase in vitamin K-deficient patients and may be associated with vascular calcificaitons. Supplementation of hemodialysis patients with vitamin K, MK7, has been studied in Europe with a maximum 61% drop of dp-ucMGP levels. This study looked at the drop of dp-ucMGP in an Eastern Mediterranena cohort after vitamin K treatment, and the correlation between baseline and vascular calcification score. The participants took 360 ug of MK7 for 4 weeks. The average drop of dp-ucMGP at 4 weeks of treatment was found to be 86%, meaning their risk for calcification had significantly declined.
Chen Z, Qureshi AR, Parini P, et al. Does statins promote vascular calcification in chronic kidney disease? Eur J Clin Invest. 2017;47:137-148.
They looked at the mortality predictive significance of CAC scores and its links with statins and inflammatory markers. A higher CAC score predicted all-cause mortality. The use of statins were associated with a higher CAD score and a more rapid progression of CAC score.
Cunha PG, Boutouyrie P, Nilsson PM. et al. Early vascular ageing (EVA): definitions and clinical applicability. Curr Hypertens Rev. 2017; 13: 8–15.
Arterial stiffness has been established as an independent risk marker for cardiovascular disease, and reflects the dissociation between chronologic and biologic age of large arteries-attributing earlier the risk that a normal vascular ageing process had installed to occur several years later. The concept of Early Vascular Ageing (EVA) is developed to establish primordial prevention, identifying individuals whose ageing path has been accelerated either by inherent features, interaction with the environment or arterial exposure to several types of insults that evolve to medial layer morphological changes. Understanding the pathophysiology of vascular ageing, its consequences and therapeutic opportunities is therefore an advantage that could be translated in time of prevention and survival free of cardiovascular disease.
Fusaro M, Plebani M, Iervasi G, Gallieni M. Vitamin K deficiency in chronic kidney disease: evidence is building up. Am J Nephrol. 2017;45:1-3.
Mounting evidence suggests that assessing vitamin K status could be potentially important in patients with chronic kidney disease. Uremic status could be an independent risk factor for vitamin K deficiency, with the deranged vitamin K metabolism in CKD as a therapeutic target. Further studies should be implemented, addressing several undefined areas to target the treatment.
Ketteler M, Brandenburg VM. K-alcification protection in dialysis patients: The underestimated phenomenon of vitamin K Deficiency. J Am Soc Nephrol. 2017 Jun;28(6):1667-1668.
Calciphylaxis, or calcific uremic arteriolopathy (CUA), is a rare (orphan) but life-threatening disorder predominantly occurring in patients with end stage CKD and characterized by calcifying cutaneous arterioles and rapidly progressive, very painful skin ulcerations. Estimated 1-year mortality may range between 50% and 80% and is mostly due to superinfections with subsequent sepsis, or cardiovascular events. There was a strong suspicion that vitamin K antagonist (VKA) treatment may be a trigger of this disorder. The solution may be to supplement all patients on dialysis with vitamin K in the future. It appears that promoting adequate vitamin K status through dietary advice, supplementation and avoidance of vitamin K antagonists may become standard treatment.
Lin MC, Streja E, SooHoo M, Hanna M, Savoj J, Kalantar-Zadeh K, et al. Warfarin use and increased mortality in end-stage renal disease. Am J Nephrol. 2017;46:249-256.
Warfarin use was associated with several-fold higher risk of death, bleeding and myocardial infarction in dialysis patients. If additional studies suggest similar associations, use of warfarin in dialysis patients warrants immediate reconsideration.
Mansour AG, Hariri E, Daaboul Y, Korjian S, El Alam A, Protegerou AD, et al. Vitamin K2 supplementation and arterial stiffness among renal transplant patients- a single arm, single-center clinical trial. J Am Soc Hypertens. 2017 Sep;11(9):589-597.
Subclinical vitamin K deficiency is prevalent among renal transplant recipients and is associated with an increased risk of cardiovascular disease. The KING trial (vitamin K2 in renal Graft) is a single-arm study that evaluated the association between the change in vitamin K status and indices of arterial stiffness, following 8 week sof MK7 supplementation, 360 ug once daily, among renal transplant recipients. The results showed that vitamin K supplementation was associated with improvement in subclinical vitamin deficiency and arterial stiffness.
McCabe KM, Booth SL, Fu X, Ward E, Adams MA, Holden RM. Vitamin K metabolism in a rat model of chronic kidney disease. Am J Nephrol. 2017;45:4-13.
Patients with CKD have very high levels of uncarboxylated, inactive, vitamin K-dependent proteins in circulation, which puts them at risk for vitamin K deficiency. In this study, they found that rats with both mild and severe CKD have significantly lower amounts of K1 as measured in the liver, spleen, and heart, and higher levels of MK4 in the kidney, cortex, and medulla. All animals treated with high dietary K! had an increase in tissue levels of both K1 and MK4, however the relative increase in K1 differed, suggesting the conversion of K1 to MK4 may be a regulating process. Their findings suggest that CKD impacts vitamin K metabolism, early in the disease process. They also conclude that taking vitamin K can reduce the risk factor for vascular and bone health in people with CKD.
