Vitamin K and Diabetes
Diabetes and Vitamin K - - - We are not going to “Sugar Coat” the facts
Bone health is key to diabetes
- Vitamin K reduces the risk of developing diabetes.
- Diabetes affects at least 285 million people worldwide.
- Recent research indicates that bone functions as an endocrine organ, regulating energy metabolism.
- Osteocalcin, a bone protein, is one of the messengers between bone and the pancreas.
- Osteocalcin needs adequate amounts of vitamin K to be carboxylated and active.
- Carboxylated osteocalcin is required for the bone and pancreas to work in coordination.
- Insufficient vitamin K leads to insufficient carboxylated osteocalcin, which interferes with energy and glucose metabolism.
Proteins that depend on vitamin K to be functional and activated are of great interest. Osteocalcin is a vitamin K dependent protein. This page will review the story of osteocalcin and diabetes, detailing the story of how the bone protein osteocalcin became identified as a key regulator of energy and glucose in the body, and the growing body of research indicating that supplementation with vitamin K can delay, prevent, and/or mitigate the disease of diabetes. This is an exciting story that is still being written, but we think it is important to begin.
On this page, we will offer a brief description of diabetes, the discovery of bone as an endocrine organ, the relationship of bone to diabetes, the research linking osteocalcin levels to diabetes, and the critical importance of vitamin K to activate osteocalcin, improving the status of diabetes.
Diabetes
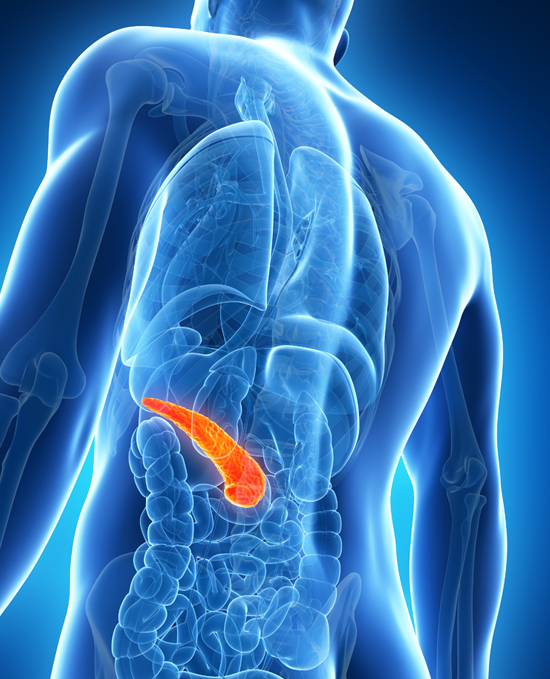
Endocrinology is the study of the various hormones in the body, and the glands or organs that make those hormones (like adrenals, thyroid, pituitary, and the like). Hormones are chemical messages, which travel in the blood throughout the body to elicit a particular response. Diabetes is the most common endocrine (meaning hormone based) disease, and insulin is the hormone which affects the pancreas and the body’s ability to metabolize and generate energy.
Metabolism refers to the way our bodies use digested food for energy and growth. Most of what we eat is broken down into glucose, which is a form of sugar in the blood and is the principal source of fuel for our bodies. As we eat, our pancreas releases the hormone insulin, which serves as a key to opening our cells so the glucose can enter. Without insulin present, glucose cannot enter the cells. With diabetes, the pancreas does not secrete or produce enough insulin, and blood sugar or glucose builds up in the blood stream. It significantly alters energy metabolism, or how the body accesses glucose/sugars that fuel the body. OBTW, it also is implicated in creating CAD.
It is often referred to as Diabetes Mellitus. The word diabetes is Greek for siphon, described by a Greek physician in the second century AD for patients who were passing too much water – like a siphon. Mellitus was added in 1675, as Mel is a Latin word for honey, as the urine and blood of people with diabetes have excess glucose, which is sweet like honey. Folks with this condition attracted ants when they urinated “au natural”.
In the United States there are 29.1 million people or 9.3% of the population who have been diagnosed with diabetes as of 2014 (www.cdc.gov/diabetes) and it is growing every year. There are an additional 8.1 million people with diabetes who are undiagnosed. Rising rates of childhood obesity have rendered it more common in children. According to the International Diabetes Federation, diabetes affects at least 285 million people worldwide, and that number is expected to reach 438 million by the year 2030 (Hu, 2011), making it a global public health crisis. The Metabolic Syndrome (MetS) is a cluster of metabolic abnormalities, which is associated with an increased risk of developing diabetes (Ford, Schulze et al 2008; Wilson, D’Agostino et al 2005).
Insulin is produced in the β-cells of the pancreas, specifically in the pancreatic Islets of Langerhans. The islets sense glucose and produce insulin. Within each islet are several types of cells, which work together to regulate blood sugar. One cell type is the beta cell. After eating, the digested food releases protein and glucose into the blood (Rhoades, Rodney et al 2009), triggering the pancreas to automatically release insulin to move the glucose present in our blood into the cells. As it enters the cells, glucose levels in the blood drop. Insulin regulates the level of glucose or sugar in the blood, and is involved in carbohydrate, lipid and protein metabolism, as well as promoting cell division and growth (Wilcox, 2005), essentially regulating whole body energy.
There are two types of diabetes, Type 1 and Type 2. About ten percent of all diabetes cases are Type 1. In Type 1 diabetes, the body mistakenly sees the insulin producing cells in the pancreas as foreign, and the immune system attacks and destroys them. The beta cells then don’t adequately sense glucose and hence insulin secretion is not stimulated, resulting in elevated glucose levels. This excess glucose eventually passes out of the body in urine. So even though the blood has plenty of glucose, the cells are not getting it for their essential energy and growth requirements. If left untreated, the high levels of blood sugar in Type 1 Diabetes can damage organs, such as eyes, kidneys, nerves, and the heart, and can lead to coma and death.
The treatment for Type 1 Diabetes is to inject insulin into the body, throughout the day, based on testing sugar levels in the blood. The injected insulin then allows the cells to take in the glucose. It can be a challenge to get the dosages of insulin correct, due to the many variables that impact sugar levels in the body, such as activity, diet, stress, emotions, growth, and general health. If you take too much insulin, your body burns too much glucose and your blood sugar can drop dangerously low. This is a condition called hypoglycemia, which can be life threatening. If you take too little insulin, your body can be starved of the energy it needs and your blood sugar can rise to a dangerously high level, called hyperglycemia.
Approximately 90% of all cases of diabetes worldwide are Type 2. Type 2 diabetes, where insulin is not produced in adequate amounts, or where cells in the body do not react to insulin, is known as insulin resistance. In Type 2 diabetes, the beta cells may churn out a lot of insulin, resulting in high glucose levels and high insulin levels in the blood. The body’s tissues are resistant to the insulin and can’t use it properly. As Type 2 progresses over time, the beta cells seem to wear out and eventually produce less insulin. Type 2 diabetes is typically a progressive disease, and often results in the person becoming insulin dependent, as their β-cells don’t produce enough of it.
Type 2 diabetes is also referred to as adult onset diabetes, since it typically develops after age 35, though a growing number of children are developing Type 2 diabetes. Type 2 diabetes (T2D) is treated via diet, oral medication, or with insulin to control the blood glucose levels. Diet and the associated gut bacteria connection are now the focus of the expanding research into T2D.
Complications
The disease of diabetes increases your risk for many serious health complications, which can develop gradually (Kendall & Harmel, 2012). The worst complication is cardiovascular disease, and the most common cause of death is coronary heart disease. Two thirds of diabetic patients die prematurely from stroke or heart disease. Life expectancy is five to ten years shorter. Adults with diabetes have cardiac mortality rates about 2-4 times higher than adults without diabetes and the risk for stroke is 2-4 times that of individuals without diabetes. Other major complications include nerve damage (neuropathy), kidney damage, eye damage, foot damage which doesn’t heal and which lead to amputations, and Alzheimer’s disease. It is estimated that 37.99% of diabetic patients have chronic kidney disease ( Mounasree et al, 2018).
Among 198 patients with type-2 diabetes mellitus and normal or slightly impaired renal function, it was more likely that the patients had an arterial calcification score above the median for a 2.72-fold increment in plasma dp-ucMGP. This association was independent of sex, age, previous cardiovascular disease, and total uncarboxylated MGP plasma levels (Liabeuf et al, 2014). And the calcification marker MGP was found to be elevated in patients with type 2 diabetes and/or heart disease (Thomsen et al, 2010).
With Preamble, lets talk Bone and its role as a hormone generator:
In recent years, exciting advances in bone biology have identified the skeleton as an endocrine organ, and as a key regulator of some metabolic pathways, and feedback loops, particularly insulin signaling and glucose tolerance (Chen, Tian et al 2012; Faienza et al, 2015).
Bone has been regarded as a structural organ for centuries (Confavreux, 2011; Chen, Tian et al 2012; Faienza et al, 2015). This structural function, provided by the skeleton, mechanically supported the body, protected the organs of the body, enabled locomotion and functioned as a reservoir for normal mineral metabolism.
However, bone is a dynamic structure and an active tissue, which is constantly renewing itself through a process called remodeling, which repairs microdamage and heals fractures (Faienza et al 2015). Bone remodeling occurs throughout life in a constant and balanced manner, and it accommodates the bone’s work of weight bearing, growth and repair, as well as for the need for calcium in the body. The process of remodeling depends upon two antagonistic cell populations: the osteoblasts and osteoclasts which work closely together.
Trivia: your bone replaces itself about every 5 years completely - - the wow factor.
Bone contains three types of cells: osteoblasts, osteocytes and osteoclasts.
Osteoblasts come from stem cells, and are bone forming cells. They are primarily responsible for replacement of new bone, synthesizing and depositing the mineralized, collagen-rich matrix that composes bone tissue. Osteoblasts produce hydroxyapatite, a very strong and dense mineralized tissue, which forms bone and makes up the skeleton. This tissue is also a very important store of minerals for the body. Osteoblasts also produce and secrete specialized proteins, such as osteocalcin, which are part of the organic matrix of bone. Osteoblasts also have different receptors that help them participate in this process, one of them being a functional insulin receptor, meaning they receive signals from insulin and participate in the endocrine loop (Hauschka, Lian et al 1989; Punn, Lau et al 1989, Kream, Smith et al 1985). Insulin signaling in osteoblasts enhances osteocalcin activity; as insulin triggers the release of osteocalcin, it promotes the ability of osteoblasts to enhance bone resorption which in turn impacts glucose homeostasis or balance.
Osteocytes are bone cells formed from mature osteoblasts, and are the most abundant bone cells. Osteocytes become entrenched within the mineralized bone matrix, communicate to a surface layer of osteoblasts, and help in maintaining the skeleton. They manufacture collagen and other substances that make up the bone extracellular matrix (Karsenty & Wagner 2002, Bonewald 2007, 2011).
Osteoclasts are a type of bone cell, which breaks down bone tissue and resorbs bone. This function is critical in the maintenance, repair, and remodeling of bones of the skeleton. During bone resorption, the osteoclast attaches to the surface of the bone and creates a sealed compartment, which allows the bone tissue to be disassembled and digested at a molecular level. During resorption, the osteoclast acidifies the compartment, and the acid dissolves the minerals in the bone. Along with dissolving bone, this acidified environment also leads to the decarboxylation of the bone protein osteocalcin, into uncarboxylated osteocalcin, which is then released into the bloodstream (Poser & Price, 1979; Rodan & Martin 2000,Teitelbaum 2000, Harada & Rodan 2003, Teitelbaum & Ross 2003, Karsenty 2006; Lacombe, Karsenty & Ferron, 2013).
Bone remodeling is characterized by alternating phases of destruction by osteoclasts and bone formation by osteoblasts (Ducy, Schinke et al 2000). Bone remodeling occurs daily in multiple locations in an organ covering a very large surface area.
The Endocrine Loop between Diabetes and Bone – Osteocalcin - - - Just when you thought bone was bone, it turns out “Bone” is a “busy system”
Research indicates that bone does much more than support and ambulate the body. Bone and bone proteins are centrally involved in regulating energy metabolism, and osteocalcin is the element that coordinates the two processes, regulating energy metabolism while also providing the energy needed for the bone remodeling process (Lin et al, 2018).
Bone remodeling, the destruction and formation of bone, occurs constantly throughout the skeleton, and requires a large energy input. It is metabolically expensive for the body. In the past decades, with the development of technology, we found that the skeleton does more than support the body, it also functions as an endocrine organ, which regulates several metabolic processes (Yoshikawa, Kode, Xu, et al 2011; Shao et al, 2015; Faienza et al 2015). In fact, the skeleton can be considered an endocrine organ because of its capacity to secrete osteocalcin (OCN), which is a bone specific protein.
Osteocalcin is a 49 amino acid, bone matrix, noncollagen protein, secreted by osteoblasts, and dependent on vitamin K. When enough vitamin K is available, osteocalcin becomes carboxylated and is secreted by the osteoblasts in a fully carboxylated form (Price, 1989; Hauschka, Lian et al 1989; Taylor et al 1990; Engelke, Hale et al 1991). This carboxylated osteocalcin has a high affinity for the extra cellular bone matrix, and binds to the bone (Mundy & Poser, 1983; Nishimoto, Chang et al 1985; Glowacki & Lian, 1987; Hauschka & Wians, 1989; Hauschka, Lian et al 1989; Poser, Esch et al 1998?; Bugel, 2008).
Later, during the reabsorption and bone remodeling phase, when the bone mineral matrix becomes acidified by osteoclasts, some of the carboxylated osteocalcin decarboxylates, and it is released into the blood stream to circulate (Price, Williamson, et al 1981; Hauschka, et al 1989, Price, 1989; Engelke, Hale et al 1991; Ivaska, Hentunen et al 2004). Research shows that bone resorption is a key mechanism promoting osteocalcin bioactivity and that this bone remodeling is also involved in a feedback loop that regulates whole body glucose homeostasis (Lee et al, 2007; Ferron, Wei, et al 2010).
One can find fully carboxylated, partially carboxylated, and completely uncarboxylated forms of osteocalcin circulating in the bloodstream (Plantalech et al. 1991, Cairns & Price 1994, Vergnaud et al, 1997, Schilling et al. 2005, Ferron et al. 2010a).
Note: Your body will NEVER let you be fully carboxylated.
Both forms of osteocalcin are necessary and important for glucose metabolism. Uncarboxylated osteocalcin is thought to function as a hormone, increasing β-cell proliferation, insulin secretion, and insulin sensitivity (Yoshikawa, Kode et al 2011; Ducy, 2011; Clemens & Karsenty, 2011; Yoshizawa, 2012). And ucOC seems to play a key anti-inflammatory role by mitigating oxidative stress (Guedes et al, 2018; Lin et al, 2020).
And carboxylated osteocalcin is a necessary prerequisite, before the uncarboxylated osteocalcin can be freed to circulate in the bloodstream (Yoshizawa et al, 2012; Ferron et al 2016). Thus both carboxylated and uncarboxylated osteocalcin function to regulate insulin signaling in a feed-forward loop, in which insulin affects osteoblasts and in turn increases its own secretion and sensitivity via uncarboxylated osteocalcin (Giovanni et al, 2014). Levels of osteocalcin are much more than a simple marker of bone formation, but also represent a major component of the complex relationship between bone and energy metabolism (Dumitru et al, 2019).
VItamin K influences the degree of carboxylation of osteocalcin, and variations in carboxylation status would be due to differences in vitamin K intake (Price et al 1981). The percentage of circulating ucOC has been shown to be the most sensitive measure of vitamin K nutrition in humans and is responsive to dietary vitamin K depletion, repletion, and supplementation (Binkley, et al, 2000; Binkley, et al 2002; Sokoll, et al, 1997).
Research
The connection between the skeleton and glucose metabolism is an emerging area of intense scientific scrutiny. Previously, in 1994, it was discovered that mice lacking osteocalin in osteoblast bone cells, had an increased secretion of urine, were obese, and became diabetic, one of the earliest indicators that bone was involved in glucose regulation and energy metabolism (Ducy et al, 1994; Lee et al, 2007; Katsnelson, 2010; Karsenty & Ferron, 2012).
A series of studies found a positive feedback loop between bone and pancreatic islet cells, which identified the crucial role for osteocalcin in regulating insulin metabolism in a hormonal way. Studies by the Karsenty group showed that mice lacking osteocalcin accumulate visceral body fat, become obese, and exhibit dramatic impairments in glucose metabolism with elevated glucose and lipid concentrations, increased insulin resistance, and reduced insulin levels and glucose tolerance (Karsenty & Ferron, 2012; Ducy et al 1996; Lee, Sowa et al 2007, Ducy, Desbois et al 1996). The serial studies performed by Karsenty and colleagues have suggested that OCN exerts endocrine regulation on pancreatic islets, fat and testis, and links bone and these organs to form feedback loops (Ducy, Amling et al 2000; Oury, Sumara et al 2011; Lee, Sowa et al 2007; Ferron, Wei et al 2010). Since osteocalcin is only produced by osteoblasts and can enter the circulation, Karsenty speculated that osteocalcin functions as a hormone (WOW !!)
These findings remained unexplained until 2007, when Lee and colleagues studied genes that regulated osteocalcin levels in the blood, and identified the Esp gene as a powerful regulator of glucose metabolism in mice. They found that mice without the Esp gene show high levels of uncarboxylated osteocalcin in the blood, beta cell proliferation in the pancreas, increased insulin secretion and sensitivity, increased adiponectin, as well as impaired glucose metabolism, or hypoglycemia. These pioneering studies were the first to demonstrate the regulation of energy metabolism by the skeleton via osteocalcin. The effect on glucose metabolism was so severe that a portion of the esp -/- mice did not survive until weaning (Lee, Sowa et al 2007; Ferron, Wei et al 2010).
To further explore the biological role of osteocalcin, mice were created that lacked an insulin receptor (InsR) in their osteoblast bone cells. These mice were found to have abnormal bone development, increased fat mass, increased serum glucose, increased insulin levels, an associated impairment in glucose tolerance, and decreased pancreatic β-cell mass (Ferron, Hinoi, et al 2008; Ferron, Wei 2010, Fulzele, Riddle et al 2010). Interestingly, both total and undercarboxylated osteocalcin levels were reduced in these InsR knockout mice, and when they were administered undercarboxylated osteocalcin, the metabolic disturbances were partially alleviated (Fulzele, Riddle et al 2010), as their insulin sensitivity and glucose tolerance improved, clearly highlighting the importance of osteocalcin in energy metabolism. It seemed that the insulin signaling in osteoblasts enhanced the activity of osteocalcin and conversely, osteocalcin influenced the pancreatic beta cells to release insulin in an endocrine feedback loop linking bone proteins to insulin levels (Lee, Sowa et al 2007; Hauschka et al 1975; Price et al 1976; Hauschka et al 1989; Ferron, Karsenty, Ducy, 2008; Ferron, Wei, et al 2010; Fulzele et al 2010; Ferron, McKee et al 2011; Mizokami, Yasutake et al 2013; Mizokami, Yasutake et al 2014; Wei, Ferron et al 2014). And when mice received injections of osteocalcin, they showed an improvement in arterial stiffness (Huang et al, 2017).
When diabetes was induced in mice, vitamin K1 helped prevent beta islet destruction as seen in Type 1 diabetes, which often leads to a reduction in insulin secretion and hyperglycemia (Varsha et al, 2015). And the vitamin K1 led to a significant increase in plasma insulin. They concluded that the level of vitamin K1 could be crucial in protecting the animals from oxidative insults arising from diabetes. In another animal study a pharmacological dose of vitamin K2 and estradiol suppressed the development of arteriosclerosis associated with diabetes (Seyama et al, 2013).
Gene expression is now being studied, and recent research indicated that giving vitamin K2, specifically MK4, significantly improved the glycemic status in rats with type 2 diabetes. They were able to show that the MK4 induced osteocalcin gene expression, which had numerous beneficial effects, such as decreasing insulin resistance and decreasing insulin sensitivity (Bilotta, et al 2018: Hussein, Mohamed et al, 2018).
The research has continued to explore the role of osteocalcin (Motyl et al, 2010; Magni, Macchi et al 2016). The research can be divided by the type of osteocalcin measured, as their understanding grew and as their research tools were developed. The early studies began with measuring total osteocalcin and its effect, then shifted to uncarboxylated osteocalcin as a possible endocrine hormone, and then to carboxylated osteocalcin, as their understanding of the relationship between osteocalcin, energy metabolism, and vitamin K has advanced.
Total Osteocalcin (OCN) -
Much of the early research simply looked at the total osteocalcin levels that could be measured in the blood, partly because they lacked the tools to study it more specifically. That early research indicated that total osteocalcin concentrations, which include both carboxylated and uncarboxylated forms, definitely played a role in glucose homeostasis (Kindblom, Ohlsson et al 2009; Pitta, Harris et al 2009; Fernandez-Real et al 2009; Kanazawa, Yamaguchi et al 2009; Reinehr, Roth 2010). Ranzi (et al, 2019) concluded that blood levels of uncarboxylated osteocalcin may be an early symptom of insulin resistance in obese patients.
Serum osteocalcin levels are generally low in patients with diabetes.
Research indicated that total osteocalcin levels are seen as an independent negative predictor for blood sugar levels, meaning if osteocalcin levels were low, then blood sugar levels would be high. Lower concentrations of total OC were described in children with type 1 diabetes, and was also linked to decreased bone formation, though it was not understood why (Kruse, Kracht, 1986). Lower total osteocalcin concentrations were also found in adults with type 2 diabetes, when compared to healthy subjects . Patients with type 1 and type 2 diabetes were matched with control groups and the research showed that the serum osteocalcin and vitamin D levels were significantly decreased in type 2 diabetic patients (Plietschmann, et al 1988).
When osteocalcin levels in the blood dropped, blood sugar levels would go up and stay up, as did fasting insulin markers, inflammation markers, and body fat (Plietschmann et al 1988; Inaba, Nishizawa et al 1999; Kanazawa, et al 2009; Kanazawa, Yamaguchi et al 2011; Pitta, Harris et al 2009; Kindblom, Ohlsson et al 2009; Gravenstein, Napora et al 2011). We know osteocalcin levels are lower in type 2 diabetics (Im, Yu, Jeon et al 2008; Diaz-Lopez et al 2013; Sarkar & Choudhury, 2012; Oosterwerff, van Schoor et al, 2013; Gower, Pollock et al 2013).
Serum osteocalcin levels increase when glycemic control improves.
A study by Rosato et al, from 1998 was one of the earliest reports showing an association between glucose metabolism and OC. Diabetic patients were compared to healthy subjects and baseline levels of serum OC were significantly lower in diabetic patients. An improvement in glycemic control raised the serum levels of insulin like grown factor 1 (IGF1) (one of its roles is repair) and osteocalcin significantly (Sayinalp, et al 1995; Rosato, et al 1998; Akin, Gol et al 2003; Achemlal, Tellal et al 2005; Dobnig, et al 2006; Cutrim, et al 2007). Others have found that improved glycemic control in poorly controlled diabetic patients increased total osteocalcin serum concentrations and decreased HBA1c (Nagasaka, Murakami et al 1995; Sayinalp, Gedik, et al 1995; Rosato, Schneider et al 1998). Fernandez-Real (et al , 2009) also demonstrated that serum total osteocalcin level was associated with insulin sensitivity in non-diabetes subjects. Components of Metabolic Syndrome were assessed in Chinese men, aged 20 to 69 years, and they found an inverse association of serum Total osteocalcin levels with MetS (Tan, Gao et al 2011), and in a cross sectional study with patients with MetS, osteocalcin was negatively correlated with fasting glucose levels (Bador, Wee, Halim et al 2015).