Neradova A, Schumacher SP, Hubeek I, Lux P, Schurgers LJ, et al. Phosphate binders affect vitamin K concentration by undesired binding, an in vitro study. BMC Nephrology. 2017;18:DOI: 10.1186/s12882-017-0560-3.
Vascular calcification is major contributing factor to mortality in renal disease. This study tested whether phosphate binders could limit bioavailability of vitamin K2 by undesired binding. Creating a deficiency of vitamin K limits the activation of vascular calcification inhibitors, such as matrix Gla protein, thereby exacerbating vascular calcification. They tested five different phosphate binders. It appears that some commonly used phosphate binders may have clinical consequences, by lowering the bioavailability of vitamin and its benefits. Sicpferroc-oxyhydroxide and sevalamer carbonate were the only binders that did not bind vitamin K2 in vitro.
Radulescu D, Stroescu AEB, Pricop C, Geavlete B, Negrei C, Bratu O, et al. Vitamin K Influence on Cardiovascular Mortality in Chronic Hemodialysed Patients. Revista de chimie. 2017;68(1):52–4.
Cardiovascular disease causes increased mortality in chronic hemodialysed patients. The decrease of vascular calcification is one of the main targets in the management of these patients. According to several experimental and clinical trials, choosing the proper diet and prescribing vitamin K2 supplements help to improve prognosis and decrease mortality, but further larger researchers are required to advocate the importance of this dietary intervention in hemodialysed population.
Roumeliotis, S.; Roumeliotis, A.; Panagoutsos, S.; Giannakopoulou, E.; Papanas, N.; Manolopoulos, V.G.; Passadakis, P.; Tavridou, A. Matrix Gla protein T-138C polymorphism is associated with carotid intima media thickness and predicts mortality in patients with diabetic nephropathy. J. Diabetes Complicat. 2017;31:527–1532.
Stenvinkel P, Luttropp K, McGuinness D, Witasp A, Qureshi AR, Wernerson A, et al. G.CDKN2A/p16INK4(alpha) expression is associated with vascular progeria in chronic kidney disease. AGING-US. 2017;9(2):494–507.
Clinically, decreasing vascular calcification in chronic hemodialysed patients suffering from cardiovascular diseases helps decrease mortality. It has been suggested by a number of experimental and clinical trials, that vitamin K supplementations and a proper diet helps decrease mortality and improve prognosis. This study found that impaired vitamin K carboxylation may contribute to premature vascular difficulties in CKD.
Thamratnopkoon S, Susantitaphong P, Tumkosit M, Katavetin P, Tiranthanaqul K, Praditpornsilpa K, et al. Correlations of plasma dephosphorylated uncarboxylated matrix Gla protein with vascular calcification and vascular stiffness in chronic kidney disease. Nephron. 2017;135(3):167-172.
Matrix Gla protein is a potent inhibitor of vascular calcification and needs vitamin K-dependent carboxylation for its activity. This study explored correlations between blood levels of dp-ucMGP (desphosphorylated uncarboxylated MGP) and vascular calcification and vascular stiffness in patients with chronic kidney disease. They found that blood levels of dp-ucMGP increase according to the severity of chronic kidney disease, indicating that they had a vitamin K deficiency.
Wei FF, Thijs L, Zhang ZY et al. The risk of nephrolithiasis is causally related to inactive matrix Gla protein, a marker of vitamin K status: a Mendelian randomization study in a Flemish population. Nephrol Dial Transplant. 2017;doi 10.1093/ndt/gjx014
Nephrolithiasis represents a process of unwanted calcification associated with substantial mortality and high recurrence rates. This study hypothesized that the risk of nephrolithiasis increases with VK shortage. They studied 1748 randomly recruited Flemish individuals, and followed them for almost nine years. They found that higher levels of inactive dp-ucMGP may be causally associated with the risk of nephrolithiasis. More research should study whether vitamin K deficiency plays a role in these observations.
Wei FF, Trenson S, Thijs L, Huang QF, Zhang ZY, Yang WY, et al. Desphosopho-uncarboxylated matrix Gla protein is a novel circulating biomarker predicting deterioration of renal function in the general population. Nephrol Dial Transplant. 2017:1-7.
Research supports that matrix Gla protein is renoprotective (or helps with renal functioning) due to vitamin K-dependent activation. Over 1000 Flemish women were studied for a median of 8.9 years. They found that circulating inactive dp-ucMGP (desphosopho-uncarboxylated matrix Gla protein), a biomarker of poor vitamin K status, predicts renal dysfunction.
Cozzolino M, Mangano M, Stucchi A, Ciceri P, Conte F, et al. Cardiovascular disease in dialysis patients. Nephrol Dial Transpl. 2018;33:ii28-ii34.
Cardiovascular disease (CVD) is a highly common complication and the first cause of death in patients with end-stage renal disease (ESRD) on haemodialysis (HD). In this population, mortality due to CVD is 20 times higher than in the general population and the majority of maintenance HD patients have CVD. This is likely due to ventricular hypertrophy as well as non-traditional risk factors, such as chronic volume overload, anaemia, inflammation, oxidative stress, chronic kidney disease–mineral bone disorder and other aspects of the ‘uraemic milieu’.
Cui L, Xu J, Zhang J, Zhang M, Zhang S, Bai Y. Menaquinone-4 modulates the expression levels of calcification-associated factors to inhibit calcification of rat aortic vascular smooth muscle cells in a dose-dependent manner. Exp Ther Med. 2018 Oct;16(4):3172-78.
Studies have demonstrated that menaquinone 4 is negatively associated with vascular calcifications in patients with chronic kidney disease. This study found that MK4 reduces mineralization by regulating the bone morphogenetic protein (BMP-2) pathway. Calcium deposition in the cells could be completely prevented by co-incubation with MK4 in a dose dependent manner.
Dihingia A, Ozah D, Baruah PK, et al. Prophylactic role of vitamin K supplementation on vascular inflammation in type 2 diabetes by regulating the NF-κB/Nrf2 pathway via activating Gla proteins. Food Funct. 2018; 9: 450–462.
Franceschi C, Garagnani P, Parini P, et al. Inflammaging: a new immune–metabolic viewpoint for age-related diseases. Nat Rev Endocrinol. 2018; 14: 576–590.
Hou Y-C, Lu C-L, Zheng C-M, Chen R-M, Lin Y-F, Liu W-C, et al. Emerging role of vitamins D and K in modulating uremic vascular calcification: The aspect of passive calcification. Nutrients. 2019;11:152.
Vitamin K governs the gamma-carboxylation of matrix Gla protein for inhibiting vascular calcification, and the Vitamin D binding protein receptor is related to vitamin K gene expression. Matrix vesicles and calciprotein particles (CPP) have gained attention in CKD. Vitamin D supplementation may be a possible therapeutic target along with vitamin K for alleviating uremic vascular calcification.
Jansz TT, Neradova A, van Ballegooijen AJ, Verhaar MC, Vervloet MG, et al. The role of kidney transplantation and phosphate binder use in vitamin K status. PLosS One. 2018;13(8):e-2-3157.
This study measured the blood levels of dp-ucMGP (uncarboxylated matrix Gla protein), a marker reflecting low vitamin K status in a cross-sectional study of patients on hemodialysis, peritoneal dialysis, or who recently received a kidney transplant. Patients on dialysis are routinely prescribed phosphate binders to lower serum phosphate levels, despite there being no evidence of benefit and some indication of adverse effects. (Phosphate binders can worsen vitamin K status and promote vascular calcification). They found that kidney transplant recipients have substantially lower dp-ucMGP levels compared to patients on any form of dialysis, indicating better vitamin K status. They also found a negative effect of binders on vitamin K status. Their findings warrant more attention to vitamin K status in patients on dialysis, or even vitamin K supplementation.
Miyata KN, Nast CC, Dai T, Dukkipati R, LaPage JA, Troost JP. Renal matrix Gla protein expression increases progressively with CKD and predicts renal outcome. Exp. Mol. Pathol. 2018;105:120–129.
Puzantian H, Akers SR, Oldland G, Javaid K, Miller R, Ge Y, Ansari B, Lee J, Suri A, Hasmath Z, Townsend R, Chirinos JA. Circulating dephospho-uncarboxylated matrix Gla-protein is associated with kidney dysfunction and arterial stiffness. Am J Hypertens. 2018;31:988–994.
Large artery stiffening is increased in advanced chronic kidney disease (CKD) but likely develops progressively in earlier stages of CKD. Active matrix Gla-protein (MGP) is a potent vitamin K-dependent inhibitor of vascular calcification. This study showed that CKD is associated with increased (inactive) dp-ucMGP, a vitamin K-dependent inhibitor of vascular calcification, which correlates with large artery stiffness. Further studies are needed to assess whether vitamin K2 supplementation represents a suitable therapeutic strategy to prevent or reduce arterial stiffening in CKD.
Turner ME, Adams MA, Holden RM. The vitamin K metabolome in chronic kidney disease. Nutrients. 2018 Aug 12;10(8):1076.
Vitamin K-dependent probeins contribute to cardiovascular disease prevention via the prevention of ectopic mineralization. Sub-clinical vitamin K deficiency is common in CKD patients which contributes to the CVD burden in this population.It appears that CKD alters tissue measures of MK4 and K1. And the expression and/or activity of enzymes that regulate the recycling of vitamin and the carboxylation of vitamin K-dependen tproteins also appear to be altered in CKD. Statins interfere with the metabolism of vitamin K for CKD patients.
Viegas CSB, Santos L, Macedo AL, Matos AA, Silva AP, Neves PL, et al. Chronic kidney disease circulating calciprotein particles and extracellular vesicles promote vascular calcification: A role for GRP (Gla-Rich Protein). Arterioscler Thromb Vasc Biol. 2018 Mar;38(3):575-587.
Inhibition of mineral crystal formation is a crucial step in ectopic calcification. This study looked at the association of vitamin K dependent protein GRP with circulating calciprotein particles and extracellular vesicles. They found that carboxylated GRP was an inhibitory factor to prevent calcification at both systemic and tissue levels.
Wei FF, Thijs L, Zhang ZY, et al. The risk of nephrolithiasis is causally related to inactive matrix Gla protein, a marker of vitamin K status: a Mendelian randomization study in a Flemish population. Nephrol Dial Transplant. 2018;33:514–522.