There is a positive correlation between total serum osteocalcin levels and glycemic control in patients with obesity and the metabolic syndrome (von Mach, Stoeckli et al 2004; Yeap, Chubb et al 2010; Garcia-Martin, Cortes-Berdonces et al 2011; Confavreaux et al 2014).
And this association of lower osteocalcin levels with metabolic syndrome has been found in multiple ethnic groups (Saleem et al 2010), including Japanese men and women (Iki, et al 2012), Korean postmenopausal women (Kanazawa, et al 2009) and Chinese men (Tan, et al 2011). Tan’s study was the first large cross-sectional study to highlight the important relationship between osteocalcin levels and MetS in a Chinese male population. In aging men, results were confirmed in the Health in Men Study (Yeap, et al, 2010) and in the Longitudinal Aging Study Amsterdam (Oosterwerff, et al 2013). Yeap (et al, 2010) corroborated the Kindblom results with a large cohort study that evaluated more than 2760 elderly men and found lower levels of osteocalcin in the presence of metabolic syndrome, as well as worse glycemic and insulin sensitivity indexes. Reduced serum osteocalcin was associated with increased risk of having the MetS in older men (Yeap, Chubb et al 2010). A large observational study of Afro Americans and non Hispanic whites found that osteocalcin was inversely related to the presence of metabolic syndrome, body mass index, fasting glucose and insulin and triglycerides (Saleem, Mosley et al 2010). The severity of the metabolic syndrome was correlated with the lowest levels of osteocalcin. Bouillon (et al 1995) found that osteocalcin levels decreased with age and they were significantly associated with the individual components of MetS.
Osteocalcin levels and glucose metabolism in postmenopausal women, with and without diabetes was also investigated.
They found that patients with Type 2 diabetes showed a significant reduction in osteocalcin levels, compared with the normal glucose and impaired fasting glucose groups. Subjects in the highest quartile for osteocalcin were observed to have significantly decreased fasting glucose and hbA1c (a surrogate test for blood sugar levels over time) levels compared with subjects in the lowest quartile. They concluded that in humans, the skeleton may be involved in energy metabolism by functioning as part of the endocrine system (Im, et al 2008; Shou, Ma et al 2009; Hu, et al 2014).
Also total OCN and ucOCN were related to insulin sensitivity (Bullo, et al 2012; Pitta, Harris et al, 2009; Garanty-Gobacka, et al 2013). After 8 weeks of aerobic exercise training in young obese individuals, a reduction in body fat and improved insulin sensitivity were accompanied by significant increases in serum total OCN and ucOCN (Kim, et al 2015).
Another clue as to why exercise (even moderate) combined with weight loss makes a “difference”.
Studies have now shown that low osteocalcin levels in the blood are associated with an increased risk of developing diabetes.
Others found that Total osteocalcin levels was inversely associated with the development of type 2 diabetes, independent of age, gender, body mass index and fasting sugar levels in the blood (Hwang, et al 2012). They studied 425 subjects who had never been treated for diabetes, and those with low levels of osteocalcin were more likely to develop type 2 diabetes (Garcia-Martin, et al 2011; Gravenstein, et al 2011; Hwang, et al 2012; Ngarmukos, et al, 2012; Lee, Jo et al 2012). Long term studies of patients diagnosed with diabetes and matched controls indicated that total OCN was an independent risk factor for the development of diabetes (Ngarmukos, et al 2012; Diaz-lopez et al 2013).
The MINOS study is a cohort study of osteoporosis and its determinants in men (Szulc, et al 2000). It is the result of a collaborative projecting involving one of the largest local health insurance companies which covers mineworkers and their families living in the French city of Monteau-les-Mines and its surrounding area. It began in 1996 and involves 847 men. They evaluated whether osteocalcin levels were associated with metabolic syndrome severity in men. 30% of the cohort had Metabolic Syndrome. Osteocalcin levels were lower in men with elevated blood glucose. The higher the number of the MetS traits present, the lower the average osteocalcin level was. They concluded that in older Caucasian men, the total osteocalcin level was associated with Metabolic Syndrome severity, and osteocalcin carried the strongest association than any other bone turnover markers. The higher the number of MetS criteria, the lower serum total osteocalcin was (Confavreaux, et al 2014).
1691 postmenopausal belonging to the Nagano cohort study were studied for the relationship between serum OC and diabetes, for an average of 7.6 years. Those with the lowest levels of osteocalcin showed 8 times higher incidence of diabetes when compared to those with the highest levels of osteocalcin. Even when all co-founders were adjusted for, the presence of low osteocalcin levels were a significant and independent risk factor for type 2 diabetes (Urano et al, 2017).
Collectively, these human studies have shown that the serum osteocalcin concentration is negatively associated with the plasma glucose level and body fat mass, (Kanazawa et al 2009; Zhou, Ma et al 2009, Fernandez-Real et al 2009; Kindblom, Ohlsson et al 2008; Shea, Gundberg, Meigs et al 2009; Reinehr &Roth, 2010; SAleem, Mosley, et al 2010), and positively associated with insulin secretion (Zhou, Ma 2009; Hwang, Jeong et al 2009), and lower insulin resistance (Ferandez-Real, 2009; Kindbloom et al 2008; Pittas, et al 2009, Hwang et al 2009; Shea, Gundberg, et al 2009) suggesting that high concentrations of osteocalcin have a protective effect in humans, and low concentrations of osteocalcin are associated with higher metabolic parameters (Pittas, Harris et al 2009; Liang et al, 2016).
Uncarboxylated Osteocalcin (ucOCN) -
As time went on, and as research tools advanced, the data seemed to indicate that it was uncarboxylated osteocalcin released from bone, which was the active form in the energy loop and which had the capacity to regulate insulin production and sensitivity. It seemed that ucOC acted as a circulating hormone to stimulate insulin production and secretion by pancreatic beta-cells and adiponectin by adipocytes (Lee, Sowa et al 2007: Lin, et al, 2018).
Uncarboxylated osteocalcin is associated with increased proliferation of pancreatic beta cells and increased insulin secretion and insulin sensitivity.
The early work by Lee et al (2007) and Ferron et al (2008) pointed to uncarboxylated osteocalcin as the key factor that enhanced insulin sensitivity and insulin production, lowered blood glucose, and decreased visceral fat in both genders, and functioned as a mediator of energy metabolism between bone, the pancreas and fat tissue. When osteocalcin was administered to wild type or regular mice, the ucOC stimulated the proliferation of pancreatic beta-cells and insulin secretion in vitro, and increased adiponectin production in fat cells, which resulted in increased insulin sensitivity. In turn, the insulin triggered the release of osteocalcin, which then becomes uncarboxylated and loops back to enhance insulin production and sensitivity (Ferron, et al 2008; Ducy, et al 1997; Ferron, et al 2012). ucOC appeared to function as a hormone.
Uncarboxylated osteocalcin has an inverse relationship with markers of the metabolic syndrome, such as beta cell function, insulin and blood glucose levels. This means that when ucOC goes up, the markers go down, and health improves. Several human studies have described a positive inverse association between serum undercarboxylated osteocalcin levels and β-cell function, insulin, blood glucose levels, and calciphylaxis (Hwang et al, 2009; Levinger et al., 2011; Kanazawa, et al, 2011; Kanazawa et al 2011; Pollock, et al 2011; Iki, Tamaki et 2012; Bullo, et al 2012; Hwang, et al 2012; Furusyo, et al 2013; Wang et al 2013; Chen et al 2014; Niqwekar et al 2017; Riquelme-Gallego et al, 2020).
Serum levels of ucOC negatively correlate with insulin resistance, obesity, diabetes or markers of the metabolic syndrome (Pittas, et al 2009; Hwang, et al 2009; Pollock, et al 2011; Kanazawa, et al 2011; Diamanti-Kandarakis, et al 2011; Ogawa-Furuya, et al 2013; Yano, et al 2015). Korean men with higher ucOC levels had better glucose tolerance. Once the men developed diabetes, the osteocalcin levels measured in their blood decreased (Hwang, et al 2009). UcOC has been associated with plasma glucose levels in men with Type 2 diabetes (Kanazawa, et al 2010; Kanazawa, et al 2011). Japanese men had ucOC levels that were significantly inversely correlated with the glycemic index and insulin resistance (Iki, et al 2011). A later study found that ucOC levels were associated with glycemic status and insulin resistance in the general Japanese population (Iki, et al 2012). A recent study of Australian men, age 70-89 years, indicated that higher ucOC was associated with a reduced risk of diabetes. They concluded that higher ucOC is both a marker of bone remodeling as well as an independent predictor of reduced risk for diabetes (Yeap, et al 2015).
One study reported that elevations in serum undercarboxylated osteocalcin levels predict reductions in serum glucose levels following aerobic exercise in obese and diabetic men (Levinger, et al 2011), while others have reported undercarboxylated osteocalcin levels correlate inversely with body weight and fat mass (Schafer, et al 2011; Kanazawa, et al 2011). A study of postmenopausal women and men with type 2 diabetes, showed that serum ucOC levels were inversely associated with glycemic status and insulin resistance in the general population of Japanese men (Iki, et al 2012).
A review examined the epidemiological and interventional evidence associating osteocalcin and uncarboxylated osteocalcin with metabolic risk and cardiovascular disease, and concluded that current observational and indirect interventional evidence supports a relationship between uncarboxylated osteocalcin with metabolic and cardiovascular disease (Levinger et al, 2017). Another cross-sectional study of patients with Metabolic Syndrome showed that circulating ucOC identified increased cardiovascular and type 2 diabetes risk and explores whether ucOC can be used as a treatment (Riquelme-Gallego et al, 2020).
It has been shown that ucOC levels are correlated with several metabolic variables in children. Higher levels of ucOC are associated with higher insulin secretion and higher levels of adiponectin in healthy children, while lower concentrations of ucOC are associated with impaired fasting gucose and impaired glucose tolerance in children (Prats-Puig, et al 2010; Pollock, et al 2010). The prediabetes group had significantly lower ucOC and Total OC levels, and higher fasting glucose and insulin levels, compared to the normal glucose group. The results suggest that the lower uncarboxylated osteocalcin levels observed in the overweight children at risk for diabetes could be contributing to beta cell dysfunction.
There was some consideration that perhaps it was the ratio or proportion of uncarboxylated OC, relative to the carboxylated OC, that functioned as a metabolic signal; that a shift in the proportion of ucOC and cOC might affect the physiological actions of this hormone (Hinoi, et al 2008). Villafan-Bernal (et al 2014) assessed the relationship between the ucOC/cOC index and glycemic status markers, such as fasting levels of sugar in the blood, fasting insulin. They found subjects with ucOC/cOC index less than 0.31 had a 12.6 x increased probability to have type 2 diabetes. They concluded that ucOC/cOC index could be a risk factor to type 2 diabetes and might be used as a good marker of poor metabolic control in T2D - - - this is key - - - (too much or too little is not good)
Carboxylated OCN -
While the initial research pointed to uncarboxylated osteocalcin as the key hormone linking bone to energy metabolism (Pi, et al 2011; Mizokami, et al 2013; Ferron, et al 2012; Rached, et al 2010; Zhou,et al 2013), there were many conflicting results, where carboxylated osteocalcin was shown to have a strong relationship to glucose metabolism. It has not been determined whether the metabolic actions of osteocalcin are restricted to undercarboxylated forms (Brennan-Speranza & Conigrave, 2015). The results of studies in glucocorticoid-treated mice with replacement of osteocalcin suggest that both the carboxylated and undercarboxylated forms are hormonally active (Brennan-Speranza, et al 2012).
Carboxylated osteocalcin is associated with improved glucose tolerance and insulin sensitivity.
Among middle-aged males, elevated serum cOC as well as ucOC levels are associated with improved glucose tolerance and insulin sensitivity, as well as enhanced β-cell function (Hwang, et al 2009). In healthy older men and women, elevated carboxylated osteocalcin concentrations are associated with lower insulin resistance. It appears that the uncarboxylated form was related to insulin secretion, and the carboxylated form was associated with insulin resistance (Shea, et al 2009;). Brennan-Speranza (et al 2013) demonstrated that both uncarboxylated and carboxylated forms of osteocalcin, which are both bioactive, had a similar effect. Both forms of osteocalcin improved insulin resistance and glucose tolerance in a mouse model. The different forms of osteocalcin, carboxylated and uncarboxylated, exert different effects with respect to potency and specific cellular actions and add complexity to metabolic regulation. Elderly men and women from Spain (PREDIMED trial), were followed for a median of 5.9 years, to determine the incidence of new onset diabetes. They found that low concentrations of both carboxylated OC and uncarboxylated OC were significantly and independently associated with an increased risk of developing type 2 diabetes. Although both forms of OC were inversely associated with the risk of developing diabetes, only cOC showed an inverse relationship with glucose metabolism-related parameters. This five year follow up study showed that low concentrations of carboxylated OC were involved in the development of diabetes. (Diaz-Lopez et al 2013; Ngarmukos, et al 2012). In addition, changes in insulin sensitivity were associated with changes in carboxylated OC but not ucOC (Choi, et al 2011).
A middle aged Asian population was studied to assess the relationship between undercarboxylated osteocalcin and carboxylated osteocalcin with metabolic syndrome. They found that undercarboxylated osteocalcin was increased in subjects with metabolic syndrome. Interestingly, they found a gender difference, in that middle aged Asian females with metabolic syndrome had higher levels of under carboxylated osteocalcin and lower levels of carboxylated osteocalcin. This relationship was not found in Asian males (Liu, et al 2013). In this study of a female population, both carboxylated and undercarboxylated osteocalcin were associated with metabolic syndrome but the direction between the two associations was different (obviously the impact of gender based hormones).
A meta-analysis investigated the associations between osteocalcin and fasting plasma glcose (FPG) and glycated hemoglobin A1c, using the databases of Pubmed, ISI web of science and the Cochrane library from 2007 to 2014 to identify related studies. The meta-analysis included 39 studies involving 23,381 participants. The meta-analysis found that both total OCN and undercarboxylated Ocn were negatively related with plasma glucose levels, with the association being more pronounced in men. The magnitude of the correlation between osteocalcin and glucose levels was significantly higher in men than in women. The negative correlations mean that as there was lower osteocalcin, that fasting plasma glucose or sugar levels in the blood were higher (Liu, et al 2015).
Carboxylated osteocalcin is associated with metabolic parameters such as adiponectin and body mass index.
An investigation was conducted of the uncarboxylated and carboxylated osteocalcin, adiponectin, and insulin secretion in healthy prepubertal children. The results indicated that it was carboxylated osteocalcin, the active form in the bone that was related to adiponectin, while uncarboxylated osteocalcin was related to insulin secretion (Prats-Puig et al 2010). Hill, et al (2014) found that both carboyxlated and uncarboxylated osteocalcin directly increased insulin sensitivity, and increased glucose transport in adipocytes and muscles, and suppressed pro inflammatory cytokine secretion.
Carboxylated osteocalcin functions as a negative regulator of osteocalcin as a hormone.
In 2015, Lacombe & Ferron showed that the carboxylated form of osteocalcin negatively regulates endocrine functions (Lacombe & Ferron, 2015). Insulin signaling in osteoblasts triggers the release of carboxylated osteocalcin which is deposited into the bone matrix. Bone resorption by osteoclasts then decarboxylates the osteocalcin, and releases it into circulation (Ferron et al 2010). The uncarboxylated osteocalcin then circulates to stimulate insulin secretion by the beta cells and to promote insulin sensitivity in peripheral organs (Zoch, et al 2015). Their work provides direct evidence that γ-carboxylation of OCN is a negative regulator of its endocrine function, because if γ-carboxylation is not present, then the sequence is interrupted and decarboxylated osteocalcin is unavailable to circulate as a hormone affecting glucose metabolism. These results provide the first genetic in vivo evidence that γ-carboxylation of OCN is absolutely necessary for its accumulation in the bone ECM, where it can then be modified during bone resorption (Lacombe & Ferron, 2015).
In newly emerging work, Ferron (et al 2015) directly assessed the influence of carboxylation on the osteocalcin endocrine function in vivo. His team was able to establish that the carboxylation of OCN is absolutely required for it to accumulate in the bone matrix. Uncarboxylated osteocalcin binds poorly, if at all, to bone matrix, and it is necessary for osteocalcin to be carboxylated for it to bind to the bone matrix, so as it can later be decarboxylated into circulation, and participate in the glucose metabolic regulation. The studies support the conclusion that uncarboxylated OC is the active form of the hormone in vivo and that carboxylation negatively regulates both the bioactivity and the bioavailability of osteocalcin. This work established, at least in mice, that carboxylation negatively regulates both the bioactivity and the bioavailability of osteocalcin.
This work demonstrates the novel role for vitamin K. With adequate amounts of vitamin K, osteocalcin becomes carboxylated before it is secreted to the bone. Without carboxylation, uncarboxylated osteocalcin cannot be released to function as a hormone. Future studies will further elucidate this relationship. “We confirmed that osteocalcin's hormonal activity relies on vitamin K, which in turn participates in the gamma-carboxylation process. …. osteocalcin is controlled by carboxylation, a process that modifies the hormone’s function and relies on vitamin K. " adds Dr. Ferron. This work demonstrates the novel role for vitamin K dependent gamma carboxylation in the control of glucose metabolism (Lacombe & Ferron 2015).
Given that uncarboxylated osteocalcin has been used as a marker of vitamin K deficiency, and that generally carboxylation of vitamin K dependent hormones has healthy outcomes, it created confusion for a deficiency marker to be a key marker of diabetic health. It has now become clear that while both play crucial roles in glucose metabolism, the required first step is the adequate carboxylation of osteocalcin.
There is an emerging notion that osteocalcin could be a treatment for type 2 diabetes (Ferron, Mckee et al 2012)
Here is Where Vitamin K “fits in”
Micronutrients are being recognized as an important nutritional therapy for the prevention and/or management of diabetes and its associated health risks. Although a very small quantity of micronutrients are required for specific function in our body, moderate deficiencies can lead to serious health issues (Manna & Kalita, 2016). Vitamin K is a micronutrient that has been increasingly recognized as an important strategy to reduce complications and improve clinical features of pre-diabetes and diabetes (Yeh, et al, 2003).
Vitamin K is a fat-soluble vitamin that is necessary for blood coagulation factors and clotting, and is also necessary to active key proteins in the body, also known as Gla-containing proteins. In recent years, research has identified at least 17 vitamin K-dependent (VKD) proteins throughout the body, located in various tissues. These vitamin K dependent proteins rely on adequate amounts of vitamin K in order to be carboxylated and activated, so as to become bioavailable in the body (Shiraki, et al, 2015). Osteocalcin is one of the proteins in the body that depend on vitamin K to be carboxylated and activated. Data has shown that vitamin K1 insufficiency is followed by higher levels of undercarboxylated OC (Tsugawa et al 2008; Zwakenberg et al, 2019). (thus the all important ratio is thrown off). Reviews of the preclinical and clinical evidence show that vitamin K supplementation improves insulin sensitivity and glucose tolerance (Prasenjit & Jatin, 2016; Al-Suhaimi & Al-Jafary, 2020; Karamzad et al, 2020). High intake of vitamin K2 and higher status of vitamin K are associated with lower prevalence of metabolic syndrome (Dam et al, 2015).
Vitamin K supplements delayed the insulin response.
In 1999, Sakamoto reported that a low vitamin K diet induced glucose intolerance in rats (Sakamoto, et al 1999). Similar results have been shown in small-scale human studies among young men with a low risk of diabetes. In an attempt to elucidate the role of vitamin K in the pancreas, healthy young males with a higher percentage of ucOC, took 90 mg of MK4 per day (menaquinone 4) for one week. Their acute insulin response time was significantly decreased after only one week. Interestingly, the subjects who had lower vitamin K levels, exhibited the largest decrease in insulin secretion, suggesting that vitamin K may play an important role in the acute insulin response in glucose tolerance (Sakamoto, et al 2000).
High intakes of Vitamin K have been associated with greater insulin sensitivity (or glycemic markers).
Recently two large studies investigated the relation between dietary phylloquinone and insulin sensitivity. An observational study of 2,719 women showed that high vitamin K1 intake, phylloquinone, was associated with improved insulin sensitivity and glycemic control. In a group of healthy volunteers between 26 and 81 years old, higher dietary vitamin K1 intake was associated with greater insulin sensitivity and lower post meal glucose levels (Yoshida, et al 2008; Li, et al 2018; Ho et al, 2020).
Note: this in part has to do with the respective gut bacteria that can liberate the K-1 from the “food” (a topic for another article).
Vitamin K has been found to have a direct impact on the diabetic state itself. The main disruption in diabetes and pre-diabetes is hyperglycemia, and vitamin K may have an effective response.
A randomized controlled trial showed improved insulin sensitivity after phylloquinone supplementation among men. Healthy men and women, between the ages of 26 and 81 years, without diabetes, were given 500 micrograms of phylloquinone (vitamin K1)/ per day for 36 months. It was associated with a significant decrease in insulin resistance in men but not in women and a reduced progression of insulin resistance (Yoshida, et al 2008).
A more recent study investigated whether supplementing with Vitamin K1 would affect glucose metabolism or insulin sensitivity in prediabetic and premenopause women. 82 prediabetic women were given vitamin K1, of 1000 micrograms daily for 4 weeks. The K1 supplementation increased the serum levels of cOC and decreased ucOC, compared with placebo, and increased insulin sensitivity. They found that phylloquinone supplementation improved the glycemic status in premenopausal prediabetic women. The results demonstrated that vitamin K1 supplementation for 4 weeks did not affect insulin resistance in premenopausal and pre-diabetic women, but had beneficial effects on glycemic status and insulin sensitivity (Rasekhi, et al. 2015.)
And MK7 has been shown to be effective in improving glycemic indices in men and women with Type 2 diabetes (Karamzad et al, 2020). They were given 200 ugs a day for twelve weeks. Compared to the control group, those receiving MK7 had significantly lower fasting blood sugar and inflammation. While MK4, which is present in large amounts in the pancreas, was found to help regulate insulin (Ho et al, 2019). A recent study found that even 360 ug of MK7 for twelve weeks reduced fasting plasma glucose and HbA1c in patients with Type 2 Diabetes. And the number of patients who reached the glycemic control targets was significantly higher in the vitamin K2 group compared to the placebo group (Sakek et al, 2020).