Nephrolithiasis represents a process of unwanted calcification associated with substantial mortality and high recurrence rates. We hypothesized that the risk of nephrolithiasis increases with VK shortage, as exemplified by higher plasma levels of desphospho-uncarboxylated MGP (dp-ucMGP). In 1748 randomly recruited Flemish individuals (51.1% women; mean age 46.8 years), we determined dp-ucMGP and the prevalence of nephrolithiasis. We found that higher levels of inactive dp-ucMGP may be causally associated with the risk of nephrolithiasis. Whether or not VK deficiency plays a role in these observations remains to be firmly established.
Wei FF, Trenson S, Thijs L, Huang QF, Zhang ZY, Yang WY, Moliterno P, Allegaert K, Boggia J, Janssens S, Verhamme P, Vermeer C, Staessen JA. Desphospho-uncarboxylated matrix Gla protein is a novel circulating biomarker predicting deterioration of renal function in the general population. Nephrol Dial Transplant. 2018;33:1122–1128.
Willems BA, Furmanik M, Caron MMJ, Chatrou MLL, Kusters DHM, Welting TJM, et al. Ucma/GRP inhibits phosphate-induced vascular smooth muscle cell calcification via SMAD-dependent BMP signaling. Scientific Reports. 2018;8:ISSN 2045-2322.
Vascular calcification is the process of deposition of calcium phosphate crystals in the blood vessel wall, and is highly prevalent in chronic kidney disease. Calcification is in part regulated by vascular smooth muscle cells (VSMCs). This study shows that Ucma/GRP is present in calcified atherosclerotic plaques and highly expressed in vascular smooth muscle cells. Their results showed evidence for an important role of Ucma/GRP in regulating osteo/chondrogenic differentiation and phosphate-induced mineralization in the VSMCs.
Yamada H., Kuro-O. M., Ishikawa S.-E., Funazaki S., Kusaka I., Kakei M., Hara K. Daily variability in serum levels of calciprotein particles and their association with mineral metabolism parameters: A cross-sectional pilot study. Nephrology (Carlton). 2018;23:226–230.
Cozzolino M, Ciceri P, Galassi A, Mangano M, Carugo S, Capelli I, et al. The key role of phosphate on vascular calcification. Toxins. 2019;11:213.
Cozzolino M, Fusaro M, Ciceri P, Gasperoni L, Cianciolo G. The role of vitamin K in vascular calcification. Adv Chronic Kidney Dis. 2019;26:437-444.
This review analyzes the pathophysiological mechanisms and clinical consequences of vitamin K deficiency with emphasis on its involvement on vascular calcification in CKD and end-stage renal disease and its relationship to the bone-vascular axis.
Cozzolino M, Mangano M, Galassi A, Ciceri P, Messa P, Nigwekar S. Vitamin K in chronic kidney disease. Nutrients. 2019 Jan 14;11(1).
Accumulating evidence demonstrates that chronic kidney disease patients suffer from subclinical vitamin K deficiency. This deficiency might be caused by exhaustion of vitamin K due to its high requirements by vitamin K-dependent proteins used to inhibit calcification.
Evenepoel P, Claes K, Meijers B, Laurent M, Bammens B, et al. Poor vitamin K status is associated with low bone mineral density and increased fracture risk in end-stage renal disease. J Bone Min Res. 2019;34:262-69.
Patients with chronic kidney disease (CKD) suffer an excessively high fracture risk. This study hypothesizes that vitamin K insufficiency may be a risk factor for folks with CKD. Vitamin K plays an important role in maintaining bone health. This study tested the hypothesis that vitamin K insufficiency confers an increased fracture risk in patients with early stage renal disease. They found a significant and direct association between vitamin K status and aBMD (areal Bone Mineral Density) at the central skeleton. They concluded that poor vitamin K status is highly prevalent among patients with ESRD and associates with inflammation and low aBMD. Poor vitamin K status at the time of renal transplant can be considered a risk factor for fractures.
Fusaro M, Aghi A, Khairallah P, Gallieni M, Cozzolino MG, Russo D, et al. Sevelamer use is associated with decreased vitamin K levels in hemodialysis patients: results from the Vitamin K Italian (VIK1) study. J Am Soc Nephrol. 2019;30:471.
In this analysis of the Vitamin K Italian (VIKI) study, the relationship between vitamin K status, vertebral fractures (VFs) and VCs in 387 hemodialysis (HD) patients with (N = 163; 42.1%) or without N = 224; 57.9%) sevelamer was evaluated. Levels of vitamin K vitamers K1 and K2 or menaquinones (MK; MK4–7), total and undercarboxylated (uc) forms for both BGP and MGP were determined. Although no differences in clinical characteristics were noted, lower levels of MK4 (0.45 versus 0.6 ng/mL, p = .01) and a greater MK4 deficiency was observed in sevelamer-treated patients (13.5% versus 5.4%, p = .005). Sevelamer may interfere with MK4 levels in HD patients and interact with low BGP levels to increase bone fractures in CKD patients
Fusaro M, Khairallah P, Aghi A, Plebani M, Zaninotto M, Cosma C, et al. Vitamin K-dependent proteins after kidney transplantation: results from a prospective study. J Am Soc Nephrol. 2019;30:477.
Two Vitamin K-dependent proteins (VDKPs) link bone and vasculature in CKD-MBD: Bone Gla Protein (BGP) and Matrix Gla Protein (MGP). In ESKD, Vitamin K deficiency is highly prevalent and leads to increased levels of inactive VKDPs (undercaboxylated (ucBGP and dephosphorylated (dp)-uMGP), which are linked to greater risk of fractures and severity of vascular calcification. We hypothesized that kidney transplantation (KT) would improve Vitamin K status and lower levels of inactive VKDPs. Conclusion KT was associated with improvement in Vitamin K status as manifested by decreased levels of inactive VKDPs. These are the first prospective data on VKDPs in CKD patients pre- and post-KT.
Jaques D, Pivin D, Pruijm M, Ackermann D, Guessous I, Ehret G, et al. Renal Resistive Index Is Associated with Inactive Matrix Gla (γ-Carboxyglutamate) Protein in an Adult Population-Based Study. J. Am. Heart Assoc.. 2018;8:e013558.
Lee SM, An WS. Supplementary nutrients for prevention of vascular calcification in patients with chronic kidney disease. Korean J Intern Med. 2019 May;34(3):459-469.
Vascular calcification (VC) and malnutrition associated with cardiovascular disease are common in patients with chronic kidney disease (CKD) treated with dialysis. VC, which reflects vascular aging, and malnutrition are also encountered in the non-CKD elderly population. This similarity of clinical findings suggests that the progression of CKD is related to aging and the existence of a causal relationship between VC and malnutrition. Menaquinone-7, a type of vitamin K2, is under investigation for inhibiting VC in elderly patients without CKD, as well as for prevention of VC in patients with CKD. This review focuses on the ability of supplementary nutrients to prevent VC in patients with CKD, in whom dietary restriction is essential.
Lees JS, Chapman FA, Whitham MD, Jardine AG, Mark PB. Vitamin K status, supplementation and vascular disease: a systematic review and meta-analysis. Heart. 2019 Jun:105(12):938-945.
Vitamin K dependent proteins are associated with vascular stiffness and vascular calcification and require vitamin K for activity. This systemic review and meta-analysis showed that supplementation with vitamin K significantly reduced calcification, when compared with controls. In their review of 13 controlled clinical studies and 14 longitudinal trial sin 12, 888 patients, they found that compared to control, vitamin K supplementation was associated with a 9.1% reduction in VC status, accompanied by a 44.7% decrease in dp-ucMGP levels.
Li Y, Lu X, Yang B, Mao J, Jiang S, Yu D, et al. Vitamin K1 inhibition of renal crystal formation through matrix Gla protein in the kidney. Kidney and Blood Pressure Res. 2019;44(6):
Vitamin K (VK) plays a major role in modifying the binding of calcium in bones and blood vessels. Understanding the effect of VK on crystal formation in the kidney would contribute to advancing the treatment and prevention of kidney stones. Rats were treated with vitamin K1 (VK1) for 8 weeks. VK1 levels were detected and crystal formation were observed. The concentrations of VK1 in whole blood and kidney tissues rose under treatment with VK1. Crystal formation was inhibited from the second to the 6th week, the frequency and quality of crystal formation decreased significantly, and the location of crystal formation was limited to a greater extent in the rats treated by VK1 compared to the control group. Warfarin treatment in the crystals-exposed HK2 cells significantly increased the number of crystals adhering to cells and the number of apoptotic cells and reduced cell viability. VK1 treatment reversed warfarin’s above influence. They found that VK1 treatment can inhibit the formation of renal crystals in vivo. VK1 increases MGP expression and functions through MGP to reduce crystal deposition in cells and provide cell protection. The findings suggest that vitamin K treatment could be a potential strategy for the treatment and prevention of kidney stones.
Mizuiri S, Nishizawa Y, Yamashita K, et al. Relationship of matrix Gla protein and vitamin K with vascular calcification in hemodialysis patients. Ren Fail. 2019;41:770–7.
This study evaluated associations of serum matrix Gla protein (MGP), plasma vitamin K1, and plasma vitamin K2 with coronary artery calcium score (CACS) and cardiovascular disease (CVD) in maintenance hemodialysis (MHD) patients. They found that the end-stage renal disease on hemodialysis is a deficiency state of vitamin K. Total MGP was significantly higher in maintenance dialysis patients compared to healthy subjects and total MGP was associated with the presence of CVD in MHD patients.
Silaghi CN, Ilyes T, Filip VP, Farcas M, van Ballegooijen AJ, Craciun AM. Vitamin K dependent proteins in kidney disease. Int J Mol Sci. 2019;20:1571.
Mounting evidence shows that vitamin K dependent proteins are useful tools to improve early diagnosis, monitor progression or identify complications of CKD.
Caluwé R, Verbeke F, De Vriese AS. Evaluation of vitamin K status and rationale for vitamin K supplementation in dialysis patients. Nephrol Dial Transplant. 2020 Jan 1;35(1):23-33.