Two studies conducted by Dihingia et al (2018) evaluated the impact of vitamin K1 administration in an animal model of diabetes after 8 weeks of 1,3 and 5 μg/kg body weight (BW)/day administration of vitamin k1. The results demonstrated that circulating VK1 has a positive effect on lowering fasting glucose and insulin resistance in T2D. They also demonstrated that circulating VK1 was significantly lower in T2D patients compared to age-matched control subjects and VK1 levels in T2D were significantly and inversely associated with fasting glucose and insulin resistance. These results suggest that boosting plasma VK1 may reduce the fasting glucose and insulin resistance in T2D patients.
Vitamin K intake has been shown to improve insulin resistance in people with diabetes.
12 healthy young male volunteers were given 1 week of vitamin K supplements (90 mg of MK4) to examine the impact on the pancreas. After only one week, markers of vitamin K absence decreased and the amount of insulin in the blood (IRI) was reduced. They concluded there was a relationship between pharmacological dose of vitamin K and insulin response ( Sakamoto, et al 2000).
A cross-sectional study was done, using the Framingham Offspring Cohort) of 1247 men and 1472 women, examining the effects of phylloquinone administration over 3 years on carbohydrate metabolism. They found that higher vitamin K intake was associated with greater insulin sensitivity and glycemic status and showed an improvement in insulin resistance (HOMA-IR) in male but not female subjects. In older, non diabetic men, three years of supplementation with 500 micrograms/day of vitamin K1 produced a significant reduction in insulin resistance compared with controls (Yoshida, et al 2008).
In a study of healthy young men, just four weeks of supplementation with 30 mg of vitamin K2 (as MK-4), three times daily, improved insulin sensitivity. They gave vitamin K2 supplements for 4 weeks, to see the impact on beta cell function and/or insulin sensitivity in healthy young male subjects. They found that vitamin K supplementation significantly increased the insulin sensitivity index. The increased insulin sensitivity seemed to be related to the increased carboxylated OCN. They concluded that the carboxylation of osteocalcin by vitamin K may be the key for increasing insulin sensitivity in humans (Choi,et al 2011). Note: this study also validated the safety of “high dose” MK-4.
Diabetic patients often present with dyslipidemia, characterized by elevated triglycerides (TG), low levels of highâ€density lipoprotein cholesterol (HDLâ€C), and predominance of smallâ€dense low density lipoprotein (LDL) particles (Vollenweider et al, 2015; Chawla et al 2016). A recent study assessed the relationship between intake of vitamin K and markers for insulin resistance and Type 2 diabetes, in a longitudinal analysis of elderly subjects at high cardiovascular risk. The subjects were drawn from the PREDIMED study, which is a large, parallel group, multicenter, controlled, randomized, clinical trial designed to evaluate the effect of the Mediterranean diet on the primary prevention of cardiovascular disease in elderly. Participants were community-dwelling men and women aged 55–80 and 60–80 years, respectively. At baseline, they were free of cardiovascular disease and were either diabetic or met at least three or more coronary heart disease risk factors including smoking, hypertension, or treatment with antihypertensive drugs, dyslipidemia, high-density lipoprotein cholesterol level of 40 mg/dL or lower, overweight, or with a family history of premature cardiovascular disease. The results showed, for the first time, that an increased dietary intake of phylloquinone is associated with an improvement in inflammatory and other metabolic risk markers related to insulin resistance and diabetes, thus supporting a protective role of vitamin K on low-grade chronic inflammatory diseases (Juanola-Falgarona et al 2013).
Vitamin K intake associated with improved retinopathy.
Research shows that active MGP helps to maintain retinal microcirculation, with might be considered to be a marker of retinal health (Wei et al, 2018). In rats treated with vitamin K1, there was a decrease in the blood glucose level, ALR2 (aldose lens reductase activity 2), and accumulation of lens sorbitol. The study indicated that vitamin K1 was a potent inhibitor of ALR2 and may represent a mechanism of vitamin K1 on diabetes-related cataract formation (Varsha et al, 2014; Tiagarajan et al, 2019).
Vitamin K intake associated with lower risk of developing chronic kidney disease, or nephropathy.
Kidney disease for people with diabetes is a serious complication. Matrix gla proteins appear to be a predictor of mortality in patients with diabetic kidney disease (Roumeliotis et al, 2017). There was a strong inverse correlation between the circulating dp-ucMGP levels and stages of chronic kidney disease, suggesting that MGP was a predictor or mortality in patients with diabetic nephropathy (Puzantian et al, 2018).
Vitamin K intake associated with lower risk of developing diabetes or MetS.
The relationship between dietary intake of vitamin K and metabolic syndrome (MetS) was investigated to determine the impact of vitamin K intake, phylloquinone, and Metabolic Syndrome. The National Health and Nutrition Examination Survey (NHANES) 1999-2004 found that vitamin K intake in the highest, compared with the lowest, quintile was associated with lower prevalence of hyperglycemia as a component of metabolic syndrome (Pan & Jackson, 2009). They performed a cross sectional analysis on data from 5800 adults aged 20 to 45 years who participated in the national health and nutrition examination survey (1999-2004). They found that the individuals with the highest phylloquinone intake, had the lowest prevalence of MetS and its 5 components. The highest quartile of intake was associated with significantly reduced risks of low HDL level, and hyperglycemia and hypertriglyceridemia. In general, participants who had MetS or its element consumed less phylloquinone from diet compared to those who did not. Those with the highest intakes of phylloquinone had a reduced prevalence of MetS (Pan & Jackson, 2009).
One study with animals receiving 5 mg per kilogram of weight, twice a week of vitamin K1 for three months showed a significant reduction in microalbuminuria, urea, uric acid, urinary albumin and early onset diabetic nephropathy (Varsha et al, 2015).
Another study demonstrated that both vitamins K1 and K2 reduced the risk of developing diabetes in a cohort of Dutch men and women. However, the stronger and more significant association occurred with K2 (in this case MK-7), which reduced the risk of Type 2 diabetes by 7% for each 10-microgram increase in intake (Beulens, et al 2010).
The European Prospective Investigation into Cancer and Nutrition (EPIC)-NL consists of the two Dutch contributions to the EPIC study, the Prospect-EPIC and MORGEN-EPIC cohorts. These cohorts were set up simultaneously in 1993–1997 and merged into one Dutch EPIC cohort. The Prospect-EPIC study includes 17,357 women aged 49–70 years living in Utrecht and vicinity. The MORGEN-EPIC cohort consists of 22,654 adults aged 21–64 years selected from random samples of the Dutch population in three Dutch towns. Intake of phylloquinone was 200 ± 98 micrograms/day and intake of menaquinones was 31 ± 7 micrograms/day in our study population. Vegetables contributed 78% of phylloquinone intake, whereas cheese contributed 53%, milk products 19%, and meat 17% of menaquinone intake. They found that both dietary phylloquinone and menaquinones intakes were associated with a reduced risk of type 2 diabetes. This association was linear inverse for menaquinones, whereas a significant risk reduction for phylloquinone was observed at higher intakes, in particular. This was the first study to investigate the relation between vitamin K intake and risk of type 2 diabetes. In summary, the findings of this study show that both phylloquinone and menaquinones intakes may be associated with a reduced risk of type 2 diabetes. (Every little bit helps)
Tip: in Europe, studies are limited to less than 350mcg of MK-7 and MK-4.
In a study of older adults at high risk for cardiovascular disease, the risk of developing Type 2 diabetes was reduced by 17% per 100 micrograms of K1 intake per day (Ibarrola-Jurado, et al, 2012). An analysis was done of the cross sectional and longitudinal associations between K1 intake and Type 2 diabetes in elderly subjects from the PREDIMED trial for 5.5 years. They found that dietary phylloquinone at baseline was significantly lower in subjects who developed type 2 diabetes during the study. And subjects who increased their intake of vitamin K during the 5 year follow up had a 51% reduced risk of incident diabetes, compared with subjects who decreased or did not change the amount of K1 intake.
Subsequently, an intervention trial in young male volunteers using menaquinone-4 (MK-4) at a dose of 90 mg/day for 1 week was performed. MK-4 increased the immunoreactive insulin (IRI) response in pre-existing vitamin K-deficient subjects (Shiraki, et al 2015).
Vitamin K intake has been associated with several components of Metabolic Syndrome (MetS) both in cross-sectional and longitudinal analyses.
In the longitudinal analyses, high menaquinone intakes were associated with a lower occurrence of MetS. The associations of menaquinones and vitamin K status are mainly driven by associations with triacylglycerol and waist circumference. Dam, (et al 2015), aimed to study whether the intake of K1 and K2 and vitamin K status are associated with MetS and its individual components. Data came from the Profiel study (Preservation of Function in Elderly), which studied two cohorts of women and men, aged 40-80 years. At follow up, 625 participants were still alive and phylloquinone/menaquinone intakes were measured. At baseline 34.5% had MetS and 35.7% had MetS at follow-up. The findings indicated that high menaquinone intakes were associated with a lower prevalence of MetS. At follow-up the highest levels of menaquinones intake were associated with a lower occurrence of MetS. K1 was not associated with MetS prevalence. Higher menaquinone intakes were associated with a lower occurrence of MetS and lower triglycerol concentrations. They concluded that a high intake of menaquinones and high vitamin K status are associated with a lower occurrence of MetS. In conclusion, high intakes of menaquinones and high vitamin K status were associated with a reduced occurrence of MetS.
Medications and vegetable oil that interfere with vitamin K and osteocalcin activation can contribute to diabetes causation. Both vegetable oils and medicines, such as statin and warfarin share, in part, a common mechanism to inhibit vitamin K2-dependent processes, which can be interpreted to lead to increased onset of CVD, DM, chronic kidney disease, bone fracture and even mental disorder (Raggi et al, 2005; Brault et al, 2014; Okuyama et al, 2016) Under diabetic conditions, glucose is not utilized efficiently as an energy source. Instead, hydrophilic ketone bodies, synthesized from fatty acids in mitochondria, are transported to the tissues and utilized as an energy source. Statins inhibit the synthesis of ketone bodies (Okuyama, et al, 2015).
MK7 intake improves diabetic neuropathy
An open label study of 30 patients with peripheral neuropathy were given Mk4 twice a day for eight weeks, and then followed up with for another eight weeks. By the end of eight weeks, patients with both moderate and severe neuropathy had reduced symptoms. The intensity of tingling and numbness was greatly reduced (Kulkarni et al, 2013). And an association between diabetic neuropathy and the inactive form of MGP suggests that uncarboxylated MGP may be used as a biomarker of sensitive neuropathy (Jeannin et al, 2020).
K1 not associated with any changes.
Kumar, et al 2010, assessed whether changes in ucOC are associated with changes in serum glucose or insulin concentrations in humans. They examined total osteocalcin, ucOC, glucose, and insulin concentrations in women who had been treated with 1 mg phylloquinone daily, for 1 year. They found that 6 and 12 months of phylloquinone administration produced a decrease of ≈200% in ucOC concentrations. However, despite the dramatic change in ucOC concentrations, glucose and insulin concentrations remained unchanged. In this study, phylloquinone administration in normal postmenopausal women did not alter fasting serum glucose or insulin concentrations despite significant (≈200%) changes in serum ucOC concentrations. This begs the question, “is it gender based, or gender based gut bacteria in play”?
The role of osteocalcin, linking bone to the pancreas, and glucose metabolism, has been an exciting discovery in recent years, and the research has just begun to explore the pathways by which osteocalcin functions (Neve et al, 2013; O'Connor & Durack, 2017). As osteocalcin is a vitamin K dependent protein, this research has also begun to explore the role of vitamin K in diabetes, with the idea that vitamin K supplements may improve symptoms in diabetes or reduce the risk of even developing diabetes. The early research findings point to vitamin K being a crucial and necessary “player” in the feedback loop between osteocalcin and insulin, and that vitamin K through osteocalcin may be one of the significant regulators of glucose or energy metabolism (Tsugawa & Shiraki, 2020). In fact, it now appears that “K” is actually serving to regulate it. This early research indicates that having enough vitamin K can significantly reduce the risk of acquiring diabetes.
A quote from Dr. Ferron,
"A better understanding of the function of osteocalcin could eventually lead to the development of therapies for type 2 diabetes and obesity that would target vitamin K or gamma-carboxylation in osteoblasts."
This article has focused on the vitamin K dependent protein, osteocalcin. There are other vitamin K dependent proteins, such as Matrix Gla Protein, osteoprotegerin, and Fetuin-A, among others, that are also associated with the status of diabetes that were beyond the scope of this article. It will be with great interest that we watch the research unfold on the contributions of vitamin K to diabetes. For example, a recent study indicated that inactive mGp in type 2 diabetes patients was associated with arterial stiffness (Sardana et al, 2017) and other cardiovascular events (Dalmeijer et al, 2013).
References
1970s
Okada Y, Taniguchi H, Schimada C. High concentration of GABA and high glutamate decarboxylase activity in rat pancreatic islets and human insulinoma. Science. 1976;194:620-622.
Poser JW, Price PA. A method for decarboxylation of gamma-carboxyglutamic acid in proteins:Properties of the decarboxylated gamma-carboxyglutamic acid protein from calf bone. J Biol Chem. 1979;254:431–436.
1980s
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: Insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419.
The steady-state basal plasma glucose and insulin concentrations are determined by their interaction in a feedback loop.
Kruse K, Kracht U. Evaluation of serum osteocalcin as an index of altered bone metabolism. Eur J Pediatr. 1986 Apr;145(1-2):27-33.
With the introduction of a radioimmunoassay for serum osteocalcin it was hoped that this test would provide a useful index of altered bone metabolism. Therefore serum osteocalcin was measured in 88 controls and 112 patients with disorders of calcium and phosphate metabolism, isolated elevation of alkaline serum phosphatase in the absence of disease, and children prone to osteopenia. Levels of osteocalcin was decreased in children with diabetes mellitus type I and in patients on glucocorticoid treatment, indicating decreased bone formation. It is concluded that the measurement of serum osteocalcin seems to be a reliable index of bone formation provided that the vitamin D status and renal function are normal.
Reid IR, Chapman, GE, Fraser TR, Davies AD, Surus AS, Meyer J, et al. Low serum osteocalcin levels in glucocorticoid-treated asthmatics. J Clin Endocrinol Metab. 1986 Feb;62(2):379-83.
Serum osteocalcin (OC) levels were measured in 19 asthmatic patients receiving long term glucocorticoid therapy and in age- and sex-matched asthmatic patients not receiving this treatment. In the glucocorticoid-treated patients, the mean OC level was approximately 50% less than that in the control group (P less than 0.001), and there was a direct correlation between serum OC and vitamin D3 levels (r = 0.71; P less than 0.001]. It is likely that the depression of serum OC in glucocorticoid-treated patients results from the reduction in the rate of bone formation induced by these hormones.
Plietschmann P, Schernthaner G, Woloszczuk W. Serum osteocalcin levels in diabetes mellitus: Analysis of the type of diabetes and microvascular complications. Diabetologis. 1988 Dec;31(12):892-5.
Recent studies indicate that serum levels of osteocalcin, a 49-amino acid bone matrix protein, are a biochemical marker of bone formation. In order to study bone metabolism in diabetes mellitus, in 28 patients with Type 1 (insulin-dependent) diabetes mellitus, in 38 patients with Type 2 (non-insulin-dependent) diabetes mellitus, and two control groups, matched for Type 1 and Type 2 diabetic patients, respectively, serum levels of osteocalcin, parathyroid hormone and 25 hydroxy vitamin D were measured by radioimmunoassay. Our data give evidence of a vitamin D deficiency and a decreased bone formation in patients with Type 2 diabetes mellitus. In Type 1 diabetes mellitus bone formation, as reflected by serum osteocalcin levels, was influenced by the presence or absence of microangiopathic complications.
Hauschka PV, Lian JB, Cole DE, Gundberg CM. Osteocalcin and matrix Gla protein: Vitamin K-dependent proteins in bone. Physiol Rev. 1989 Jul;69(3):990-1047.
Price P. A. Gla-containing proteins of bone. Connective Tissue Research. 1989;21(1–4):51–57.
Bone has high levels of two proteins which contain the vitamin K-dependent Ca2+ binding , gamma-carboxyglutamic acid (Gla). Bone Gla protein (BGP) or osteocalcin, is a 49 residue water soluble protein, and matrix Gla protein (MGP) is a 79 residue water insoluble protein. BGP is synthesized only by calcified tissues while MGP is synthesized by calcified tissues, cartilage, and all soft tissues tested.
1990s
Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15(4):827-832.
Taylor AK, Linkhart S, Mohan S, Christenson RA, Singer FR, Baylink DJ. Multiple osteocalcin fragments in human urine and serum as detected by a midmolecule osteocalcin radioimmunoassay. J Clin Endocrinol Metab. 1990;70:467-472.
Reliable markers of bone formation are essential to the investigation of metabolic bone disorders. Circulating levels of human osteocalcin (OC) can be used as an index of bone formation. A disadvantage of using serum OC as a marker of formation is its diurnal variation, so this study determined the usefulness of urine in the assessment of bone turnover. Z-Score analysis indicates that uOC (z = 14.04) is better able to distinguish between normal children with high bone turnover and normal adults.
Cairns J. R., Price P. A. Direct demonstration that the vitamin K-dependent bone Gla protein is incompletely γ-carboxylated in humans. Journal of Bone and Mineral Research. 1994;9(12):1989–1997.
Incomplete vitamin K-dependent gamma-carboxylation has been found in bone Gla protein (BGP).
Reddi K, Henderson B, Meghji S, Wilson M, Poole S, Hopper C, et al. Interleukin 6 production by lipopolysaccharide-stimulated human fibroblasts is potently inhibited by naphthoquinone (vitamin K) compounds. Cytokine. 1995;7(3):287–290.
Ducy P, Desbois C, Boyce B, Pinero G, Story B, Dunstan C, Smith E et al. Increased bone formation in osteocalcin deficient mice. Nature. 1996;382:448-452.
Vertebrates constantly remodel bone. The resorption of preexisting bone by osteoclasts and the formation of new bone by osteoblasts is strictly coordinated to maintain bone mass. The molecular determinants of osteoblast activity are unknown. To investigate the role of osteocalcin, we have generated osteocalcin-deficient mice. These mice develop a phenotype marked by higher bone mass and bones of improved functional quality. Studies done before and after ovariectomy showed that the absence of osteocalcin leads to an increase in bone formation without impairing bone resorption. To our knowledge, this study provides the first evidence that osteocalcin is a determinant of bone formation.
Lehto S, Niskanen L, Suhonen M, Ronnemaa T, Laakso M. Medial artery calcification. A neglected harbinger of cardiovascular complications in non-insulin-dependent diabetes mellitus. Arterioscler Thromb Vasc Biol. 1996;16:978–983.
This large population based study demonstrated that MAC is a powerful and hitherto largely unrecognized marker for future total and cardiovascular mortality in patients who are non-insulin dependent diabetic. They found that during the follow-up, MAC was a strong independent predictor of total cardiovascular and CHD mortality, and it was also a significant predictor of future CHD events (fatal or nonfatal myocardial infarction), stroke, and amputation. This relationship was observed regardless of glycemic control and known duration of NIDDM.
Niskanen L, Rauramaa R, Miettinen H, Haffner SM, Mercuri M, Usitupa M. Carotid artery intima-media thickness in elderly patients with NIDDM and in nondiabetic subjects. Stroke. 1996;27:1986-92.
The risk of atherosclerotic vascular disease is increased both in subjects with non–insulin-dependent diabetes mellitus (NIDDM) and in those with impaired glucose tolerance compared with nondiabetic subjects. The purpose of this study was to investigate the carotid intimal-medial thicknesses (IMTs) and their determinants in elderly patients with NIDDM and in control subjects. The patients were elderly. Common carotid and carotid bifurcation IMTs were greater in the NIDDM group than in control subjects (P<.05 to .01. Both diabetic status and the presence of clinical macrovascular disease contributed independently to carotid IMT. Carotid IMT was greater in NIDDM patients than in control subjects.
Koshihara Y., Hoshi K. Vitamin K2 enhances osteocalcin accumulation in the extracellular matrix of human osteoblasts in vitro. Journal of Bone and Mineral Research. 1997;12(3):431–438.
This study demonstrated that vitamin K2 promoted the carboxylation of osteocalcin production and mineralization by osteoblasts, even when treated with a ten times higher concentration of warfarin, which interferes with vitamin K. However the warfarin did produce artificial calcification in osteoblasts. Vitamin K2 (MK4) was recently developed as an osteoporosis medication that both enhances osteoblast function, as well as inhibits osteoclast function. As a medication it was more effective for patients with a high level of vitamin D3 in the blood.
Luo G, Ducy P, McKee MD, Pinero GJ, Loyer E, Behringer RR, Karsenty G. Spontaneous calcification of arteries and cartilage in mice lacking matrix Gla protein. Nature. 1997;386:78-81.
Calcification of the extracellular matrix (ECM) can be physiological or pathological. Physiological calcification occurs in bone when the soft ECM is converted into a rigid material capable of sustaining mechanical force; pathological calcification can occur in arteries and cartilage, and other soft tissues. This study looked for a molecular determinant that would regulate the extracellular matrix. One candidate is matrix GLA protein. Mice that lack Mgp, develop to term but die within two months as a result of arterial calcification which leads to blood vessel rupture. Mgp-deficient mice additionally exhibit inappropriate calcification of various cartilages, including the growth plate, which eventually leads to short stature, osteopenia and fractures. These results indicate that ECM calcification must be actively inhibited in soft tissues by matrix Gla Protein.
Vergnaud P, Garnero P, Meunier PJ, Bréart G, Kamihagi K, Delmas PD. Undercarboxylated osteocalcin measured with a specific immunoassay predicts hip fracture in elderly women:The EPIDOS study. Journal of Clinical Endocrinology and Metabolism. 1997;82(3):719–724.
Osteocalcin (OC) is a bone-specific protein of 49 amino acids that is released in blood and is widely used as a sensitive marker of bone formation. Increased levels of circulating undercarboxylated osteocalcin (ucOC) have been shown to predict hip fracture risk in a small group of elderly institutionalized women. This study utilized a new ELISA for serum ucOC to confirm these findings in a prospective cohort study (EPIDOS) of 7598 healthy, independently living women over 75 years of age. They found that increased levels of ucOC were associated with increased hip fracture risk. In contrast, total OC was not associated with hip fracture risk.
Boskey AL, Gadaleta S, Gundberg C, Doty SB, Ducy P, Karsenty G. Fourier transform infrared microspectroscopic analysis of bones of osteocalcin-deficient mice provides insight into the function of osteocalcin. Bone. 1998;23(3):187–96.
Osteocalcin has been postulated to play roles in bone formation and remodeling. Recently, genetic studies showed that osteocalcin acts as an inhibitor of osteoblast function. To test the hypothesis that osteocalcin is involved in regulating mineral properties, mineralization of osteocalcin-knockout mice was studied compared to wild-type mice at various ages. The data indicated that osteocalcin is required to stimulate bone mineral maturation.
Rosato MT, Schneider SH, Shapses SA. Bone turnover and insulin-like growth factor I levels increase after improved glycemic control in noninsulin-dependent diabetes mellitus. Calcif Tissue Int. 1998 Aug;63(2):107-11.