Functional vitamin K deficiency is common and severe among dialysis patients and has garnered attention as a modifiable risk factor in this population. However, no single biochemical parameter can adequately assess vitamin K status. The etiology of vitamin K deficiency in hemodialysis is multifactorial, including deficient intake, uremic inhibition of the vitamin K cycle and possibly interference of vitamin K absorption by phosphate binders. The hope is to determine the optimal vitamin K species, dose and duration of supplementation for dialysis patients.
Cozzolino M, Cianciolo G, Podesta MA, Ciceri P, Galassi A, Gasperoni L, et al. Current therapy in CKD patients can affect vitamin K status. Nutrients. 2020 May 30;12(6):1609.
A growing body of evidence shows that CKD patients can be affected by subclinical vitamin K deficiency, which could be a potential therapeutic target (take vitamin K and improve CKD health). It appears that vitamin K deficiency is a common pathogenetic link between impaired bone mineralization and vascular calcification, the latter which is a high risk for folks with CKD.
Dai L, Schurgers, LJ, Shiels PG, Stenvinkel P. Early vascular ageing in chronic kidney disease: impact of inflammation, vitamin K, senescence and genomic damage. Nephrol Dial Transplant. 2020 mar 1;35(Suppl 2):ii31-ii37.
Chronic kidney disease (CKD) is a clinical model of premature ageing characterized by cardiovascular disease, persistent uraemic inflammation, osteoporosis muscle wasting and frailty. The accelerated early vascular ageing (EVA) process mediated by medial vascular calcification (VC) is a hallmark of senescence as well as a strong predictor of cardiovascular morbidity and mortality in the CKD population. Knowledge of the fundamental mechanism underlying EVA is urgently needed to identify and develop novel and efficient therapeutic targets for VC and EVA. Growing evidence shows that nuclear factor erythroid 2-related factor 2 (NRF2) signalling and vitamin K play a crucial role in counteracting oxidative stress, DNA damage, senescence and inflammaging, whereby NRF2 activation and vitamin K supplementation may provide a novel treatment target for EVA. In this review we discuss the link between senescence and EVA in the context of CKD, with a focus on the role of NRF2 and vitamin K in DNA damage signalling, senescence and inflammaging.
de Oliveira RB, Stinghen AEM, Massy ZA. Vitamin K role in mineral and bone disorder of chronic kidney disease. Clin Chim Acta. 2020;502:66-72.
Here, we review the literature data concerning the impact of vitamin K deficiency and supplementation on CKD-associated mineral and bone disorders (CKD-MBD). We present and discuss the available evidence from basic science and clinical studies, and highlight perspectives for further research.
Ebert T, Pawelzik S-C, Witasp A, Arefin S, Hobson S, Kublickiene K et al. Inflammation and premature ageing in chronic kidney disease. Toxins. 2020 Apr;12(4).
Fusaro M, Aghi A, Khairallah P, Gallieni M, Cozzolino MG, Russo D, et al. Sevelamer use is associated with decreased vitamin K levels in hemodialysis patients: results from vitamin K Italian (VIKI) study. Nephrol Dialy Transplant. 2020;35(3):gfaa142.P1485.
The study found that Sevelamer interfered with the absorption of MK4 in patients on hemodialysis. Longitudinal interventional studies are needed to prove the causal nature of the associations.
Fusaro M, Cosmai L, Evenepoel P, Nickolas TL, Cheung AM, Aghi A, et al. Vitamin K and kidney transplantation. Nutrients. 2020;12:2717.
Vitamin K should be explored as a new therapeutic approach with kidney transplant subjects.
Fusaro M, Gallieni M, Porta C, et al. Vitamin K effects in human health: new insights beyond bone and cardiovascular health. J Nephrol. 2020;33:239–49.
Vitamin K dependent-proteins (VKDPs) have important roles in bone health, vascular health, metabolism, reproduction as well as in cancer progression. Vitamin K deficiency is common in different conditions, including kidney disease, and it may influence the activity of VKDPs. This review discusses vitamin K status in human health and the physiologic and pathologic roles of VKDPs, beyond the established effects in skeletal and cardiovascular health.
Haroon SW, Tai BC, Ling LH et al. Treatment to reduce vascular calcification in hemodialysis patients using vitamin K (Trevasc-HDK): a study protocol for a randomized controlled trial. Medicine (Baltimore). 2020;99(36):e21906.
End stage renal failure patients on hemodialysis have significant vascular calcification This is postulated to be related to sub-clinical vitamin K deficiency, which is prevalent in hemodialysis patients. Vitamin K deficiency result in the failure of the matrix GLA protein (MGP) to undergo carboxylation. MGP is a natural local inhibitor of vascular calcification and the lack of functional carboxylated MGP may contribute to increase vascular calcification. Vitamin K supplement should therefore correct this anomaly and decrease the rate or severity of vascular calcification in this population of patients on long-term maintenance hemodialysis. This study seeks to evaluate the prevalence and the progression of vascular calcification in a cohort of maintenance hemodialysis patients. It will also evaluate the efficacy of vitamin K supplementation in reducing the progression of vascular calcification in this group of patients.
Jaminon MG, Dai L, Qureshi AR, Evenepoel P, Ripsweden J, Soderberg M, Witasp A, et al. Matrix Gla protein is an independent predictor of both intimal and medial vascular calcification in chronic kidney disease. Sci. Rep. 2020;10:6586.