This study explored whether both bone resorption and formation are affected by glycemic control, and contribute to diabetic osteopenia. In this study, 20 patients with noninsulin-dependent diabetes mellitus and 20 healthy control subjects were examined at baseline and 2 months. The diabetic patients showed an improvement of glycemic control (decreased HbA1c) at the second measurement. These data suggest that improved glycemic control is accompanied by an increase in bone turnover for male and female diabetic patients, possibly mediated by increased levels of circulating IGF-I.
Sokoll LJ, Booth SL, Davidson KW, Dallal GE, Sadowski JA. Diurnal variation in total and undercarboxylated osteocalcin: Influence of increased dietary phylloquinone. Calcified Tissue International. 1998;62(5):447–52.
Ravn P, Cizza G, Bjarnason NH, et al. Low body mass index is an important risk factor for low bone mass and increased bone loss in early postmenopausal women. Journal of Bone and Mineral Research. 1999;14(9):1622–27.
Inaba M, Nishizawa Y, Mita K, et al. Poor glycemic control impairs the response of biochemical parameters of bone formation and resorption to exogenous 1,25-dihydroxyvitamin D3 in patients with type 2 diabetes. Osteoporosis International. 1999;9(6):525–31.
Osteoblast deficit plays a principal role in the development of diabetic osteopenia. This study was performed to assess the sensitivity of osteoblasts to vitamin D3 in patients with type 2 diabetes without insulin deficiency or overt diabetic complications. During stimulation with vitamin D3 at 2.0 micrograms/day for 6 consecutive days in 9 type-2 diabetic patients, serum levels of bone alkaline phosphatase (BALP), osteocalcin (OC) and the carboxyterminal propeptide of type 1 procollagen, and the urinary excretion of pyridinoline and deoxypyridinoline (DPYR), were monitored. The findings would indicate that poor glycemic control impairs the responses of osteoblasts and osteoclasts to vitamin D3 in normo-insulinemic type 2 diabetic patients.
Marchais SJ , Metivier F, Guerin AP, London GM. Association of hyperphosphataemia with haemodynamic disturbances in end-stage renal disease. Nephrol Dial Transplant.1999;14:2178–83.
Price PA, Faus SA, Williamson MK/ Warfarin causes rapid calcification of the elastic lamellae in rat arteries and heart valves. Arterioscler Thromb Vasc Biol. 1998, 18(9):1400-1407.
High doses of warfarin cause calcification in the media of major arteries and in aortic heart valves in the rat. Aortic calcification was first seen after 2 weeks of warfarin treatment and progressively increased in density at 3, 4, and 5 weeks of treatment. By 5 weeks, the calcification of major arteries could be seen on radiographs and by visual inspection of the artery. The calcification of arteries induced by warfarin is similar to that seen in the matrix Gla protein (MGP)–deficient mouse, which suggests that warfarin induces artery calcification by inhibiting γ-carboxylation of MGP and thereby inactivating the putative calcification-inhibitory activity of the protein. Warfarin treatment markedly increased the levels of MGP mRNA and protein in calcifying arteries and decreased the level of MGP in serum. The results indicate that the improved warfarin plus vitamin K treatment protocol developed in this study should provide a useful model to investigate the role of MGP in preventing calcification of arteries and heart valves.
Sakamoto N, Nishiike T, Iguchi H, Sakamoto K. Relationship between acute insulin response and vitamin K intake in healthy young male volunteers. Diabetes Nutrition and Metabolism. 1999;12:37-41.
To evaluate the effects of vitamin K on acute insulin response, 25 healthy young male volunteers were given an oral load of 75 g of glucose, and their mean daily vitamin K intake was estimated by a one-week food check list. After excluding low (<20) and high (> or =25) body mass index (BMI) subjects, the remaining 16 participants were divided into three semi-equal groups according to VK intake. Blood vitamin K status of the low vitamin K intake group tended to be poorer than that of the high intake group but fasting plasma glucose status was not markedly different between both groups. These results suggested that VK may play an important role on the acute insulin response in glucose tolerance.
Sakamoto N, Wakabayashi I, Sakamoto K. Low vitamin K intake effects on glucose tolerance in rats. Int J Vitam Nutr Res. 1999;69:27–31.
This study investigated the effects of vitamin K (VK) on pancreatic function, performing IV glucose tolerance tests on rats fed a high or low vitamin K diet (less than 20% of required K1). Plasma glucose and immuno-reactive insulin (IRI) were determined. The results indicated that low dietary vitamin K appeared to induce a tendency of poor early insulin response, and late hyperinsulinemia to the glucose load in rats.
Yoon JW, Yoon CS, Lim HW, Huang QQ, Kang Y, Pyun KH, et al. Control of autoimmune diabetes in NOD mice by GAD expression or suppression in beta cells. Science. 1999;284:1183-87.
Glutamic acid decarboxylase (GAD) is a pancreatic beta cell autoantigen in humans and nonobese diabetic (NOD) mice. Beta Cell-specific suppression of GAD expression has been found to prevent the development of autoimmune diabetes, whereas persistent GAD expression in the beta cells in the other four lines of antisense GAD transgenic NOD mice resulted in diabetes. Complete suppression of beta cell GAD expression blocked the generation of diabetogenic T cells and protected islet grafts from autoimmune injury. Thus modulation of GAD might have therapeutic value in type 1 diabetes.
2000s
Abramsen B, Rohold A, Henriksen JE, Beck-Nielsen H. Correlations between insulin sensitivity and bone mineral density in non-diabetic men. Diabetic Med. 2000;17:124-29.
This study investigated the relationships between bone mineral density (BMD), insulin secretion and insulin sensitivity, controlling for body. Type 2 diabetes is associated with bone mineral density, while patients with Type 1 diabetes have normal or low bone mineral density. The results suggest that obesity may induce insulin resistance, leading to increases in bone mass. It is hypothesized that patients with insulin resistance in the metabolic pathway do not exhibit resistance to the skeletal actions of insulin.
Goff DC, D’Agostino RB, Haffner SM, Saad MF, Wagenknecht LE. Lipoprotein concentrations and carotid atherosclerosis by diabetes status: Results from the insulin resistance atherosclerosis study. Diabetes Care. 2000;23:1006-11.
Lipoprotein concentrations are associated with the development of atherosclerosis in people with and without diabetes. The associations between lipoprotein concentrations and internal and common carotid artery intimal-medial thickness (IMT) were examined by diabetes status in a cross-sectional analysis among 1,391 participants in the Insulin Resistance Atherosclerosis Study. Participants included 442 individuals with type 2 diabetes, 308 with impaired glucose tolerance, and 641 with normal glucose tolerance. The results support the importance of dyslipidemia as a major risk factor for atherosclerosis in people with diabetes.
Lejeunesse D, Delalandre A, Guggino SE. Thiazide diurectics affect osteocalcin production in human osteoblasts at the transcription level without affecting vitamin D3 receptors. J Bone Miner Res. 2000 May;15(5):894-901.
Sakamoto N, Nishiike T, Iguchi H, Sakamoto K. Possible effects of one week vitamin K (menaquinone-4) tablets intake on glucose tolerance in healthy young male volunteers with different descarboxy prothrombin levels. Clin Nutr. 2000;19:259–63.
To clarify the roles of vitamin K (VK) in the pancreas, oral glucose tolerance tests were examined in 12 healthy young male volunteers before and after one week of vitamin K tablet intake. They then took VK tablets (90 mg/d of MK4) for 1 week, and the second glucose tolerance test was examined. One week of VK intake tended to decrease the plasma DP levels of all groups and significantly reduced IRI. These results suggested that there may be some relationship between pharmacological dose of vitamin K and insulin response.
Seyama Y, Shinzi K, Yasuhiro M, Masako H. Mikio H, Eiji U, et al. Comparative effective of vitamin K2 and estradiol on experimental arteriosclerosis with diabetes mellitus. International Journal for Vitamin and Nutrition Research. 2000;70:301-304.
In order to further investigate the radical scavenging and anti-arteriosclerotic activities of vitamin K2 and estradiol, the comparative effects of vitamin K2 and estradiol on aortic calcium (Ca) and inorganic phosphorus (P) levels in the aorta and the elastin fraction were investigated in male rats after arteriosclerosis with diabetes was induced. Pharmacological doses of vitamin K2 (100 mg/kg b.w.) and medical dose of estradiol (83 mug/kg b.w.) suppressed the increased serum glucose and vitamin K2 and estradiol increased the decrease in serum insulin. Morever vitamin K2 and estradiol inhibited the increase of Ca and P in the aorta and the elastin from vitamin K2 and estradiol decreased the increased in serum lipid peroxide. It is suggested that both the pharmacological dose of vitamin K2 and the medical dose of estradiol suppressed the development of arteriosclerosis associates with diabetes.
Erkelens DW, Insulin resistance syndrome and type 2 diabetes mellitus. Am J Cardiol. 2001 Oct 11;88(uB):38J-42J.
Patients with type 2 diabetes mellitus have an elevated risk of morbidity and mortality from cardiovascular disease. This risk is partly attributable to an increased prevalence of classic coronary artery disease risk factors and partly because of hyperglycemia itself. In most cases, diabetic dyslipidemia is preceded by hyperinsulinemia resulting from insulin resistance. Furthermore, in large-scale clinical trials (eg, Scandinavian Simvastatin Survival Study [4S] and the Cholesterol and Recurrent Events [CARE] study), it has been demonstrated that lipid lowering can appreciably reduce cardiovascular events in diabetic patients.
Isomaa B , Almgren P , Tuomi T , Forsen B, Lahti K, et al.. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001;24:683–89.
This study aimed to estimate the prevalence of and the cardiovascular risk associated with the metabolic syndrome using the new definition proposed by the World Health Organization (WHO). 4,483 subjects aged 35–70 years participating in a large family study of type 2 diabetes in Finland and Sweden (the Botnia study) were included in the analysis of cardiovascular risk associated with the metabolic syndrome. In women and men, respectively, the metabolic syndrome was seen in 10 and 15% of subjects who were insulin resistant, 42 and 64% of those with impaired fasting or impaired glucose tolerance, and 78 and 84% of those with type 2 diabetes. The risk for heart disease and stroke increased threefold in subjects with metabolic syndrome.
Yamauchi T, Kamon J, Waki H, Terauchi Y, Kubota N, Hara K, et al. The fat-derived hormone adiponectin reverses insulin resistance associated with both lipoatrophy and obesity. Nature Medicine. 2001;7:941-46.
Adiponectin is an adipocyte (fat)-derived hormone. Recent genome-wide scans have mapped a susceptibility locus for type 2 diabetes and metabolic syndrome to chromosome 3q27, where the gene encoding adiponectin is located. Here we show that decreased expression of adiponectin correlates with insulin resistance in mouse models of altered insulin sensitivity. Adiponectin decreases insulin resistance by decreasing triglyceride content in muscle and liver in obese mice. Moreover, insulin resistance in lipoatrophic mice was completely reversed by the combination of physiological doses of adiponectin and leptin, but only partially by either adiponectin or leptin alone. We conclude that decreased adiponectin is implicated in the development of insulin resistance in mouse models of both obesity and lipoatrophy. These data also indicate that the replenishment of adiponectin might provide a novel treatment modality for insulin resistance and type 2 diabetes.
Yang WS, Lee WJ, Funahashi T, Tanaka S, Matsuzawa Y, Chao CL, et al. Weight reduction increases plasma levels of an adipose-derived anti-inflammatory protein, adiponectin. Journal of Clinical Endocrinology and Metabolism. 2001;86:3815–19.
Adiponectin, an adipose tissue-specific plasma protein, was recently revealed to have anti-inflammatory effects on the cellular components of vascular wall. Its plasma levels were significantly lower in men than in women and lower in human subjects with obesity, type 2 diabetes mellitus, or coronary artery disease. In this study, we observed the changes of plasma adiponectin levels with body weight reduction among 22 obese patients who received gastric partition surgery. A 46% increase of mean plasma adiponectin level was accompanied by a 21% reduction in mean body mass index. The change in plasma adiponectin levels was significantly correlated with the changes in body mass index, and hip circumferences, and steady state plasma glucose levels. In conclusion, body weight reduction increased the plasma levels of a protective adipocytokine, adiponectin.
Kendall, D.M.; Harmel, A.P. The metabolic syndrome, type 2 diabetes, and cardiovascular disease:Understanding the role of insulin resistance. Am. J. Manag. Care 2002;8:S635–S653.
Lakka HM , Laaksonen DE , Lakka TA , et al.. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002;288:2709–16.
The metabolic syndrome, a concurrence of disturbed glucose and insulin metabolism, overweight and abdominal fat distribution, mild dyslipidemia, and hypertension, is associated with the development of type 2 diabetes mellitus and cardiovascular disease (CVD). This study assessed the association of the metabolic syndrome with cardiovascular and overall mortality, using participants from the Kuopio Ischaemic Heart Disease Risk Factor Study, a population-based, prospective cohort study of 1209 Finnish men aged 42 to 60 years at baseline (1984-1989) who were initially without CVD, cancer, or diabetes. The results indicated that men with the metabolic syndrome were 2.9 times more likely to die of CHD after adjustment for conventional cardiovascular risk factors.
Libby, Ridker, Maseri. Inflammation and atherosclerosis. Circulation. 2002 Mar 5;105(9):1135-43.
Atherosclerosis, formerly considered a bland lipid storage disease, actually involves an ongoing inflammatory response. Recent advances in basic science have established a fundamental role for inflammation in mediating all stages of this disease from initiation through progression. Elevation in markers of inflammation predicts outcomes of patients with acute coronary syndromes, independently of myocardial damage. In addition, low-grade chronic inflammation, as indicated by levels of the inflammatory marker C-reactive protein, prospectively defines risk of atherosclerotic complications. These new insights into inflammation in atherosclerosis have practical clinical applications in targeting of therapy for this scourge of worldwide importance.
Atkin O, Gol K, Akturk M, Erkaya S. Evaluation of bone turnover in postmenopausal patients with type 2 diabetes mellitus using biochemical markers and bone mineral density measurements. Gynecol Endocrinol. 2003 Feb;17(1):19-29.
Although osteoporosis is reported as a potential complication of type 1 diabetes mellitus (DM), the effects of type 2 Diabetes on bone mass are conflicting. Most of the studies conducted in recent years reveal that bone mineral density (BMD) values of type 2 DM patients are not decreased and even increased when compared with healthy control groups. In this study we evaluated bone turnover in 57 postmenopausal type 2 DM patients. We found that BMD values in diabetic patients for lumbar region, were higher than healthy postmenopausal control group. Our findings suggested that the bone turnover rate is remarkably lower in type 2 DM patients compared to healthy postmenopausal patients.
Koshihara Y, Hoshi K, Okawara R, Ishibashi I, Yamamoto S. Vitamin K stimulates osteoblastogenesis and inhibits osteoclastogenesis in human bone marrow cell culture. J Endocrinol. 2003 Mar;176(3):339-48.
Accumulating evidence indicates that menaquinone-4 (MK-4), a vitamin K2, inhibits the development of osteoclasts in murine bone marrow culture. In clinical practice, MK4 treatment has been successful in inhibiting the occurrence of new bone fractures and increased carboxylation of osteocalcin. To clarify the inhibitory mechanism, we investigated the differentiation of colony forming-unit fibroblasts (CFU-Fs) and osteoclasts in human bone marrow culture. They found that both types of vitamin K1, and K2 promoted the development of osteoblasts and inhibited osteoclast formation in human bone marrow.
London GM , Guerin AP , Marchais SJ , Metivier F , Pannier B , Adda H. Arterial media calcification in end-stage renal disease: Impact on all-cause and cardiovascular mortality. Nephrol Dial Transplant. 2003;18:1731–40.
Studies on end-stage renal disease patients showed that arterial calcifications are associated with cardiovascular (CV) morbidity and are an independent predictor of all-cause and CV mortality. This study investigated the prognostic value of arterial medial calcification (AMC) in relationship to all-cause or CV mortality for stable haemodialysis (HD) patients. They found that arterial medical calcification is a strong prognostic marker of all-cause and CV mortality in HD patients. The principal effect of AMC on arterial function is increased arterial stiffness.
Lu, H, Kraut D, Gerstenfeld LC, Graves DT. Diabetes interferes with the bone formation by affecting the expression of transcription factors that regulate osteoblast differentiation. Endocrinology. 2003 Jan;144(1):346-52.
Type 1 diabetes in humans has a complication of inadequate bone formation, resulting in osteopenia and delayed fracture healing. This was investigated with mice who were made diabetic. Insulin treatment substantially reversed the effect of diabetes on the expression of bone matrix osteocalcin and collagen type 1 and transcription factors Cbfa1/Runx2 and Dlx5. These results indicate that diabetic animals produce sufficient amounts of immature mesenchymal tissue but fail to adequately express genes that regulate osteoblast differentiation, which in turn, leads to decreased bone formation.
Yet GY, Eisenberg DM, Kaptchuk TJ, Phillips RS. Systematic review of herbs and dietary supplements for glycemic control in diabetes. Database of Abstracts of Reviews of Effects (DARE): Quality-assessed Reviews. 2003. The aetiology of vitamin K deficiency in haemodialysis is multifactorial, including deficient intake, uraemic inhibition of the vitamin K cycle and possibly interference of vitamin K absorption by phosphate binders.
Giachelli CM. Vascular calcification mechanisms. J Am Soc Nephrol. 2004;15:2959-64.
Vascular calcification is highly correlated with cardiovascular disease mortality, especially in patients with End Stage Renal Disease or diabetes. Vascular calcification is now recognized as a marker of atherosclerotic plaque burden as well as a major contributor to loss of arterial compliance and increased pulse pressure seen with age, diabetes, and renal insufficiency.
Hu G, Qiao Q, Tuomilehto J, Baldau B, Borch-Johnsen K, Pyorala K. Prevalence of the metabolic syndrome and its relation to all-cause and cardiovascular mortality in nondiabetic European men and women. Arch Intern Med. 2004;164:1066-1076.
This study examined the age and sex specific prevalence of the metabolic syndrome and its association with all-cause and cardiovascular mortality in nondiabetic European men and women. The study was based on 11 prospective European cohort studies comprising 6156 men and 5356 women without diabetes and aged from 30 to 89 years, and had a median follow-up of 8.8 years. The age standardized prevalence of the metabolic syndrom was slightly higher in men (15.7%) than in women (14.2%). Of the 1119 deaths recorded during follow up, 432 were caused by cardiovascular disease. The overall prevalence of the metabolic syndrome in nondiabetic adult Europeans is 15%. Nondiabetic persons with the metabolic syndrome have an increased risk of death from all causes as well as cardiovascular disease.
Malik S, Wong ND, Franklin SS, et al. Impact of the metabolic syndrome on mortality from coronary heart disease, cardiovascular disease, and all causes in United States adults. Circulation. 2004;110:2345-50.
We examined the impact of the Metabolic Syndrome (MetS) on Coronary Heart Disease, Coronary Vascular Disease, and overall mortality among US adults. In a prospective cohort study, 6255 subjects 30 to 75 years of age (54% female) (representative of 64 million adults in the United States) from the Second National Health and Nutrition Examination Survey were followed for a mean+/-SD of 13.3+/-3.8 years. In persons with MetS but without diabetes, risks of CHD and CVD mortality remained elevated. Diabetes predicted all mortality end points. Those with even 1 to 2 MetS risk factors were at increased risk for mortality from CHD and CVD.
Murshed M, Schinke T, McKee Md & Karsenty G. Extracellular matrix mineralization is regulated locally: Different roles of two gla-containing proteins. The J of Cell Biol. 2004;165:625-30.
Extracellular matrix mineralization (ECMM) is a physiologic process in the skeleton and in teeth and a pathologic one in other organs, where it must be inhibited. Some proteins that inhibit ECMM have been identified, including Matrix gla Protein (MGP) and fetuin. The molecular mechanisms controlling ECMM are poorly understood, including whether they are secreted locally, or whether they act systemically via circulation. This study used mouse models to determine that restoration of Mgp expression in arteries rescues the arterial mineralization phenotype of Mgp-/- mice, whereas its expression in osteoblasts prevents bone mineralization. Having enough vitamin K in order to carboxylate the MGP was important. These results indicate that ECMM is regulated locally in animals.
Papakitsou EF, Margioris AN, Dretakis KE, et al. Body mass index (BMI) and parameters of bone formation and resorption in postmenopausal women. Maturitas. 2004;47(3):185–93.
The aim of this study was to evaluate increased body mass index (BMI) as a factor predisposing to lower rates of bone turnover or changes in bone balance after menopause. They concluded that in postmenopausal women, increased body weight may have different effects on mature estrogen-deficient bone and extraskeletal tissues containing collagen I.
Wajih N, Borras T, Xue W, Hutson SM, Wallin R. Processing and transport of matrix gamma-carboxyglutamic acid protein and bone morphogenetic protein-2 in cultured human vascular smooth muscle cells: Evidence for an uptake mechanism for serum fetuin. J Biol Chem. 2004;279(41):43052-60.
Matrix gamma-carboxyglutamic acid protein (MGP) is a member of the vitamin K-dependent protein family with unique structural and physical properties. MGP has been shown to be an inhibitor of arterial wall and cartilage calcification. One inhibitory mechanism is thought to be binding of bone morphogenetic protein-2, which has been shown to be dependent upon having enough vitamin K, in order to carboxylate MGP. Evidence is presented for fetuin by cultured human VSMCs. Fetuin uptake and secretion by cells at sites of calcification in the arterial wall may represent an additional protective mechanism against arterial calcification.
Achemlal L, Tellal S, and Rkiouak F, Bone metabolism in male patients with type 2 diabetes. Clinical Rheumatology. 2005;24(5):493–96.
Studies suggest that poor glycaemic control in type 2 diabetes may contribute to osteopaenia. The aim of this study was to investigate biochemical markers of bone turnover in males with poorly controlled type 2 diabetes. The patients were receiving oral hypoglycaemic agents (metformin or sulphonylureas or both). The mean age of the study population was 53.7 (10.3) years, and the mean disease duration was 8.6 years (range: 6.5–10.7). The results indicated that patients had significantly lower serum levels of osteocalcin than controls. Our study suggested that bone formation is altered in type 2 diabetes and that bone turnover is affected by glycaemic control status.
Gerdhem P, Isaksson A, Åkesson K., Obrant KJ. Increased bone density and decreased bone turnover, but no evident alteration of fracture susceptibility in elderly women with diabetes mellitus. Osteoporosis International. 2005;16(12):1506–12.
Bone density, bone turnover and fracture susceptibility were evaluated in 1,132 randomly recruited women, all 75 years old. Seventy-four of the women had diabetes, while 1,058 women did not. Women with diabetes had no more lifetime fractures (52%) than women without diabetic disease (57%), (p=0.31). This study shows that elderly women with diabetes and without severe renal insufficiency have high bone mass and low bone turnover, which is not likely to have a strong influence on fracture susceptibility.
Raggi P, Cooil B, Ratti C, Callister TQ, Budoff M. Progression of coronary artery calcium and occurrence of myocardial infarction in patients with and without diabetes mellitus. Hypertension. 2005;46(1):238-43. 
In a retrospective study, we examined 1153 nondiabetic and 157 diabetic subjects to assess progression of coronary calcium. A yearly score increase >15% was considered evidence of true progression. The use of statins and occurrence of myocardial infarction were recorded. There was no difference in baseline calcium score between diabetic and nondiabetic patients. Diabetic patients with no coronary calcium on the baseline scans developed it more often than nondiabetic subjects (42% versus 25%; P=0.046) during follow-up. Calcium progression was 33% greater in diabetic patients than nondiabetic subjects (P<0.001) if no statin therapy was provided and 17.7% greater when statins were used (P<0.001). Among the 49 subjects who experienced a myocardial infarction, the calcium score increased on average 20% more in diabetic than nondiabetic patients (P<0.001). These findings support the notion that diabetes mellitus causes accelerated atherosclerosis, despite the use of statin therapy, and provide evidence that coronary calcium monitoring is an effective method to assess treatment efficacy.
Wilson PW, D’Agostino RB, Parise H, Sullivan L, Meigs JB. Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation. 2005;112(20):3066 –72.
The objective was to investigate risk for CVD, CHD, and T2diabetes according to metabolic syndrome traits. The study followed a cohort of 3323 middle-aged adults for the development of new CVD, CHD and T2Diabetes over an 8 year period. In persons without CVD or T2DM at baseline, the prevalence of metabolic syndrome was 26.8% in men and 16.6% in women. The data indicated that metabolic syndrome is common and is associated with an increased risk for CVD and T2DM in both sexes. The metabolic syndrome accounts for up to one third of CVD in men and approximately half of new T2dm over 8 years of follow up. . .
Dobnig H, Piswanger-Sölkner JC, Roth M. Type 2 diabetes mellitus in nursing home patients: Effects on bone turnover, bone mass, and fracture risk. Journal of Clinical Endocrinology and Metabolism. 2006;91(9):3355–63.
The objective of this study was to investigate whether type 2 diabetes affects bone mass, bone turnover, or prospective fracture rates in frail, elderly women living in nursing homes in Austria. Patients were followed over 2 years. A total of 110 hip fractures occurred during the observation period, corresponding to a hip fracture rate of 3.1% in the control group and 3.4% in the group with Type 2 diabetes, per 100 patient years; this was not a significant difference for the two groups. The results indicated that decreased PTH levels and higher levels of glycemia independently contribute to lower bone turnover in elderly nursing home patients with type 2 DM. Despite higher bone mass and lower bone turnover, hip fracture risk is comparable with women without DM.
Lee NK , Sowa H , Hinoi E , et al.. Endocrine regulation of energy metabolism by the skeleton. Cell. 2007;130:456–69.
The regulation of bone remodeling by an adipocyte-derived hormone implies that bone may exert a feedback control of energy homeostasis. We show here that mice lacking the protein tyrosine phosphatase OST-PTP are hypoglycemic and are protected from obesity and glucose intolerance because of an increase in beta-cell proliferation, insulin secretion, and insulin sensitivity. In contrast, mice lacking the osteoblast-secreted molecule osteocalcin display decreased beta-cell proliferation, glucose intolerance, and insulin resistance. By revealing that the skeleton exerts an endocrine regulation of sugar homeostasis, this study expands the biological importance of this organ and our understanding of energy metabolism.
Schurgers LJ, Teunissen KJ, Knapen MH, Kwaijtaal M, van Diest R, Appels A, et al. Novel conformation-specific antibodies against matrix gamma-carboxyglutamic acid (Gla) protein: Undercarboxylated matrix Gla protein as marker for vascular calcification. Arterioscler Thromb Vasc Biol. 2005;25(8):1629-33.
Matrix Gla Protein is a vitamin K dependent protein, that is a potent inhibitor of arterial calcification. This study showed that uncarboxylated MGP (ucMGP) is strongly associated with intimal and medial vascular calcification, and suggested the essentiality of vitamin K to carboxylate MGP, so that it can inhibit ectopic calcification.
Stafford D W. The vitamin K cycle. J Thromb Haemost. 2005;3:1873-78.
Johnson RC, Leopold JA, Loscalzo J. Vascular calcification: pathobiological mechanisms and clinical implications. Circ Res . 2006;99(10):1044-59.
It now appears that vascular calcification is a consequence of tightly regulated processes that culminate in organized extracellular matrix deposition by osteoblast like cells. The normal balance between promotion and inhibition of calcification becomes dysregulated in chronic kidney disease, diabetes, atherosclerosis, and as a consequence of aging. At the molecular level, new insights into the factors regulating mineralization provide greater appreciation of its complexity.
Karsenty G. Convergence between bone and energy homeostases: Leptin regulation of bone mass. Cell Metabolism. 2006;4:341-8.
The observation that obesity protects from osteoporosis suggested that energy metabolism and bone mass could be regulated by the same hormones. This review summarizes the genetic and molecular bases of this regulation and discusses its potential clinical implications.
Abdul-Ghani MA, Matsuda M, Balas B, DeFronzo R. Muscle and liver insulin resistance indexes derived from the oral glucose tolerance test. Diabetes Care. 2007;30:89–94.
Cutrim DM, Pereira FA, de Paula FJ, Foss MC. Lack of relationship between glycemic control and bone mineral density in Type 2 diabetes mellitus. Braz J Med Biol Res. 2007 Feb;40(2):221-7.
We assessed the effect of chronic hyperglycemia on bone mineral density (BMD) and bone remodeling in patients with type 2 diabetes mellitus. We investigated 42 patients with type 2 diabetes under stable control for at least 1 year, 22 of them with good metabolic control, and 20 with poor metabolic control, and 24 normal control individuals. The present results demonstrate that hyperglycemia is not associated with increased bone resorption in type 2 diabetes mellitus and that BMD is not altered in type 2 diabetes mellitus.
Fulzele K, DiGirolamo DJ, Liu Z, Xu J, Messina JL, Clemens TL. Disruption of the insulin-like growth factor type 1 receptor in osteoblasts enhances insulin signaling and action. The Journal of Biological Chemistry. 2007;282(35):25649–58.
Kronmal RA, McClelland RL, Detrano R, Shea S, Lima JA, Cushman M, et al. Risk factors for the progression of coronary artery calcification in asymptomatic subjects: Results from the Multi-Ethnic Study of Atherosclerosis (MESA). Circulation. 2007;115(21):2722-30.
The Multi-Ethnic Study of Atherosclerosis (MESA) provides an opportunity to study the association of traditional cardiovascular risk factors with the incidence and progression of coronary artery calcium (CAC) in a large community-based cohort with no evidence of clinical cardiovascular disease. This is the first large multi-ethnic study reporting on the incidence and progression of CAC. Standard coronary risk factors were generally related to both CAC incidence and progression. Whites had more incident CAC and CAC progression than the other 3 racial/ethnic groups. Except for diabetes mellitus, risk factor relationships were similar across racial/ethnic groups.
Lee NK, Sowa H, Hinoi E, Ferron M, Ahn JD, et al. Endocrine regulation of energy metabolism by the skeleton. Cell. 2007;130(3):456-69.
The regulation of bone remodeling by an adipocyte-derived hormone implies that bone may exert a feedback control of energy homeostasis. To test this hypothesis theylooked for genes expressed in osteoblasts, encoding signaling molecules and affecting energy metabolism. We show here that mice lacking the protein tyrosine phosphatase OST-PTP are hypoglycemic and are protected from obesity and glucose intolerance because of an increase in beta-cell proliferation, insulin secretion, and insulin sensitivity. In contrast, mice lacking the osteoblast-secreted molecule osteocalcin display decreased beta-cell proliferation, glucose intolerance, and insulin resistance. Removing one Osteocalcin allele from OST-PTP-deficient mice corrects their metabolic phenotype. Ex vivo, osteocalcin can stimulate CyclinD1 and Insulin expression in beta-cells and Adiponectin, an insulin-sensitizing adipokine, in adipocytes; in vivo osteocalcin can improve glucose tolerance. By revealing that the skeleton exerts an endocrine regulation of sugar homeostasis this study expands the biological importance of this organ and our understanding of energy metabolism.
McCabe L. R. Understanding the pathology and mechanisms of type I diabetic bone loss. Journal of Cellular Biochemistry. 2007;102(6):1343–57.
Type I (T1) diabetes, also called insulin dependent diabetes mellitus (IDDM), is characterized by little or no insulin production and hyperglycemia. One of the less well known complications of T1-diabetes is bone loss which occurs in humans and animal models. Exact mechanisms accounting for T1-diabetic bone loss are not known. Existing data indicate that the bone defect in T1-diabetes is anabolic rather than catabolic, suggesting that anabolic therapeutics may be more effective in preventing bone loss. Differences between T1-diabetic- and age-associated bone loss underlie the importance of condition specific, individualized treatments for osteoporosis.
Schurgers LJ, Spronk HM, Skepper JN, Hackeng TM, Shanahan CM, Vermeer C, et al. Post-translational modifications regulate matrix Gla protein function: Importance for inhibition of vascular smooth muscle cell calcification. J Thromb Haemost. 2007, 5(12):2503-11.
Schurgers LJ, Spronk HM, Soute BA, Schiffers PM, DeMey JG, Vermeer C: Regression of warfarin-induced medial elastocalcinosis by high intake of vitamin K in rats. Blood. 2007, 109(7):2823-31.
Wu KK, Huan Y. Diabetic atherosclerosis mouse models. Atherosclerosis. 2007 Apr;191(2):241-9.
Coronary heart disease due to atherosclerosis is the leading cause of death in the USA and accelerated CHD has emerged as a leading cause of morbidity and mortality in diabetic patients worldwide. In the past decade, several diabetic atherosclerosis mouse models have been established. This review focused on common diabetic atherosclerosis mouse models with respect to developing tools for studying the mechanisms of diabetes-accelerated atherosclerosis and evaluating therapeutic options.
Cranenburg EC, Vermeer C, Koos R, Boumans ML, Hackeng TM, Bouwman FG, et al. The circulating inactive form of matrix Gla Protein (ucMGP) as a biomarker for cardiovascular calcification. J Vasc Res. 2008, 45(5):427-36.
Matrix gamma-carboxyglutamate (Gla) protein (MGP) is a vitamin K-dependent protein and a strong inhibitor of vascular calcification. Vitamin K deficiency leads to inactive uncarboxylated MGP (ucMGP), which accumulates at sites of arterial calcification. We hypothesized that as a result of ucMGP deposition around arterial calcification, the circulating fraction of ucMGP is decreased. Here we report on the development of an ucMGP assay and the potential diagnostic utility of monitoring serum ucMGP levels.
Ferron M., Hinoi E., Karsenty G., Ducy P. Osteocalcin differentially regulates β cell and adipocyte gene expression and affects the development of metabolic diseases in wild-type mice. Proceedings ofthe National Academy of Sciences of the United States of America. 2008;105(13):5266–70.
Osteocalcin behaves as a hormone, regulating glucose metabolism and fat mass in two mutant mouse strains. In these mouse models, osteocalcin can increase beta cell proliferation, stimulate insulin expression and secretion, enhance energy expenditure and increase expression of adiponectin, an insulin sensitizing hormone produced by adipocytes. This study looked at wild type (WT) and the results indicated that osteocalcin acts directly on beta cells in culture, and likely in vivo. It appears that osteocalcin acts in (WT) mice to improve glucose handling and reduce fat mass and as a result can reduce the severity of obesity and type 2 diabetes. These results establish in WT mice the importance of this novel molecular player in the regulation of glucose metabolism and fat mass and suggest that osteocalcin may be of value in the treatment of metabolic diseases.
Ford ES, Schulze MB, Pischon T, Bergmann MM, Joost HG, Boeing H. Metabolic syndrome and risk of incident diabetes: Findings from the European Prospective Investigation into Cancer and Nutrition- Potsdam Study. Cardiovasc Diabetol. 2008;7:35.
We used data for 2796 men and women aged 35-65 years from the European Prospective Investigation into Cancer and Nutrition-Potsdam Study, followed for an average of 6.9 years to look at the relationship between metabolic syndrome and incident diabetes. Of the five components of metabolic syndrome, abdominal obesity and hyperglycemia were most strongly associated with incident diabetes.
Guzman RJ, Brinkley DM, Schumacher PM, Donahue RM, Beavers H, Qin X: Tibial artery calcification as a marker of amputation risk in patients with peripheral arterial disease. J Am Coll Cardiol. 2008, 51(20):1967-74.
Hinoi E, Gao N, Jung DY, et al. The sympathetic tone mediates leptin’s inhibition of insulin secretion by modulating osteocalcin bioactivity. Journal of Cell Biology. 2008;183(7):1235–42.
The skeleton acts as an endocrine regulator of energy metabolism through osteocalcin, that favors insulin secretion by Beta cells, insulin sensitivity in fat, liver, and muscle, and energy expenditure. The osteoblast-secreted molecule osteocalcin favors insulin secretion, but how this function is regulated in vivo by extracellular signals is unknown. In this study, we show that leptin, which inhibits insulin secretion, partly uses the sympathetic nervous system to fulfill this function. By showing that leptin inhibits insulin secretion by decreasing osteocalcin bioactivity, this study illustrates the importance of the relationship existing between fat and skeleton for the regulation of glucose homeostasis.
Im J-A, Yu B-P, Jeon JY, Kim S-H. Relationship between osteocalcin and glucose metabolism in postmenopausal women. Clinica Chimica Acta. 2008 Oct;396(1-2):66-9.
Recently, osteocalcin was found to regulate blood glucose, insulin secretion, and fat deposition in mice. They investigated the relationship between osteocalcin and glucose metabolism in postmenopausal women. They found there was a significant reduction in osteocalcin levels among type 2 diabetes mellitus patients compared with the normal glucose and impaired fasting glucose groups, and those in the highest quartile for osteocalcin were observed to have significantly decreased fasting glucose and HbA1c levels compared with subjects in the lowest quartile. In addition, osteocalcin levels were inversely correlated with glucose, insulin, HbA1c, and insulin resistance. Moreover, multivariate analysis showed that serum osteocalcin was found to be an independent factor associated with glucose and HbA1c. This finding indicates that in humans the skeleton may be involved in energy metabolism by functioning as part of the endocrine system.
Kassi E, Papavassiliou AG. A possible role of osteocalcin in the regulation of insulin secretion: human in vivo evidence? J of Endocrinology. 2008;199(2):151-3.
Recent studies have indicated a novel function for the skeleton in the regulation of energy metabolism. Vitamin K appears to play a role in the insulin response, via osteocalcin. In the present commentary, they speculate on the meaning for bone to act as a ‘rheostat’ modulating glucose metabolism, and how the primitive way of communication between bone and energy metabolism through switch on/off genes evolved to a more complicated ‘talking’ via gain/loss of hormones activity (like osteocalcin) by the carboxylation/decarboxylation process.
Kindblom JM, Ohlsson C, Ljunggren O, Karlsson MK, Tivesten A, Smith U, et al. Plasma osteocalcin is inversely related to fat mass and plasma glucose in elderly Swedish men. J Bone Miner Res. 2009;24:785–791.
Obesity and diabetes have developed into epidemics in the Western world. The osteoblast-derived protein osteocalcin has recently been shown to affect adiposity (obesity) and glucose (sugar) homeostasis in mice, suggesting that the skeleton influences energy metabolism through an endocrine mechanism. This study showed that osteocalcin is inversely related to fat mass and plasma glucose. Although one should be cautious with mechanistic interpretations, our human data support recently published experimental studies, that show the endocrine functions of osteoblast-derived osteocalcin on glucose and fat homeostasis.
Shroff RC, McNair R, Figg N, Skepper JN, Schurgers L, Gupta A, et al. Dialysis accelerates medial vascular calcification in part by triggering smooth muscle cell apoptosis. Circulation. 2008;118(17):1748-57.
Yoshida M, Booth SL, Meigs JB, Saltzman E, Jacques PF. Phylloquinone intake, insulin sensitivity, and glycemic status in men and women. Am J Clin Nutr. 2008;88(1):210–15.
Evidence suggests that vitamin K may have a beneficial role in glucose homeostasis. This study examined the associations between vitamin K intake and insulin sensitivity and glycemic status in men and women aged 26-81 years who were part of the Framingham Offspring Cohort. They found that higher phylloquinone intake was associated with greater insulin sensitivity and glycemic status, and concluded that phylloquine (vitamin K1) has a potentially beneficial role in glucose homeostasis in men and women.
Yoshida M, Jacques PF, Meigs JB, Saltzman E, Shea MK, Gundberg C,Dawson-Hughes B, Dallal G, Booth SL : Effect of vitamin K supplementation on insulin resistance in older men and women. Diabetes Care. 2008;31:2092–96.
We tested the hypothesis that vitamin K supplementation for 36 months will improve insulin resistance in older men and women. Study participants were older nondiabetic men and women (n = 355; aged 60-80 years; 60% women). The effect of 36-month vitamin K supplementation on insulin resistance differed by sex (sex x treatment interaction P = 0.02). HOMA-IR was statistically significantly lower at the 36-month visit among men in the supplement group versus the men in the control group (P = 0.01) after adjustment for baseline HOMA-IR, BMI, and body weight change. They concluded that Vitamin K supplementation for 36 months at doses attainable in the diet may reduce progression of insulin resistance in older men.
Atkins GJ, Welldon KJ, Wijenayaka AR, Bonewald LF, Findlay DM. Vitamin K promotes mineralization, osteoblast-to-osteocyte transition, and an anticatabolic phenotype by {gamma}-carboxylation-dependent and -independent mechanisms. Am J Physiol Cell Physiol. 2009 Dec;297(6):C1358-67.
The family of vitamin K is being studied as potential therapeutic agents for skeletal diseases. This study investigated the effects of vitamins K1, K2, and K3 on the differentiation and function of human primary osteoblasts. All vitamin K types increased the formation of bone-like mineralized matrix and enhanced the osteoblast-to-osteocyte transition. The results indicated that the mineralization is due in part to the positive effect of vitamin K to carboxylate certain proteins, such as osteocalcin. These may be mechanisms by which vitamin K optimizes bone formation and integrity in vivo.
Bacchetta J , Boutroy S , Guebre-Egziabher F, Juillard L, Drai J, Pelletier S, et al. The relationship between adipokines, osteocalcin and bone quality in chronic kidney disease. Nephrol Dial Transplant.2009;24:3120–25.
Fabbrini E, Magkos F, Mohammed BS, et al. Intrahepatic fat, not visceral fat, is linked with metabolic complications of obesity. Proc Natl Acad Sci USA. 2009;106:15430–435.
Fernandez-Real JM, Izquierdo M, Ortega F, et al. The relationship of serum osteocalcin concentration to insulin secretion, sensitivity, and disposal with hypocaloric diet and resistance training. J Clin Endocrinol Metab. 2009;94:237–2459.
Bone has recently been described as exhibiting properties of an endocrine organ by producing osteocalcin that increases insulin sensitivity and secretion in animal models. Abnormalities of bone metabolism occur in subjects with obesity and type 2 diabetes. This study evaluated osteocalcin with insulin sensitivity and insulin secretion in nondiabetic subjects: one cross-sectional study in 149 men (using minimal model), and two longitudinal studies in two independent groups (one formed by 26 women, and the other by 9 men and 11 women), after a mean of 7.3 and 16.8% weight loss, and after a mean of 8.7% weight loss plus regular exercise. They found that circulating osteocalcin could mediate the role of bone as an endocrine organ in humans. They also proposed that osteocalcin represents the missing link in the exercise induced improvement in insulin sensitivity.
Fukumoto S., Martin T. J. Bone as an endocrine organ. Trends in Endocrinology and Metabolism. 2009;20(5):230–6.
Recent evidence shows that the skeleton itself produces at least two hormones, fibroblast growth factor 23 (FGF23) and osteocalcin. FGF23 is produced by osteocytes in bone and acts on the kidney to inhibit 1alpha-hydroxylation of vitamin D and promote phosphorus excretion. Mouse genetics studies revealed that the osteoblast product, osteocalcin, acts on the pancreatic beta-cell to enhance insulin production and on peripheral tissues to increase glucose utilization as a result of increased insulin sensitivity and to reduce visceral fat. This review highlights the recent studies indicating bone's role as an endocrine organ.
Hwang YC, Jeong IK, Ahn KJ, Chung HY. The uncarboxylated form of osteocalcin is associated with improved glucose tolerance and enhanced β-cell function in middle-aged male subjects. Diabetes/Metabolism Research and Reviews. 2009;25:768–72.
Human studies suggest that serum osteocalcin increases beta-cell proliferation and insulin secretion, and improves insulin sensitivity. However, no study has examined the effects of carboxylated osteocalcin on these associations or determined the role of uncarboxylated osteocalcin in glucose metabolism in humans. This study looked at the association between uncarboxylated osteocalcin and beta-cell function and insulin sensitivity in humans. As many as 199 men, aged 25-60 years (mean age, 47 years), who had never been treated with glucose lowering agents, were enrolled in this cross-sectional study. They found that elevated levels of both carboxylated and uncarboxylated forms of osteocalcin were associated with improved glucose tolerance. Moreover, the uncarboxylated form of osteocalcin was found to be associated with enhanced beta-cell function, and the carboxylated form was associated with improved insulin sensitivity in middle-aged male subjects.
Kanazawa I, Yamaguchi T, Yamamoto M, et al. Serum osteocalcin level is associated with glucose metabolism and atherosclerosis parameters in type 2 diabetes mellitus. J Clin Endocrinol Metab. 2009;94:45–9.
Recent animal studies showed that osteocalcin action is related to not only bone metabolism but also glucose metabolism and fat mass. This study investigated the relationship between two bone formation markers, serum osteocalcin and bone-specific alkaline phosphatase, and glucose metabolism, serum adiponectin, and the amount of fat mass as well as atherosclerosis parameters in men and postmenopausal women with type 2 diabetes. The data showed that serum osteocalcin is associated with glucose and total adiponectin levels, fat mass, and atherosclerosis parameters in patients with type 2 diabetes, suggesting that osteocalcin is important for not only bone metabolism but also glucose and fat metabolism.
Krueger T, Westenfeld R, Ketteler M, Schurgers LJ, Floege J: Vitamin K deficiency in CKD patients: a modifiable risk factor for vascular calcification? Kidney Int. 2009;76(1):18-22.
Luo XH , Zhao LL , Yuan LQ , Wang M , Xie H , Liao EY. Development of arterial calcification in adiponectin-deficient mice: adiponectin regulates arterial calcification. J Bone Miner Res. 2009;24:1461–1468.
Zhou M, Ma X, Li H, et al. Serum osteocalcin concentrations in relation to glucose and lipid metabolism in Chinese individuals.Eur J Endocrinol. 2009;161:723–29.