Matrix Gla protein (MGP) is a potent inhibitor of vascular calcification (VC) and requires carboxylation by vitamin K to exert calcification inhibition. Chronic kidney disease (CKD) patients undergo early vascular aging often involving extensive calcification. The present cross-sectional study investigated the association between circulating dp-ucMGP levels, MGP expression in vascular tissue and MGP polymorphisms in 141 CKD stage 5 patients, The results indicate that plasma levels of dp-ucMGP are an independent predictor of increased VC in CKD5 patients and correlate with both higher CAC scores and degree of medial calcification. Taken together, our results support that MGP is involved in the pathogenesis of VC.
Mosa MFI, Harfoosh AK. Role of vitamin K therapy in prevention of vascular calcification in chronic kidney disease. EJMED. 2020;2:360.
Randomized study performed to estimate the effect of VK1 supplementation (10 mg after each hemodialysis for 1 year) on vascular calcification as well as to evaluate its impact on MGP in hemodialysis patients. After one year of supplementation the authors found a significant increase in MGP levels, however without any significant changes in carotid intimal medial thickness (CIMT) and abdominal aorta calcification score (AACS) compared to baseline levels. On the other hand, the CIMT and AACS significantly increased in the control group (no supplementation). The authors concluded that VK supplementation could not stop VC, but significantly attenuated their progression.
Silva AP, Viegas CS, Mendes F, Macedo A, Guilherme P, Tavares N, et al. Gla-rich protein (GRP) as an early and ovel marker of vascular calcification and kidney dysfunction in diabetic patients with CKD: A pilot cross-sectional study. J Clin Med. 2020;9:635.
Stępień A, Koziarska-Rościszewska M, Rysz J, Stępień M. Biological role of vitamin K-with particular emphasis on cardiovascular and renal aspects. Nutrients. 2020;14:262.
Vascular calcification is one of the most important mechanisms of renal pathology. The most potent inhibitor is Matrix Gla Protein, which is vitamin K dependent. Chronic kidney disease patients, both dialyzed and non-dialysed often have vitamin K deficiency, which is associated with a higher risk of cardiovascular events in these patients. It has been suggested that K intake may reduce the risk. The role and possibility of K supplementation as well as the impact of vitamin K antagonists which create K deficiency in CKD patients is discussed.
Van Ballegooijen AJ, Beulens JWJ, Keyzer CA, Navis GJ, Berger SP, De Borst MH, et al. Join association of vitamins D and K status with long-term outcomes in stable kidney transplant recipients. Nephrol Dial Transplant. 2020;35:706-714.
Kidney transplant recipients (KTR) continue to have a high mortality and graft failure risk. They are often low in micronutrient status, including vitamins D and K. This study looked at those vitamins and vitamin D treatment as associated with graft failure and mortality, following a transplant. They found that the combined low vitamin D and K status was associated with an increased risk of premature death and graft failure. Importantly, a low vitamin K status with active vitamin D treatment increased the risk. They believe the vitamin D treatment increased the pool of uncarboxylated vitamin K dependent proteins, creating a shorting of active vitamin K and reducing the protection from calcification that vitamin K provides.
Wikström SL, Lentz KA, Hansen D, Rasmussen LM, Jakobsen J, Hansen HP, et al. Causes of vitamin K deficiency in patients on haemodialysis. 2020 Sep;12(9):2513.
The purpose of this study was to investigate possible underlying causes of low vitamin K status, which could potentially be low intake, washout during dialysis or inhibited absorption capacity. Moreover, the aim was to investigate whether the biomarker dp-ucMGP is affected in these patients. All patients had vitamin K deficiency. The reason for the low vitamin K status is not due to removal of vitamin K during dialysis or decreased absorption but is plausibly due to a low intake of vitamin K in food. dp-ucMGP concentrations were measured in plasma before and after haemodialysis treatment. dp-ucMGP concentrations were significantly lower after dialysis treatment. Moreover, dp-ucMGP concentrations were measured in dialysate. These results show that dp-ucMGP were present in dialysate in approximately the same concentrations at the beginning and the end of haemodialysis treatment, meaning it was not filtered out.
Dai L, Li L, Erlandsson H, Jaminon AMG, Qureshi AR, Ripsweden J, et al. Functional vitamin K insufficiency, vascular calcification and mortality in advanced chronic kidney disease: a cohort Study. PLoS One. 2021;16(2):e0247623.
Functional vitamin K deficiency as measured by dp-ucMGP, was associated with increased mortality risk, that is independent of the presence of vascular calcification in patients with CKDG5.
Fusaro M, Tondolo F, Gasperoni L, Tripepi G, Plebani M, Zaninotto M, Nickolas TL, Ketteler M, Aghi A, Politi C, et al. The role of vitamin K in CKD-MBD. Curr Osteoporos Rep. 2022;20:65–77.
We describe the mechanism of action of vitamin K, and its implication in cardiovascular disease, bone fractures, and inflammation to underline its protective role, especially in chronic kidney disease (CKD).