Osteocalcin, a bone-derived protein, has recently been reported to affect energy metabolism. This study investigated the relationship between serum osteocalcin and parameters of adiposity, glucose tolerance, and lipid profile in Chinese subjects who had type 2 diabetes and those who did not, premenopausal women and postmenopausal women. They found that serum osteocalcin concentrations in diabetic patients were significantly lower after adjusted for age, gender, and body mass index (P=0.003). Postmenopausal women had higher osteocalcin concentrations than premenopausal women and men (both P<0.001). Besides age and HbA1c, serum triglyceride was also an independent factor influencing osteocalcin in premenopausal women. They concluded that osteocalcin was closely associated with fat, glucose metabolism and also with lipid metabolism.
Pan Y, Jackson RT. Dietary phylloquinone intakes and metabolic syndrome in US young adults. J Am Coll Nutr. 2009;28(4):369–79.
The aim of this cross sectional analysis was to examine whether and to what extent vitamin K intake measured as phylloquinone is related to Metabolic Syndrome. They looked at the data of 5800 adults who participated in the National Health and Nutrition Examination Survey (NHANES) from 1999-2004. They found that the lowest prevalence of MetS and its 5 components was observed in individuals with the highest phylloquinone intake. The prevalence of low high-density lipoprotein cholesterol (HDL) and elevated blood pressure progressively decreased with increasing phylloquinone intake (p < 0.05 for trend). HDL and C-reactive protein (CRP) levels improved gradually with increasing dietary phylloquinone intake (p < 0.05 for trend). In general, participants who had MetS or its element consumed less phylloquinone from diet compared those who did not. The mean reported dietary phylloquinone intakes suggested that most US young adults consume an insufficient amount of vitamin K from their diet.
Pittas AG, Harris SS, Eliades M, Stark P, Dawson-Hughes B. Association between serum osteocalcin and markers of metabolic phenotype. J Clin Endocrinol Metab. 2009;94:827–32.
Osteocalcin has been reported to contribute to the regulation of glucose tolerance and insulin secretion and sensitivity in experimental animals. This study looked at the association between osteocalcin and markers of dysmetabolic phenotypes in adults age 65 and older. They found that osteocalcin was inversely associated with fasting plasma glucose levels, fasting insulin, C-reactive protein and body fat. They concluded that osteocalcin concentrations were inversely associated with measures of obesity and dysmetabolic phenotypes.
Rosen C. J. Leptin’s RIGHT turn to the brain stem. Cell Metabolism. 2009;10(4):243–44.
Data indicates that skeletal remodeling is intimately connected to the regulation of metabolism.
Shea M K, Benjamin E J, Dupuis J, Massaro JM, Jacques PF, D’Agostino RB Sr, et al. Genetic and non-genetic correlates of vitamins K and D. European Journal of Clinical Nutrition. 2009;63(4):458–64.
Shea MK, Gundberg CM, Meigs JB, et al. Gamma-carboxylation of osteocalcin and insulin resistance in older men and women. Am J Clin Nutr. 2009;90:1230–35.
The skeletal protein osteocalcin is carboxylated by vitamin K. High serum uncarboxylated osteocalcin reflects low vitamin K status. In vitro and animal studies indicate that high uncarboxylated osteocalcin is associated with reduced insulin resistance. This study examined associations between circulating forms of osteocalcin (total, uncarboxylated, and carboxylated) and insulin resistance in older men and women. They found that in older adults, circulating uncarboxylated osteocalcin was not associated with insulin resistance. In contrast, elevated carboxylated osteocalcin and total osteocalcin were associated with lower insulin resistance, which supports a potential link between skeletal physiology and insulin resistance in humans.
Yoshizawa T., Hinoi E., Dae Y. J., et al. The transcription factor ATF4 regulates glucose metabolism in mice through its expression in osteoblasts. Journal of Clinical Investigation. 2009;119(9):2807–17.
The recent demonstration that osteoblasts have a role in controlling energy metabolism suggests that they express cell-specific regulatory genes involved in this process. These results provide a transcriptional basis to the observation that osteoblasts fulfill endocrine functions and identify ATF4 as a regulator of most functions of osteoblasts.
2010s
Beulens JWJ, van der A DL, Grobbee, DE, Sluijs I, Spijkerman AMW, van der Schouw YT. Dietary phylloquinone and menaquinones intake and risk of type 2 diabetes. Diabetes Care. 2010 Aug;33(8):169.
This study investigated whether dietary phylloquinone and menaquinone intakes are related to risk of type 2 diabetes, using data from a prospective cohort study in 38,094 Dutch men and women, aged 20–70 years. During 10.3 years of follow-up, 918 incident cases of diabetes were documented. The study showed that both phylloquinone and menaquinone intake were associated with a reduced risk of type 2 diabetes.
Cranenburg EC, Koos R, Schurgers LJ, Magdeleyns EJ, Schoonbrood TH, Landewe RB, et al. Characterisation and potential diagnostic value of circulating matrix Gla protein (MGP) species. Thromb Haemost. 2010, 104(4):811-22.
Matrix (Gla) Protein (MGP) is an important local inhibitor of vascular calcification, which can undergo two post-translational modifications: vitamin K-dependent y-glutamate carboxylation and serine phosphorylation. Since both modifications can be exerted incompletely, various MGP species can be detected in the circulation. MGP levels were measured in patients with rheumatic disease, aortic valve disease, and end-stage disease, as well as in volunteers after vitamin K supplementation (VKS) and treatment with vitamin K antagonists (VKA). They found major differences between the MGP assays, including significantly different behavior with regard to vascular disease and the response to VKA and VKS.
Ferron M, Wei J, Yoshizawa T, et al. Insulin signaling in osteoblasts integrates bone remodeling and energy metabolism.Cell. 2010;142:296–308.
The osteoblast is a cell in the bone that favors glucose metabolism through a hormone, osteocalcin, that becomes active once uncarboxylated. We show here that insulin signaling in osteoblasts is necessary for whole-body glucose homeostasis because it increases osteocalcin activity. Since bone resorption occurs at a pH acid enough to decarboxylate proteins, osteoclasts determine the carboxylation status and function of osteocalcin. Accordingly, increasing or decreasing insulin signaling in osteoblasts promotes or hampers glucose metabolism in mice and humans. Hence, in a feed-forward loop, insulin signals in osteoblasts to activate a hormone osteocalcin, that promotes glucose metabolism.
Fulzele K, Riddle RC, DiGirolamo DJ, et al. Insulin receptor signaling in osteoblasts regulates postnatal bone acquisition and body composition. Cell. 2010;142:309–19.
Energy balance in mammals is controlled by circulating hormones that coordinate fuel production in metabolically active tissues. Osteocalcin, in its undercarboxylated, hormonal form, regulates fat deposition and is a potent insulin secretagogue. This study showed that insulin receptor (IR) signaling in osteoblasts controls osteoblast development and osteocalcin expression. Mice lacking IR in osteoblasts have low circulating undercarboxylated osteocalcin and reduced bone acquisition due to decreased bone formation and deficient numbers of osteoblasts. With age, these mice develop marked peripheral adiposity and hyperglycemia accompanied by severe glucose intolerance and insulin resistance. The metabolic abnormalities in these mice are improved by infusion of exogenous undercarboxylated osteocalcin. These results indicate the existence of a bone-pancreas endocrine loop through which insulin signaling in the osteoblast ensures osteoblast differentiation and stimulates osteocalcin production, which in turn regulates insulin sensitivity and pancreatic insulin secretion to control glucose homeostasis.
Holden RM, Morton AR, Garland JS, Pavlov A, Day AG, Booth SL. Vitamins K and D status in stages 3–5 chronic kidney disease. Clin J Am Soc Nephrol. 2010, 5(4):590-97.
Vitamin K, vitamin K-dependent proteins, and vitamin D may be involved in the regulation of calcification in chronic kidney disease (CKD). In this study, dietary vitamin K intake was associated with higher phylloquinone and lower PIVKA-II. These data indicate that a suboptimal vitamin K and D status is prevalent in patients with CKD. Sufficiency of both vitamins K and D was similarly predicted by measures of overall improved nutritional status. Proteinuria was associated with both a suboptimal vitamin D status as well as worse peripheral vitamin K status.
Kumar R, Binkley N, Vella A. Effect of phylloquinone supplementation on glucose homeostasis in humans. Am J Clin Nutr. 2010;92(6):1528–32.
Under-γ-carboxylated osteocalcin (ucOC) increases insulin secretion and decreases glucose concentrations in mice. In this study, we determined whether changes in ucOC concentrations in humans were associated with changes in insulin and glucose concentrations. Twenty-one community-dwelling postmenopausal women received 1 mg phylloquinone daily for 12 mo (experimental group), and 21 subjects were treated with a placebo during the same period (control group). They found that in postmenopausal women, phylloquinone administration was not associated with changes in insulin secretion and action despite reductions in ucOC concentrations. Changes in ucOC concentrations do not alter glucose metabolism in women.
Motyl KJ, McCabe LR, Schwartz AV. Bone and glucose metabolism: a two-way street. Arch Biochem Biophys. 2010 Nov 1;503(1):2-10.
Evidence from rodent models indicates that undercarboxylated osteocalcin (ucOC), a product of osteoblasts, is a hormone affecting insulin production by the pancreas and insulin sensitivity in peripheral tissues. Clinical research to test whether this relationship is found in humans is just beginning to emerge. Cross-sectional studies confirm associations between total osteocalcin (OC), ucOC and glucose metabolism but cannot distinguish causality. Further exploration into the physiological and mechanistic effects of ucOC and OC, in rodent models and clinical studies, is necessary to determine to what extent the skeleton regulates energy metabolism in humans.
Parker BD, Schurgers LJ, Vermeer C, Schiller NB, Whooley MA, Ix JHT. The association of uncarboxylated matrix Gla protein with mitral annular calcification differs by diabetes status: The Heart and Soul study. Atherosclerosis. 2010;210(1):320-5.
Mitral annular calcification (MAC) and aortic stenosis (AS) are associated with systemic calcification and cardiovascular disease (CVD) events. Matrix Gla protein (MGP) is an inhibitor of vascular calcification and lower levels of its precursor - uncarboxylated MGP (ucMGP) - are associated with vascular calcification in pilot studies. They found that among outpatients with stable CVD, higher ucMGP is associated with lower odds of MAC in persons without diabetes, and higher odds of MAC in persons with diabetes.
Prats-Puig A, Mas-Parareda M, Riera-Perez E, Gonzalez-Forcadell D, Mier C, Mallol-Guisset M, et al. Carboxylation of osteocalcin affects its association with metabolic parameters in healthy children. Diabetes Care. 2010 Mar;33(3):661-3.
Osteocalcin (OC), a bone-derived protein, has been shown to regulate metabolic pathways in mice. Undercarboxylated OC (ucOC), increases adiponectin and insulin secretion. It is unclear if carboxylation of OC affects its association with metabolic parameters in humans. The associations between ucOC, cOC, total and high-molecular-weight (HMW) adiponectin, and insulin secretion (HOMA]-β) were investigated in a population-based sample of healthy prepubertal. In a weight-dependent manner, cOC and the proportion of ucOC are differentially related to adiponectin and insulin secretion in healthy children.
Rached M.-T., Kode A., Silva B. C., et al. FoxO1 expression in osteoblasts regulates glucose homeostasis through regulation of osteocalcin in mice. Journal of Clinical Investigation. 2010;120(1):357–68.
Reinehr T, Roth CL. A new link between skeleton, obesity and insulin resistance: relationships between osteocalcin, leptin and insulin resistance in obese children before and after weight loss. Int J Obes (Lond). 2010;34:852–58.
The skeleton is regarded as an endocrine organ that affects energy metabolism. However, there are very limited data available concerning the relationships between the osteoblast-derived hormone osteocalcin, weight status, adiponectin and leptin in obese humans, especially in children. This study analyzed osteocalcin, adiponectin, leptin and insulin resistance (IR) index homeostasis model assessment (HOMA) in 60 obese and 19 age- and gender-matched normal weight children. They found that osteocalcin levels were lower in obese children and were related to IR and leptin both in cross-sectional and longitudinal analyses. Therefore, osteocalcin might be a new promising link between obesity and IR.
Saleem U, Mosley TH, Kullo IJ. Serum osteocalcin is associated with measures of insulin resistance, adipokine levels, and the presence of metabolic syndrome. Atertioscler Thromb Vasc Biol. 2010 Jul;30(7):1474-78.
This study investigated whether serum osteocalcin was associated with measures of insulin resistance, adipokine levels and metabolic syndrome. They measured serum osteocalcin in 1284 blacks, and 1209 non Hispanic whites, belonging to hypertensive sibships. Prevalence of metabolic syndrome was 50% in blacks and 49% in nonhispanic whites. Osteocalcin levels were inversely correlated with body mass index, fasting glucose and insulin, homeostasis model assessment of insulin resistance, triglycerides and leptin and positively correlated with adiponectin.
Schurgers LJ, Barreto DV, Barreto FC, Liabeuf S, Renard C, Magdeleyns EJ, et al. The circulating inactive form of matrix gla protein is a surrogate marker for vascular calcification in chronic kidney disease: a preliminary report. Clin J Am Soc Nephrol. 2010;5(4):568-575.
Vitamin K-dependent matrix Gla protein (MGP) acts as a calcification inhibitor in vitro and in vivo. The present study was performed to (1) determine plasma levels of dephosphorylated, uncarboxylated MGP (dp-ucMGP) in a cohort of patients at different stages of chronic kidney disease (CKD) and (2) evaluate the association between dp-ucMGP levels on one hand and aortic calcification and mortality on the other. They found that plasma dp-ucMGP levels increased progressively with CKD stage, and was associated with the severity of aortic calcification. They concluded that the amount of uncarboxylated MGP would be a surrogate marker for vascular calcification in CKD.
Tanaka S, Nishiumi S, Nishida M, Mizushina Y, Kobayashi K, Masuda A, et al. Vitamin K3 attenuates lipopolysaccharide-induced acute lung injury through inhibition of nuclear factor-kappa B activation. Clin Exp Immunol. 2010;160(2):283–292.
Vitamin K is a family of fat-soluble compounds including phylloquinone (vitamin K1), menaquinone (vitamin K2) and menadione (vitamin K3). Recently, it was reported that vitamin K, especially vitamins K1 and K2, exert a variety of biological effects, and these compounds are expected to be candidates for therapeutic agents against various diseases. In this study, we investigated the anti-inflammatory effects of vitamin K3 in in vitro cultured cell experiments and in vivo animal experiments. They found that vitamin K3 may be an effective therapeutic strategy against acute lung injury including acute respiratory distress syndrome (ARDS).
Thomsen SB, Rathcke CN, Zerahn B, Vestergaard H. Increased levels of the calcification marker matrix Gla Protein and the inflammatory markers YKL-40 and CRP in patients with type 2 diabetes and ischemic heart disease. Cardiovasc Diabetol. 2010;9:86.
Low grade inflammation is of pathogenic importance in atherosclerosis and in the development of cardiovascular disease (CVD) and type 2 diabetes (T2D). Matrix GLA protein (MGP), an inhibitor of medial calcification of arteries, is increased in patients with atherosclerosis. In the present study levels of markers of calcification (MGP) and inflammation (YKL-40, hsCRP) were evaluated in patients with T2 D and/or ischemic heart disease (IHD). The results indicated that in patients with type 2 Diabetes or heart disease, they found increased levels of MGP and inflammation, likely reflecting a low grade inflammatory state.
Winhofer Y, Handisurya A, Tura A, et al. Osteocalcin is related to enhanced insulin secretion in gestational diabetes. Diabetes Care. 2010;33:139–143.
There is growing evidence that osteocalcin, an osteoblast-derived protein locally acting on bone formation, can increase insulin secretion as well as insulin sensitivity and thus prevent the development of obesity and diabetes in experimental animals. In humans, osteocalcin has been reported to be decreased in patients with type 2 diabetes. Because gestational diabetes mellitus (GDM) can serve as a model of pre-type 2 diabetes, the aim of this study was to investigate osteocalcin in GDM. They found that osteocalcin was higher in women with gestational diabetes, and that osteocalcin showed a significant correlation with insulin secretion. They concluded that osteocalcin can enhance insulin secretion in insulin-resistant states.
Bao Y, Zhou M, Lu Z, Huating L, Wang Y. Sun L, et al. Serum levels of osteocalcin are inversely associated with the metabolic syndrome and the severity of coronary artery disease in Chinese men. Clin Endocrinology. 2011 Aug;75(2):196-201.
Osteocalcin is a bone-derived protein and has been shown to play an important role in regulating glucose and fat metabolism. This study investigated the association of serum levels of osteocalcin with the metabolic syndrome (MS) and coronary atherosclerosis in Chinese men. Osteocalcin levels in patients with the MS were significantly lower compared with those in non-MS subjects (P < 0·001) and decreased correspondingly with the increasing number of components of the MS (P < 0·001). They concluded that serum osteocalcin is inversely associated with the MS as well as the severity of coronary atherosclerosis in Chinese men, supporting the new concept that bone has the reciprocal regulation with energy metabolism.
Basu R, Peterson J, Rizza R, Khosla S. Effects of physiological variations in circulating insulin levels on bone turnover in humans. J Clin Endocrinol Metab. 2011;96:1450–55.
Uncarboxylated osteocalcin enhances insulin sensitivity. This study looked at insulin levels and bone metabolism in humans, and concluded that insulin sensitivity correlates with bone resorption, but do not impact bone metabolism.
Choi HJ, Yu J, Choi H, An JH, Kim SW, Park KS, Jang HC, Kim SY, Shin CS. Vitamin K2 supplementation improves insulin sensitivity via osteocalcin metabolism: a placebo-controlled trial. Diabetes Care. 2011 Sep;34(9):e147.
This study demonstrated for the first time that vitamin K2 supplementation for 4 weeks increased insulin sensitivity in healthy young men, which seems to be related to increased cOC rather than modulation of inflammation. Forty-two healthy young male volunteers received 30 mg of vitamin K2 (MK4) or placebo for 4 weeks. Their results are consistent with previous studies that demonstrated improved glucose intolerance or relieved insulin resistance by treatment with vitamin K1 or vitamin K2 (MK4), respectively. We conclude that unlike in rodents, cOC rather than ucOC may be the endocrine hormone that increases insulin sensitivity in humans. Alternatively, cOC can directly regulate glucose disposal at skeletal muscle or adipose tissues.
Clemens T. L., Karsenty G. The osteoblast: An insulin target cell controlling glucose homeostasis. Journal of Bone and Mineral Research. 2011;26(4):677–80.
The past five years have witnessed the emergence and discovery of unexpected functions played by the skeleton in whole-organism physiology. Among these newly described tasks is the role of bone in the control of energy metabolism, which is achieved through the secretion of osteocalcin, an osteoblast-derived hormone regulating insulin secretion, insulin sensitivity, and energy expenditure. Importantly, this function of insulin signaling in osteoblasts was achieved through the negative regulation of osteocalcin carboxylation and bioavailability. Interestingly, it appears that insulin signaling in osteoblasts induced osteocalcin activation by stimulating osteoclast activity. Our findings establish that the osteoblast is an important target used by insulin to control whole-body glucose homeostasis and identify bone resorption as the mechanism regulating osteocalcin activation.
Confavreux CB. Bone: From a reservoir of minerals to a regulator of energy metabolism. Kidney Intl Suppl. 2011 Apr;79(S121):S14-S19.
Bone remodeling affects energy metabolism through uncarboxylated osteocalcin, a recently discovered hormone secreted by osteoblasts. This review traces how energy metabolism affects osteoblasts through the central control of bone. The role of osteocalcin (insulin secretion, insulin sensitivity, and pancreas β-cell proliferation) in the regulation of energy metabolism is described. Then, the connections between insulin signaling on osteoblasts and the release of uncarboxylated osteocalcin during osteoclast bone resorption are reported.
Diamanti-Kandarakis E, Livadas S, Katsikis I, et al. Serum concentrations of carboxylated osteocalcin are increased and associated with several components of the polycystic ovarian syndrome. J Bone Miner Metab. 2011;29:201–6.
Intriguing studies suggest that osteocalcin (OC) and its carboxylated (Gla)/uncarboxylated form are involved in the regulation of insulin secretion and action. In this study, we evaluated the serum levels of osteocalcin and Gla osteocalcin and their possible associations with metabolic, hormonal, and ultrasonographic components of PSOS: 97 women were studied, 50 PCOS patients and 47 controls, matched for age and body mass index (BMI). The findings suggest a potential interaction between bone-derived markers and the metabolic/hormonal abnormalities observed in PCOS.
Ducy P. The role of osteocalcin in the endocrine cross-talk between bone remodeling and energy metabolism. Diabetologia. 2011 Jun;54(6):1291-7.
This review summarises the molecular and cellular bases of the present knowledge on osteocalcin biology and discusses the potential relevance of osteocalcin to human metabolism and pathology. Osteocalcin, a hormone secreted by osteoblasts, was identified as a positive regulator of insulin secretion, insulin resistance and energy expenditure. Remarkably, insulin signalling in osteoblasts is a positive regulator of osteocalcin production and activation via its ability to indirectly enhance bone resorption by osteoclasts. Hence, osteocalcin is part of a complex signalling network between bone and the organs more classically associated with the regulation of energy homeostasis, such as the pancreas and adipose tissue.
Fadini GP, Albiero M, Menegazzo L, Boscaro E, Vigili De Kreutzenberg S, et al. Widespread increase in myeloid calcifying cells contributes to ectopic vascular calcification in type 2 diabetes. Circ Res. 2011;108(9):1112-21.
García-Martín A, Cortés-Berdonces M, Luque-Fernández I, Rozas-Moreno P, Quesada-Charneco M, Muñoz-Torres M. Osteocalcin as a marker of metabolic risk in healthy postmenopausal women. Menopause. 2011;18(5):537-41.
Several studies have reported the role of osteocalcin on glucose and fat metabolism. This study analyzed the relationship between the concentration of osteocalcin and metabolic risk factors in healthy postmenopausal women. They found that serum osteocalcin was negatively correlated with fasting plasma glucose levels and significantly lower osteocalcin levels in women with impaired fasting glucose levels than in those with normoglycemia. They also found lower concentrations of osteocalcin in obese women versus nonobese women and women with increased low-density lipoprotein cholesterol levels versus those with low LDL-c levels. They suggest the potential usefulness of serum osteocalcin as a predictor for increased risk of diabetes in postmenopausal women.
Gravenstein KS, Napora JK, Short RG, et al. Cross-sectional evidence of a signaling pathway from bone homeostasis to glucose metabolism. The Journal of Clinical Endocrinology & Metabolism. 2011;96(6):E884–E890.
Preclinical studies suggested the existence of a signaling pathway connecting bone and glucose metabolisms. This study looked at the reciprocal relationships of adiponectin, leptin, osteocalcin, insulin resistance, and insulin secretion to verify whether such relationships are consistent with a signaling pathway connecting bone homeostasis and glucose metabolism. The study was conducted with community-dwelling volunteers participating in the Baltimore Longitudinal Study of Aging. The results indicate that bone and glucose metabolisms are probably connected through a complex pathway that involves leptin, osteocalcin, and adiponectin. The clinical relevance of such a pathway for bone pathology in diabetes should be further investigated.
Hu, FB. Globalization of Diabetes. The role of diet, lifestyle and genes. Diabetes Care. 2011 Jun;34(6):1249-57.