Groothof D, Post A, Sotomayor CG, Keyzer CA, Flores-Guerero JL, Hak E, Bos JH, Schurgers LJ. Navis GJ, Gans RO, et al. Functional vitamin K status and risk of incident chronic kidney disease and microalbuminuria: A prospective general population-based cohort study. Nephrol Dial Transplant. 2021;36:2290–2299.
Circulating desphospho-uncarboxylated matrix γ-carboxyglutamate (Gla) protein (dp-ucMGP), a marker of vitamin K status, is associated with renal function and may serve as a potentially modifiable risk factor for incident chronic kidney disease (CKD).
Sevinc C, Yilmaz G, Ustundag S. The relationship between calcification inhibitor levels in chronic kidney disease and the development of atherosclerosis. Renal Failure. 2021;43(1):1349-1358.
Atherosclerosis or cardiovascular disease is the most important cause of increased mortality in CIKD. They compared healthy individuals and CKD patients for their carotid intima-media thickness, measuring the carotid artery and monitored several calcification inhibitors such as Fetuin-A, matrix Gla protein, and osteoprotegerin. They found that Fetuin-A levels begin to decline from the early stages of CKS and are significantly lower in patients with atherosclerosis in the carotid artery.
Bellone F, Cinquegrani M, Nicotera R, Carullo N, Casarella A, Presta P, et al. Role of vitamin K in chronic kidney disease: a focus on bone and cardiovascular health. Int J Mol Sci. 2022 May;23(9):5282.
Poor vitamin K status seems to have a key role in the progression of CKD, but also in the onset and advance of both bone and cardiovascular complications. This review focuses on the biochemical and functional characteristics of vitamin K vitamers, suggesting this nutrient as a possible marker of kidney, CV, and bone damage in the CKD population and exploring its potential use for promoting health in this clinical setting. Treatment strategies for CKD-associated osteoporosis and CV disease should include vitamin K supplementation.
Fusaro M, Cianciolo G, Evenepoel P, Schurgers L, Plebani M. Vitamin K in CKD bone Disorders. Calcif. Tissue Int. 2021;108:476–485.
It has been highlighted that the uremic state is a condition of greater vitamin K deficiency than the general population with resulting higher prevalence of bone fractures, vascular calcifications and mortality. The purpose of this literature review is to evaluate the protective role of Vitamin K in bone health in CKD patients
Fusaro M, Tondolo F, Gasperoni L, Tripepi G, Plebani M, Zaninotto M, et al. The role of vitamin K in CKD-MBD. Current Osteopor. Reports. 2022;20:65-77.
CKD patients are characterized by lower levels of vitamin K than the general populations, with a resulting higher prevalence of bone fractures, vascular calcifications, and mortality. This review describes the action of vitamin K and its role in disease, especially in chronic kidney disease. CKD patients are characterized by lower levels of vitamin K than the general population, with a resulting higher prevalence of bone fractures, vascular calcification, and mortality. The dose of vitamin K is an important issue and that could improve the health of CKD patients.
Ren S-C, Mao N, Yi S, Ma X, Zou J-Q. Vascular calcification in chronic kidney disease: an update and perspective. Aging Dis. 2022 Jun;13(30:673-697.
Vascular calcification, an ectopic deposition of calcium-phosphate salts in blood vessel walls and heart valves, is an independent risk factor of cardiovascular morbidity and mortality in chronic kidney disease. In this systematic review, we aimed to overview the underlying mechanisms of vascular calcification in chronic kidney diseases and discuss the impact of chronic kidney disease on vascular calcification. Additionally, we summarized potential clinical diagnostic biomarkers and therapeutic applications for vascular calcification with chronic kidney disease. This review may offer new insights into the pathogenesis, diagnosis, and therapeutic intervention of vascular calcification.
Roumeliotis S, Duni A, Vaios V, Kitsos A. Liakopoulos V, Dounousi E. Vitamin K supplementation for prevention of vascular calcification in chronic kidney disease patients: are we there yet? Nutrients. 2022;14:925.
Roumeliotis S, Liakopoulos V, Schurgers LJ. Vitamin K supplementation in chronic kidney disease patients: where is the evidence? Curr Vasc Pharmacol. 2022;20(2):121-126.
Accumulating epidemiological data have associated vitamin K depletion with vascular calcification progression. CKD patients are characterized by poor vitamin K status and at the same time, pronounced calcification. In early and advanced CKD, including end-stage kidney disease, exogenous supplementation of vitamin K (especially with menaquinone 7, its most bioavailable form) might decrease the inactive form of MGP (dephosphorylated, uncarboxylated MGP) and probably retard the progression or even reverse VC. Here, we focus and discuss the interventional human studies of vitamin K supplementation in CKD patients and suggest future directions in this area of interest.
Written by RPT 7/1/13
"In life, in any given situation, one can either be a winner, a loser, or a victim.
If you keep your nose clean, work hard, work smart, and pay attention,
you will win far more than you lose - - - but every now and then you will
lose - - - no worries - - - but what is unacceptable is being a victim.
I chose not be a victim.” - Pat
Click here to read his story
Koncentrated K
USA
Phone: (715) 612-5858
Copyright © 2024 Koncentrated K, web content in part or in whole may not be used without written consent. All rights reserved.