Type 2 diabetes is a global public health crisis that threatens the economies of all nations, particularly developing countries. Fueled by rapid urbanization, nutrition transition, and increasingly sedentary lifestyles, the epidemic has grown in parallel with the worldwide rise in obesity. Asia's large population and rapid economic development have made it an epicenter of the epidemic. Asian populations tend to develop diabetes at younger ages and lower BMI levels than Caucasians. Epidemiologic studies and randomized clinical trials show that type 2 diabetes is largely preventable through diet and lifestyle modifications. Translating these findings into practice, however, requires fundamental changes in public policies, the food and built environments, and health systems.
Idelevich A , Rais Y , Monsonego-Ornan E. Bone Gla protein increases HIF-1α-dependent glucose metabolism and induces cartilage and vascular calcification. Arterioscler Thromb Vasc Biol. 2011;31:e55–e71.
Bone Gla Protein (BGP, osteocalcin) is commonly present in the calcified vasculature and was recently shown to be an energy metabolism-regulating hormone. This study investigates the role of BGP in cartilage and vasculature mineralization. They concluded that bone gla protein shifts cells toward a glycolytic breakdown of glucie and stimulates calcification of cartilage and vasculature.
Iwamoto J, Sato Y, Takeda T, Matsumoto H. Bone quality and vitamin K2 in type 2 diabetes: Review of preclinical and clinical studies. Nutr Rev. 2011 Mar;69(3):162-7.
Type 2 diabetic patients are at high risk of bone fractures even if their bone mineral density is normal or high. The present review was conducted to provide an overview of the evidence on the effect of vitamin K(2) on bone quality in persons with type 2 diabetes. Vitamin K(2) stimulates γ-carboxylation of osteocalcin and can increase bone formation. One recent pre-clinical study showed that vitamin K(2) administration in a type 2 diabetic rat model had the following skeletal benefits: increased serum osteocalcin, improved collagen cross-link profiles, and increased bone strength. These new findings suggesting a possible beneficial effect of vitamin K(2) supplementation on bone quality in type 2 diabetes warrant further investigation.
Iwamoto J, Seki A, Sato Y, Matsumoto H, Takeda T, Yeh JK. Vitamin K2 prevents hyperglycemia and cancellous osteopenia in rats with streptozotocin-induced type 1 diabetes. Calcif Tissue Int. 2011 Feb;88(2):162-8.
The purpose of the present study was to examine the effect of vitamin Kâ‚‚ bone mass in rats with induced type 1 diabetes. Twenty-seven male Sprague-Dawley rats aged 12 weeks were randomized by the weight-stratified method into three groups. The administration of vitamin Kâ‚‚ to diabetes-induced rats prevented the development of hyperglycemia and a decrease in femoral weight. Vitamin Kâ‚‚ also prevented osteopenia. These results suggest that vitamin Kâ‚‚ has beneficial effects on glucose concentration and bone mass in rats with induced type 1 diabetes.
Kanazawa I , Yamaguchi T , Tada Y , Yamauchi M , Yano S , Sugimoto T. Serum osteocalcin level is positively associated with insulin sensitivity and secretion in patients with type 2 diabetes. Bone. 2011;48:720–725.
Bone is being recognized as an endocrine organ. In this cross-sectional study, they studied 101 postmenopausal women and 152 men with type 2 diabetes, who have not taken drugs for diabetes or osteoporosis. They also examined 75 g oral glucose tolerance test (OGTT) in 18 postmenopausal women and 20 men who visited our clinic for medical check-up for diabetes. They found that serum osteocalcin level is positively associated with insulin sensitivity and secretion in Japanese patients with type 2 diabetes.
Levinger I, Zebaze R, Jerums G, Hare DL, Selig S, Seeman E. The effect of acute exercise on undercarboxylated osteocalcin in obese men. Osteoporos Int. 2011;22:1621–26.
Exercise reduces serum glucose and improves insulin sensitivity in obese individuals and in those with type 2 diabetes. Osteocalcin in its undercarboxylated (ucOC) form may contribute to the regulation of glucose homeostasis. This study of middle aged men, doing exercise, found that uncarboxylated osteocalcin plays a role in the reduction in glucose after exercise.
Oury F, Sumara G, Sumara O, Ferron M, Chang H, Smith CE, et al. Endocrine regulation of male fertility by the skeleton. Cell. 2011;144(5):796–09.
It is now known that in males, bone acts as a regulator of fertility. This demonstrates that osteoblasts are able to induce testosterone production by the testes, though they fail to influence estrogen production by the ovaries. Analyses of cell-specific loss- and gain-of-function models reveal that the osteoblast-derived hormone osteocalcin performs this endocrine function. This study expands the physiological repertoire of osteocalcin and provides the first evidence that the skeleton is an endocrine regulator of reproduction.
Pollock NK, Bernard PJ, Gower BA, Gundberg CM, Wenger K, Misra S, Bassali RW, Davis CL. Lower uncarboxylated osteocalcin concentrations in children with prediabetes is associated with β-Cell function. J Clin Endocrinol Metab. 2011 Jul:96(7):E1092-E1099.
Although animal studies suggest that it is the uncarboxylated rather than carboxylated form of osteocalcin that affects glucose homeostasis, the human data are scant and equivocal. This study investigated associations of uncarboxylated and carboxylated forms of osteocalcin with insulin sensitivity and β-cell function in 140 overweight prepubertal children (43% female, 46% black, 84% obese) with normal glucose levels (n = 99) and prediabetes (n = 41). The data suggest that the lower uncarboxylated osteocalcin concentrations found in children with prediabetes may be associated with β-cell dysfunction. In addition, our findings between carboxylated osteocalcin and insulin sensitivity suggest that carboxylated osteocalcin plays a role in human glucose homeostasis.
Schafer AL, Sellmeyer DE, Schwartz AV, Rosen CJ, Vittinghoff E, Palermo L, et al. Change in undercarboxylated osteocalcin is associated with changes in body weight, fat mass, and adiponectin: parathyroid hormone (1–84) or alendronate therapy in postmenopausal women with osteoporosis (the PaTH Study). Journal of Clinical Endocrinology and Metabolism. 2011;96:E1982–E1989.
Uncarboxylated osteocalcin influences fat and glucose homeostasis, like a hormone. This study found that changes in ucOC induced by osteoporosis medications and alendronate is associated with metabolic changes. Those with greater increases in ucOC had greater decreases in body weight and fat mass, and greater increases in the insulin-sensitizing adiponectin. This supports the role for ucOC in the skeletal regulation of energy metabolism in humans.
Schauer IE, Snell-Bergeon JK, Bergman BC, Maahs DM, Kretowski A, Eckel RH, et al. Insulin resistance, defective insulin-mediated fatty acid suppression, and coronary artery calcification in subjects with and without type 1 diabetes: The CACTI study. Diabetes. 2011 Jan;60(1):306-14.
Type 1 diabetic patients are insulin resistant compared with nondiabetic subjects, and the degree of resistance is not related to current glycemic control. Insulin resistance also predicts the extent of coronary artery calcification and may contribute to the increased risk of cardiovascular disease in patients with type 1 diabetes as well as subjects without diabetes. The Coronary Artery Calcification in Type 1 Diabetes (CACTI) study has followed a cohort of type 1 diabetic subjects and similar nondiabetic controls with electron beam computed tomorgraphy for measurement of CAC and CVD outcomes for 6 years. This study supports the conclusion that profound insulin resistance in type 1 diabetes extends beyond glucose control to regulation of fat metabolism, and may be associated with increased coronary atherosclerosis.
Tan A, Gao Y, Yang X, Zhang H, Qin X, Mo L, Peng T et al. Low serum osteocalcin level is a potential marker for metabolic syndrome: Results from a Chinese male population survey. Metabolism. 2011 Aug;60(8):1186-92.
Osteocalcin has been recognized as a bone-derived hormone that regulate energy metabolism. Components of MetS, osteocalcin, body mass index (BMI), and prevalence of MetS were assessed in 2344 men aged 20 to 69 years who participated in the population-based Fangchenggang Area Male Health and Examination Survey, which was carried out in Guangxi province of China from September 2009 to December 2009. Osteocalcin had a statistically significant positive correlation with high-density lipoprotein cholesterol and a negative relationship with glucose, blood pressure, triglycerides, waist circumference, and BMI after adjustment for age (all P < .001). In a Chinese male population, we firstly identified an inverse association of serum osteocalcin levels with MetS, independent from the well-known MetS risk factors.
Villafan-Bernal JR, Sanchez-Enriquez S, Munoz-Valle JF. Molecular modulation of osteocalin and its relevance in diabetes (Review). Int J Molec Medicine. 2011;28:283-93.
Osteocalcin (Oc) is encoded by the bone γ-carboxyglutamate (Gla) protein (BGLAP) gene, and it is released by osteoblasts during osteogenesis. It was recently demonstrated that uncarboxylated Oc improves glucose tolerance and insulin sensitivity in mice by increasing the expression and secretion of insulin in β -cells and of adiponectin in adipocytes. Humans with type 2 diabetes have significantly lower serum levels of Oc than healthy individuals and indeed, serum Oc levels have been inversely correlated with fasting plasma glucose, fasting insulin and the homeostasis model assessment of insulin resistance (HOMA-IR) index. This review summarizes the molecular mechanisms involved in the modulation of Oc expression, and discusses the potential relevance of Oc in the patho-genesis and treatment of diabetes.
Yoshikawa Y, Kode A, Zu L, Mosialou I, Silva BC, Ferron M, et al. Genetic evidence points to an osteocalcin-independent influence of osteoblasts on energy metabolism. J Bone Miner Res. 2011 Sep;26(():2012-25.
The skeleton has been shown recently to regulate glucose metabolism through osteocalcin, which favors β-cell proliferation, insulin secretion, insulin sensitivity, and energy expenditure. An implication of this finding is that a decrease in osteoblast numbers would compromise glucose metabolism in an osteocalcin-dependent manner. To test this hypothesis, osteoblasts were inducibly ablated by cross-breeding transgenic mice. Ablation of osteoblasts in adult mice profoundly affected glucose metabolism. In a manner similar to what is seen in the case of osteocalcin deficiency, a partial ablation of this cell population resulted in hypoinsulinemia, hyperglycemia, glucose intolerance, and decreased insulin sensitivity. While administration of osteocalcin reversed (fully) the glucose intolerance and reinstated normal blood glucose and insulin levels, it only partially restored insulin sensitivity and did not affect the improved gonadal fat weight and energy expenditure in osteoblast-depleted mice.
Bullo M, Moreno-Navarrete JM, Fernandez-Real JM, Salas-Salvado J. Total and undercarboxylated osteocalcin predict changes in insulin sensitivity and β cell function in elderly men at high cardiovascular risk. Am J Clin Nutr. 2012;95:249–55.
The objective was to examine cross-sectional and longitudinal associations between circulating forms of osteocalcin and insulin secretion and sensitivity in elderly men at high cardiovascular risk. We found that changes in serum osteocalcin and ucOC are associated with an improvement in insulin secretion and sensitivity, which suggests a possible role of bone in the development of type 2 diabetes.
Chatrou ML, Winckers K, Hackeng TM, Reutelingsperger CP, Schurgers LJ. Vascular calcification: the price to pay for anticoagulation therapy with vitamin K-antagonists. Blood Rev. 2012;26(4):155-66.
Vitamin K-antagonists (VKA) are the most widely used anti-thrombotic drugs with substantial efficacy in reducing risk of arterial and venous thrombosis. However VKA inhibits not only post-translational activation of vitamin K-dependent coagulation factors but also synthesis of functional extra-hepatic vitamin K-dependent proteins thereby eliciting undesired and dangerous side-effects. Vascular calcification is one of the recently revealed side-effects of Vitamin K Antagonists. This review addresses vitamin K-cycle and vitamin K-dependent processes of vascular calcification that are affected by VKA. We conclude that there is a growing need for better understanding of the effects of anticoagulants on vascular calcification and atherosclerosis.
Chen XC, Tian H-M, Yu X-J. Bone delivers its energy information to fat and islets through osteocalcin. Orthopaedic Surgery. 2012 May;4(2):114-17.
Bone has emerged as a novel endocrine organ for its ability to produce hormones and involvement in several regulatory feedback loops. Osteocalcin (OCN) is released into bloodstream during bone resorption and has been demonstrated to exert endocrine regulation on islets, fat and male testis to form feedback loops. We hypothesize that bone delivers its energy metabolism signals to related energy-regulating organs through OCN. Osteocalcin has close interactions with islets and fat, and it shows ability to stimulate islets and fat to secret insulin and adiponectin, respectively. Islets and fat are important organs involved in energy metabolism. Second, OCN undergoes physiological fluctuations during a lifetime. In children and adolescents, during the development of osteoporosis or after bone fracture, OCN level increases significantly. The elevated OCN at these stages represents enhanced bone turnover and metabolic activity, which require more energy supply. Through systemic release of OCN, bone delivers its energy-demanding information to other organs to satisfy its energy requirement.
Confavreux CB , Borel O , Lee F , et al.. Osteoid osteoma is an osteocalcinoma affecting glucose metabolism. Osteoporos Int. 2012;23:1645–50.
Osteocalcin is a hormone secreted by osteoblasts, which regulates energy metabolism by increasing β-cell proliferation, insulin secretion, insulin sensitivity, and energy expenditure. The study was designed to assess the effect of surgical resection of osteoid osteoma on osteocalcin and blood glucose levels in comparison with patients undergoing knee surgery and healthy volunteers. After resection of the osteoid osteomas, we observed a decrease of osteocalcin by 62% and 30% from the initial levels. Simultaneously, blood glucose increased respectively by 32% and 15%. Bone turnover markers were not affected. This case study shows for the first time that osteocalcin in humans affects blood glucose level. This study also suggests that ostoid osteoma may be considered, at least in part, as an osteocalcinoma.
DiGirolamo DJ, Clemens TL. Kousteni S. The skeleton as an endocrine organ. Nature Reviews Rheumatology. 2012;8(11):674–83.
Surprising new discoveries in the field of skeletal biology show that bone cells produce endocrine hormones that regulate phosphate and glucose homeostasis. Consideration of evolutionary and comparative biology provides clues that a key driving force for the emergence of these hormonal pathways was the development of a large, energy-expensive musculoskeletal system. Specialized bone cells also evolved and produced endocrine hormones to integrate the skeleton in global mineral and nutrient homeostasis. The recognition of bone as a true endocrine organ represents a fertile area for further research and should improve the diagnosis and treatment of metabolic diseases such as osteoporosis and diabetes mellitus.
Ferron M, Karsenty G. Contribution of bone resorption to the control of glucose metabolism. J Bone Miner Res. 2012;27 (Suppl 1). Available at http://www.asbmr.org/Meetings/AnnualMeeting/AbstractDetail.aspx?aid=0f58446f-2af4-4360-ade4-4670cd3409ad
Osteocalcin is a hormone produced in bones by osteoblasts. Osteocalcin exists in two forms, carboxylated and uncarboxylated (ucOC). It appears that ucOC appears to function as a hormone. Osteoclasts decarboxylate and active osteocalcin. This study looked at mouse strains and found that osteoclasts control glucose metabolism through the regulation of osteocalcin decarboxylation.
Ferron M, McKee MD, Levine RL, Ducy P, Karsenty G. Intermittent injections of osteocalcin improve glucose metabolism and prevent type 2 diabetes in mice. Bone. 2012 Feb;50(2):568-75.
The uncarboxylated form of osteocalcin is a hormone favoring glucose handling and increasing energy expenditure. As a result, the absence of osteocalcin leads to glucose intolerance in mice, while genetically modificed mice with an increase in uncarboxylated osteocalcin are protected from type 2 diabetes and obesity. This study tested the therapeutic potential of intermittent administration of ostelcalcin in a mouse. We found that daily injections of osteocalcin at either 3 or 30ng/g/day significantly improved glucose tolerance and insulin sensitivity in mice fed a normal diet. This was attributable to an increase in both beta-cell mall and insulin secretion. Overall, these results provide evidence that daily injections of osteocalcin can improve glucose handling and prevent the development of type 2 diabetes.
Flammer AJ, Gossl M, Li J, Matsuo Y, Reriani M, Loeffler D, Simari RD, Lerman LO, Khosla S, Lerman A: Patients with an HbA1c in the prediabetic and diabetic range have higher numbers of circulating cells with osteogenic and endothelial progenitor cell markers. J Clin EndocrinolMetab 2012, 97(12):4761-68.
Gundberg CM, Lian JB, Booth SL. Vitamin K-dependent carboxylation of osteocalcin: Friend or foe? Adv. Nutr. 2012 Mar;3(2):149-57.
Osteocalcin originates from osteoblastic synthesis and is deposited into bone or released into circulation, where it correlates with measures of bone formation. The presence of 3 vitamin K-dependent residues is critical for osteocalcin's structure. In humans, the percentage of the circulating osteocalcin that is not γ-carboxylated (percent ucOC) is used as a biomarker of vitamin K status. In contrast, when ucOC is not corrected for total osteocalcin, the interpretation of this measure is confounded by osteoblastic activity, independent of vitamin K. Observational studies using percent ucOC have led to the conclusion that vitamin K insufficiency leads to age-related bone loss. However, clinical trials do not provide overall support for the suggestion that vitamin K supplementation of the general population will reduce bone loss or fracture risk. More recently, results from in vitro and in vivo studies using animal models indicate that ucOC is an active hormone with a positive role in glucose metabolism. By inference, vitamin K, which decreases ucOC, would have a detrimental effect. However, in humans this hypothesis is not supported by the limited data available, nor is it supported by what has been established regarding osteocalcin chemistry. In summary, the specific function of osteocalcin in bone and glucose metabolism has yet to be elucidated.
Hwang YC, Jee JH, Jeong IK, Ahn KJ, Chung HY, Lee MK. Circulating osteocalcin level is not associated with incident type 2 diabetes in middle-aged male subjects: mean 8.4-year retrospective follow-up study. Diabetes Care. 2012;35:1919–24.
Human studies suggest that osteocalcin is associated with bone and energy metabolism. This study was to determine whether serum osteocalcin level is independently associated with the development of type 2 diabetes. A retrospective cohort study was performed of 1,229 nondiabetic men, aged 25-60 years, who were recruited from the Health Promotion Center, Samsung Medical Center, between January 1997 and December 1997. They were followed for 8.4 years. Incident type 2 diabetes occurred in 90 (7.3%) of the study subjects. Osteocalcin levels were inversely associated with the presence of obesity, dyslipidemia, inflammation, and metabolic syndrome. Despite baseline associations with favorable metabolic parameters, the serum osteocalcin level was not associated with the development of type 2 diabetes in middle-aged males, only after.
Hwang Y-C, Jeong I-K, Ahn K-J, Chung H-Y. Circulating osteocalcin level is associated with improved glucose tolerance, insulin secretion and sensitivity independent of the plasma adiponectin level. Osteoporosis Int. 2012 Apr;23(4):1337-42.
The aims of this study were to determine whether or not osteocalcin is associated with the improved glucose tolerance and insulin secretion and sensitivity, and whether or not the association is dependent on the plasma adiponectin level in humans. Four hundred twenty-five subjects, 19–82 years of age (mean age, 53 years), were enrolled. The plasma levels of total osteocalcin were significantly different between the normal glucose tolerance, pre-diabetes, and diabetes groups. The glucose levels and homeostasis model assessment insulin resistance values varied inversely with the osteocalcin tertiles, and OGTT-based insulin secretion (HOMA-B%, disposition index. They concluded that circulating osteocalcin levels are associated with improved glucose tolerance and insulin secretion and sensitivity independent of the plasma adiponectin level in humans.
Ibarrola-Jurado N, Salas-Salvado J, Martinez-Gonzalez MA, Bullo M. Dietary phylloquinone intake and risk of type 2 diabetes in elderly subjects at high risk of cardiovascular disease. Am J Clin Nutr. 2012;96(5):1113–18.
This study analyzed the associations between dietary phylloquinone intake and type 2 diabetes in elderly subjects at high cardiovascular risk, from the Mediterranean Diet trial. They found that dietary phylloquinone at baseline was significantly lower in subjects who developed type 2 diabetes during the study. After adjustment for potential confounders, risk of incident diabetes was 17% lower for each additional intake of 100 μg phylloquinone/d. Moreover, subjects who increased their dietary intake of vitamin K during the follow-up had a 51% reduced risk of incident diabetes compared with subjects who decreased or did not change the amount of phylloquinone intake. They concluded that dietary phylloquinone intake is associated with reduced risk of type 2 diabetes.
Iki M, Tamaki J, Fujita Y, Kouda K, Yura A, Kadowaki E, et al. Serum undercarboxylated osteocalcin levels are inversely associated with glycemic status and insulin resistance in an elderly Japanese male population: Fujiwara-kyo Osteoporosis Risk in Men (FORMEN) Study. Osteoporosis International. 2012 Feb; 23(2):761-70.
Recent animal studies have demonstrated that undercarboxylated osteocalcin upregulates insulin secretion via osteoblast-insulin signaling. However, it remains unclear whether such a pathway exists in humans. This study looked at 2174 Japanese men in the Nara Prefecture. The results showed that both intact OC and ucOC levels showed significant inverse correlations with all outcome measures, even after adjusting for potential confounders. They concluded that levels of ucOC, but not iOC, were inversely associated with glycemic index and insulin resistance in a population of Japanese men.
Jia G, Stormont RM, Gangahar DM, Agrawal DK: Role of matrix Gla protein in angiotensin II-induced exacerbation of vascular calcification. Am J Physiol Heart Circ Physiol. 2012;303(5):H523-H532.
Karsenty G , Ferron M. The contribution of bone to whole-organism physiology. Nature. 2012;481:314–20.
The skeleton is an example of how a whole-organism approach to physiology can broaden the functions of a given organ, reveal connections of this organ with others such as the brain, pancreas and gut, and shed new light on the pathogenesis of degenerative diseases affecting multiple organs.
Kousteni S. FoxO1, the transcriptional chief of staff of energy metabolism. Bone. 2012;50(2):437–43.
Lee SW, Jo HH, Kim MR, You YO, Kim JH. Association between obesity, metabolic risks and serum osteocalcin level in postmenopausal women. Gynecological Endocrinology. 2012;28(6):472–77.
Osteocalcin, a marker of bone formation, is also known as a regulator of glucose and fat mass. The purpose of this study was to determine the association between obesity, metabolic risks and serum osteocalcin in postmenopausal women. Their study showed that serum osteocalcin has some significance as an indicator of metabolic risk, including abdominal obesity and insulin resistance. Bone as well as adipose tissue may be an active organ that regulates energy metabolism. A larger study will be needed to clarify the potential of osteocalcin as an indicator of cardiovascular disease.
Ngarmukos C, Chailurkit LO, Chanprasertyothin S, Hengprasith B, Sritara P, Ongphiphadhanakul B. A reduced serum level of total osteocalcin in men predicts the development of diabetes in a long-term follow-up cohort. Clin Endocrinol (Oxf). 2012;77:42–46.
Osteocalcin (OC), an osteoblast-specific protein, has been demonstrated to affect glucose metabolism in both animals and humans. Studies in animals have shown an effect of undercarboxylated OC (ucOC) on beta-cell proliferation and insulin resistance. The aim of this study was to examine serum OC and its post-translational forms as potential biomarkers for future the development of type 2 diabetes. They studied 63 men without diabetes, and also a non-diabetes control group from the Electricity Generating Authority of Thailand (EGAT). The results indicated that circulating total OC was associated with incident diabetes in men.
Rossi A, Targher G, Zoppini G, Cicoira M, Bonapace S, Negri C, et al. Aortic and mitral annular calcifications are predictive of all-cause and cardiovascular mortality in patients with type 2 diabetes. Diabetes Care. 2012;35(8):1781-86.
Sarkar PD, Choudhury AB. Relationship of serum osteocalcin levels with blood glucose, insulin resistance and lipid profile in central Indian men with type 2 diabetes. Arch Physiol Biochem. 2012 Dec;118(5):260-4.
The objective was to assess the relationship of serum osteocalcin levels with blood glucose, insulin resistance and lipid profile in central Indian men with type 2 diabetes. After adjustment for age and BMI, osteocalcin levels were negatively correlated with fasting plasma glucose (p = 0.0004), fasting insulin (p = 0.0311), HOMA-IR (p = 0.0023), and triglycerides (p = 0.0095), and positively correlated with high density lipoprotein (HDL)-cholesterol (p = 0.0042) in type 2 diabetic patients. They concluded that osteocalcin may play a protective role in the pathogenesis of type 2 diabetes, not only through direct involvement in glucose homeostasis, but also through improving lipid profile.
Schwetz V, Pieber T, Obermayer-Pietsch B. The endocrine role of the skeleton: background and clinical evidence. Eur J Endocrinol. 2012 June;166:959-67.
Based on the observation that diabetes, obesity, and hypogonadism influence bone metabolism, the existence of a feedback loop and a common regulation was postulated and an endocrine role ascribed to the skeleton. Interventional studies, to date only performed in murine models, have shown positive effects of OC administration on energy metabolism. Whether bone tissue has an even further-reaching endocrine role remains to be elucidated.
Silaghi CN, Fodor D, Craciun AM. Circulating matrix Gla protein: A potential tool to identify minor carotid stenosis with calcification in a risk population. Clin Chemi and Lab Med. 2012 (Sep);51(5):1115-23.
Carotid calcification is an independent marker for future ischemic events, which are more frequently encountered in postmenopausal women as the prevalence of type 2 diabetes mellitus (T2DM) and hypertension (HT) increases. Matrix Gla protein (MGP) is a major inhibitor of vascular calcification. Here, we report on the prospect of serum MGP to become an identifying tool for minor carotid stenosis (minCAS) with calcification in a risk population. They found higher circulating MGP levels could help identify minCAS with calcification in a relatively homogenous risk population (i.e., postmenopausal women), regardless of underlying cardiovascular risk factors.
Westenfeld R, Krueger T, Schlieper G, Cranenburg EC, Magdeleyns EJ, Heidenreich S, et al. Effect of vitamin K2 supplementation on functional vitamin K deficiency in hemodialysis patients: a randomized trial. Am J Kidney Dis. 2012;59(2):186-95.
This study confirmed that most hemodialysis patients have a functional vitamin K deficiency. More importantly, it is the first study showing that inactive MGP levels can be decreased markedly by daily vitamin K2 supplementation.
Yoshizawa T. Diabetes mellitus and osteoporosis. Insulin signaling and bone/glucose/energy metabolism. Clinical Calcium. 2012;22(9):1367–73.
Insulin signaling in osteoblast cells activated osteocalcin embedded in bone, by stimulating resorption activity in the osteocalsts. This activated osteocalcin acts as a hormone and regulates glucose metabolism through increasing insulin secretion from the pancreas. It will be important to study the interaction of the bone and glucose metabolism in the future, in a clinical study.
Alfadda AA, Masood A, Shaik SM, Dekhil H, Goran M. Association between Osteocalcin, Metabolic Syndrome, and Cardiovascular Risk Factors: Role of Total and Undercarboxylated Osteocalcin in Patients with Type 2 Diabetes. Int J of Endocrinology. 2013 (2013):197519.
Studies have demonstrated that total osteocalcin (TOC) is associated with metabolic syndrome (MetS) and therefore might influence the risk of cardiovascular disease in humans. Undercarboxylated osteocalcin (uOC) regulates insulin secretion and sensitivity in mice, but its relation to MetS in humans is unclear. We aimed to determine whether uOC is related to MetS and/or its individual components and other cardiovascular risk factors in patients with type 2 diabetes mellitus (T2DM), and whether TOC and uOC have utility in predicting the cardiovascular risk. Both TOC and uOC were significantly lower in patients with MetS compared to those without MetS, independent of body mass index. In patients with MetS, uOC was significantly and positively correlated with HDL cholesterol, while TOC was significantly and negatively correlated with serum triglycerides. We report for the first time that uOC is related to lipid indices in patients with T2DM.
Aoki A, Murata M, Asano T, Ikoma A, Sasaki M, Saito T, et al. Association of serum osteoprotegerin with vascular calcification in patients with type 2 diabetes. Cardiovasc Diabetol. 2013;12:11.
Osteoprotegerin is produced by osteoblasts and is an important regulator in osteoclast function. These findings suggest that elevated serum osteoprotegerin may be involved in vascular calcification independently of progression of diabetic nephropathy in patients with type 2 diabetes.
Bhattoa HP, Onyeka U, Kalina E, Balogh A, Paragh G, Antal-Szalmas P, et al. Bone metabolism and the 10-year probability of hip fracture and a major osteoporotic fracture using the country-specific FRAX algorithm in men over 50 years of age with type 2 diabetes mellitus: A case-control study. Clin Rheumatol. 2013;32:1161–67.
Booth S. L., Centi A., Smith S. R., Gundberg C. The role of osteocalcin in human glucose metabolism: marker or mediator? Nature REviews Endocrinology. 2013;9(1):43–55.
Increasing evidence supports an association between the skeleton and energy metabolism. These interactions are mediated by a variety of hormones, cytokines and nutrients. Here, the evidence for a role of osteocalcin in the regulation of glucose metabolism in humans is reviewed. Osteocalcin is a bone matrix protein that regulates hydroxyapatite size and shape through its vitamin-K-dependent, γ-carboxylated form. The concentration of osteocalcin in the circulation is a measure of bone formation. The undercarboxylated form of osteocalcin is active in glucose metabolism in mice. Total serum osteocalcin concentrations in humans are inversely associated with measures of glucose metabolism; however, human data are inconclusive with regard to the role of uncarboxylated osteocalcin in glucose metabolism. Carefully designed studies are required to define the role of osteocalcin and its carboxylated or undercarboxylated forms in the regulation of glucose metabolism in humans.
Boxma PY, van den Berg E, Geleijnse JM, Laverman GD, Schurgers LJ, Vermeer C, et al. Vitamin k intake and plasma desphospho-uncarboxylated matrix Gla-protein levels in kidney transplant recipients. PLoS One. 2013, 7(10):e47991. 
Vitamin K is essential for activation of γ-carboxyglutamate (Gla)-proteins including the vascular calcification inhibitor matrix Gla-protein (MGP). Insufficient vitamin K intake leads to production of uncarboxylated, mostly inactive proteins and contributes to an increased cardiovascular risk. In kidney transplant recipients, cardiovascular risk is high but vitamin K intake and status have not been defined. We investigated dietary vitamin K intake, vascular vitamin K status and its determinants in kidney transplant recipients. Total vitamin K intake was below the recommended level in 50% of patients. In a considerable part of the kidney transplant population, vitamin K intake is too low for maximal carboxylation of vascular MGP. The high dp-ucMGP levels may result in an increased risk for arterial calcification.
Brennan-Speranza TC, Henneicke H, Gasparini SJ, Blankenstein KI, Heinevetter U, Cogger VC, et al. Osteoblasts mediate the adverse effects of glucocorticoids on fuel metabolism. J Clin Invest. 2013;122:4172-89.
Chen H, Li X, Yue R, Ren X, Zhang X, Ni A. The effects of diabetes mellitus and diabetic nephropathy on bone and mineral metabolism in T2DM patients. Diabetes Res Clin Pract. 2013;100:272–6.
This study assessed the effects of both diabetes mellitus and diabetic nephropathy on bone mineral metabolism in patients with type 2 diabetes mellitus (T2DM). Compared with the nondiabetic controls, patients in both the diabetic and the nondiabetic group had decreased serum osteocalcin (BGP) and bone mineral density (BMD) while serum alkaline phosphatase (ALP) and urinary hydroxyproline (HOP) were increased. They concluded that patients with T2DM show an imbalance of bone mineral metabolism, and co-existence of nephropathy tends to aggravate this. Serum osteocalcin and 24-h hydroxyproline may be considered useful biochemical markers for monitoring possible bone mineral metabolism disorder in T2DM patients.
Dalmeijer GW, van der Schouw YT, Magdeleyns EJ, Vermeer C, Verschuren WM, Boer JM, et al. Matrix Gla protein species and risk of cardiovascular events in type 2 diabetic patients. Diabetes Care. 2013 Nov;36(11):3766-71.
This study investigates the relationship of circulating matrix Gla protein (MGP) species with incident cardiovascular disease (CVD) or coronary heart disease (CHD) in type 2 diabetic patients, from a cohort of 40.011 Dutch men and women. They found that high uncarboxylated MGP levels were associated with increased CVD risk among type 2 diabetic patients, especially with the subtypes PAD and heart failure, while other MGP species were not related to CVD risk. These results suggest that a poor vitamin K status is associated with increased CVD risk.
Diazo-Lopez A, Bullo M, Juanola-Falgarona M, Martinez-Gonzalez MA, Estruch R, Covas MI. Reduced serum concentrations of carboxylated and undercarboxylated osteocalcin are associated with risk of developing type 2 diabetes mellitus in a high cardiovascular risk population: a nested case-control study. J Clin Endocrinol Metab. 2013 Nov;98(11):4524-31.
Because it has been suggested that osteocalcin (OC), an osteoblast-derived hormone, is a new link between bone and glucose metabolism, we tested whether serum carboxylated osteocalcin (cOC) and undercarboxylated osteocalcin (ucOC) levels are independently associated with the development of type 2 diabetes in subjects at high cardiovascular risk. The subjects came from the the Prevención con Dieta Mediterránea (PREDIMED study. The results indicated that low concentrations of serum cOC and ucOC were strongly associated with an increased risk of incident diabetes, and that carboxylated osteocalcin but not uncarboxylated osteocalcin was inversely and significantly associated with insulin resistance and fasting glucose concentration.
Doyon M, Mathieu P, Moreau P. Decreased expression of gamma-carboxylase in diabetes-associated arterial stiffness: Impact on matrix Gla protein. Cardiovasc Res. 2013 Feb 1;97(2):331-8.
Arterial stiffness is accelerated in type 1 diabetic patients. Medial artery calcification (MAC) contributes to the development of arterial stiffness. This study aimed to evaluate the hypothesis that diabetes reduces the γ-carboxylation of MGP in the aortic wall, leading to increased vascular calcification, and the role of γ-carboxylase and VKOR in this γ-carboxylation deficit. Type 1 diabetes was induced in male Wistar rats. Ex vivo experiments showed that vitamin K supplementation prevented the glucose-induced decrease in γ-carboxylase expression. Our results suggest that reduced cMGP, through an impaired expression of γ-carboxylase, is involved in the early development of MAC in diabetes, and therefore, in the acceleration of arterial stiffness. A defect in vitamin K uptake by target cells could also be involved.
Ferrari S. Diabetes and osteoporosis. Rev Mud Suisse. 2013;9:1256, 1258-59.
Furusyo N, Ihara T, Hayashi T, Ikezaki H, Toyoda K, Ogawa E, et al. The serum undercarboxylated osteocalcin level and the diet of a Japanese population: results from the Kyushu and Okinawa Population Study (KOPS). Endocrine. 2013 Jun;43(3):635-42.
The elevated serum undercarboxylated osteocalcin (ucOC) level is related to osteoporosis. In Japan, vitamin K intake is lower, and the incidence of hip fractures noticeably higher in northern Kyushu than in other areas. The study was done to determine the serum ucOC levels in a Japanese population and its association with diet and glucose metabolism. Their study indicates that the serum ucOC decreases with age in men, increases postmenopausally in women, and correlates inversely with dietary consumption of certain foods and with fasting glucose and HbA1c level.
Gower BA, Pollack NK, Casazza K, Clemens TL, Goree LL, Granger WM. Association of total and undercarboxylated osteocalcin with peripheral and hepatic insulin sensitivity and β-cell function in overweight adults. J Clin Endocrinol Metab. 2013 Jul;98(7):E1173-80.
Animal research has provided evidence that uncarboxylated osteocalcin (ucOC) has unique effects on insulin secretion and action. However, results using human research participants have been inconsistent and often have implicated carboxylated OC rather than ucOC as being associated with insulin sensitivity. The study aimed to determine whether total OC and unOC are independently associated with insulin sensitivity and b-cell response in overweight/obese adults. They found that in overweight/obese individuals, that total OC was independently and positively associated with insulin sensitivity. The observations suggest that any potential effect of OC on insulin sensitivity may occur at skeletal muscle rather than the liver.
Garcia-Martin A, Reyes-Garcia R, Avila-Rubia V, Munoz-Torres M. Osteocalcin: a link between bone homeostasis and energy metabolism. Endocrinol Nutr. 2013;60:260-3.
Research in animal models has demonstrated the role of osteocalcin, a bone formation marker, in regulation of energy metabolism. Those studies have led to a new concept of the bone acting as an endocrine organ by secreting osteocalcin, which acts by increasing insulin secretion, lowering plasma glucose, and increasing insulin sensitivity and energy expenditure. Results in humans have been conflicting. On the other hand, antiresorptive drugs used against osteoporosis decrease osteocalcin levels, while anabolic drugs increase osteocalcin levels. However, the effects of these therapies on energy metabolism have not been investigated.
Juanola-Falgarona M, Salas-Salvado J, Estruch R, Portillo MP, Casas R, Miranda J, Martinez-Gonzalez MA, Bullo M. Association between dietary phylloquinone intake and peripheral metabolic risk markers related to insulin resistance and diabetes in elderly subjects at high cardiovascular risk. Cardiovas Diabetol. 2013 Jan 8;12:7.
This study assessed the associations between dietary intake of vitamin K and peripheral adipokines and other metabolic risk markers related to insulin resistance and type 2 diabetes mellitus on 510 elderly participants recruited in the PREDIMED centers in Spain. After 1-year of follow-up, the results show that dietary phylloquinone intake is associated with an improvement of cytokines and other markers related to insulin resistance and diabetes, thus extending the potential protection by dietary phylloquinone on chronic inflammatory diseases.
Kanazawa I., Sugimoto T. The relationship between bone and glucose/lipid metabolism. Clinical Calcium. 2013;23(2):181-88.
Fracture risks are increased in patients with lifestyle-related diseases such as diabetes mellitus and dyslipidemia. Bone has been recognized as an endocrine organ to regulate glucose and fat metabolism. It has been revealed that osteocalcin, which is secreted from bone tissue into the circulation, has a hormonal function in glucose and fat metabolism.
Kramer CK, Zinman B, Gross JL, Canani LH, Rodrigues TC, Azevedo MJ, et al. Coronary artery calcium score prediction of all cause mortality and cardiovascular events in people with type 2 diabetes: systematic review and meta-analysis. BMJ. 2013 Mar;346:f1654.
This article reviewed 8 observational studies on the association of the coronary artery calcium score with all cause mortality and cardiovascular events in people with type 2 diabetes. They found that in people with type 2 diabetes, a coronary artery calcium score predicts all cause mortality or cardiovascular events or both, with high sensitivity. Clinically, the finding of a coronary artery calcium score of <10 may facilitate risk stratification by enabling the identification of people at low risk within this high risk population.
Kulkarni VK, Upase DP, Doung YA, Jadhav SS, Bhave AA, Mehta DS, et al. The effect of vitamin K2-7 in peripheral neuropathy due to Vitamin B12 deficiency and/or diabetes mellitus: A preliminary study. The Indian Practitioner. 2013 Oct;66(10):625-29.
This preliminary study showed that vitamin MK7 at a dose of 100 mcg twice a day for 8 weeks was well tolerated and had therapeutic activity for the symptoms of peripheral neuropathy.
Lacombe J, Karsenty G, Ferron G. In vivo analysis of the contribution of bone resorption to the control of glucose metabolism in mice. Mol Metab. 2013 Nov;2(4):498-504.
Osteocalcin is a hormone produced in bones by osteoblasts and regulates energy metabolism. While osteocalcin exists in two forms, γ-carboxylated and undercarboxylated, only the latter appears to function as a hormone in vivo. It has been proposed recently that osteoclasts, the bone-resorbing cells, are responsible for decarboxylating, i.e. activating osteocalcin. To address the role of osteoclasts in the maintenance of energy metabolism we analyzed mutant mouse strains harboring either an increase or a decrease in osteoclasts number. The results support the notion that osteoclasts are controlling glucose metabolism at least in part through the regulation of osteocalcin decarboxylation.
Liu, Toy, Wong, Tan, Tavintharan, Sum CF. Elevated undercarboxylated and reduced carboxylated osteocalcin are associated with metabolic syndrome in middle age Asian females. Experimental and Clinic Endocrinol & Diabetes. 2013:121(6):329-33.
Accumulating data suggest that bone plays a role in energy metabolism through decarboxylation of osteocalcin. This study aimed to study the association of circulating under-carboxylated osteocalcin (UC-OCN) and carboxylated osteocalcin (C-OCN) with metabolic syndrome in middle aged Asian population. They found that circulating UC-OCN was increased in subjects with metabolic syndrome. Further analysis revealed that changes in both UC-OCN and C-OCN occurred primarily among females with metabolic syndrome. Interestingly, neither forms of OCN differed significantly between individuals with and without metabolic syndrome in males. Circulating UC-OCN was increased while C-OCN was decreased in treatment-naïve females with metabolic syndrome.
Neve A, Corrado A, Cantatore FP. Osteocalcin: Skeletal and extra-skeletal effects. J Cellu Physio. 2013 June;228(6):1149-53.
This review highlights the recent studies concerning skeletal and extraâ€skeletal effects of OC, a vitamin Kâ€dependent protein secreted in the late stage of osteoblasts differentiation. Recently the metabolic activity of OC, restricted to the unâ€carboxylated form, has been demonstrated in osteoblastâ€specific knockout mice. This effect is mediated by the regulation of pancreatic βâ€cell proliferation, insulin secretion, and adiponectin production by adipose tissue and leads to the regulation of glucose metabolism and fat mass.
Oosterwerff MM, van Schoor NM, Lips P, Eekhoff EM. Osteocalcin as a predictor of the metabolic syndrome in older persons: a population-based study. Clin Endocrinol (Oxf). 2013 Feb;78(2):242-7.
This study investigated the association of plasma osteocalcin levels with the metabolic syndrome in a community-dwelling cohort of older persons in the Netherlands. Data were used from the Longitudinal Aging Study Amsterdam (LASA), an ongoing multidisciplinary cohort study in a representative sample of the older Dutch population (≥65 years old). A total of 1284 subjects (629 men and 655 women) between the age of 65 and 88 years participated in this study. Among the participants, the prevalence of the metabolic syndrome was 37·1%. Plasma osteocalcin was inversely associated with the metabolic syndrome. Low plasma osteocalcin levels are strongly associated with the metabolic syndrome in an older community-dwelling population.
Patti A, Gennari L, Merlotti D, Dotta F, Nuti R. Endocrine Actions of Osteocalcin. International Journal of Endocrinology. 2013;2013:846480.
Osteocalcin is the most abundant noncollagenous protein of bone matrix. Once transcribed, this protein undergoes posttranslational modifications within osteoblastic cells before its secretion, including the carboxylation of three glutamic residues in glutamic acid, which is essential for it to bind and be deposited in the matrix of bone. Provocative data from experimental observations in mice showed that the circulating undercarboxylated fraction of osteocalcin increases insulin secretion and sensitivity, lowers blood glucose, and decreases visceral fat in both genders, while it enhances testosterone production by the testes in males. Moreover, both total and undercarboxylated osteocalcins increase following physical activity with potential positive effects on glucose tolerance.
Sardana M, Vasim, Varakantam S, Kewan U, Tariq A, Koppula MR, et al. Inactive matrix Gla-protein and arterial stiffness in Type 2 diabetes mellitus. Am J Hypertens. 2017 Feb;30(2):196-201.
Large arterial stiffness is increased in diabetes and causes an excessive pulsatile load to the heart and to the microvasculature. This study hypothesized that levels of inactive MGP are related to arterial stiffness in type 2 diabetes. Their findings suggest that deficient vitamin K-dependent activation of MGP may lead to large artery stiffening, and supplementing with vitamin K may help patients with diabetes.
Schurgers LJ, Uitto J, Reutelingsperger CP. Vitamin K-dependent carboxylation of matrix Gla-protein: A crucial switch to control ectopic mineralization. Trends Mol Med. 2013;19(4):217-26.
Sheng L, Cao W, Cha B, Chen Z, Wang F, Liu J: Serum osteocalcin level and its association with carotid atherosclerosis in patients with type 2 diabetes. Cardiovasc Diabetol. 2013;12:22.
They performed a cross-sectional community-based looking at serum total osteocalcin in 382 men and 435 postmenopausal women as well as the carotid artery intima-media thickness (IMT) and carotid plaques (PLQ). Osteocalcin levels were associated inversely with age, fasting serum insulin, HOMA-IR, ALT, triglycerides, total cholesterol, LDL- cholesterol, CRP (all P<0.001) and positively with adiponectin and HOMA-B (all P<0.05). They concluded that serum osteocalcin levels is an independent risk factor for carotid atherosclerosis in patients with type 2 diabetes.
Silaghi CN, Fodor D, Craciun AM: Circulating matrix Gla protein: a potential tool to identify minor carotid stenosis with calcification in a risk population. Clin Chem Lab Med. 2013, 51(5):1115-23.
Vella A, Kumar R. Osteocalcin and the regulation of glucose metabolism. Clin Rev Bone Miner Metab. 2013 Mar:11(1):11-16.
Uncarboxylated osteocalcin enhances insulin and adiponectin release and improves glucose tolerance in mice. Data in humans do not unequivocally support a role for osteocalcin in glucose homeostasis. Interventional studies in humans, designed to detect small changes in insulin secretion and action attributable to changes in uncarboxylated osteocalcin, will be required to reliably detect effects of osteocalcin on glucose metabolism and to better understand its interaction with adiposity and adipokines, which are cells secreted by fat tissue.
Wang Q, Zhang B, Xu Y, Xu H, Zhang N. The relationship between serum osteocalcin concentration and glucose metabolism in patients with Type 2 Diabetes Mellitus. Int J of Endocrinology. 2013;2013:842598.
Studied the correlations between osteocalcin and glucose metabolism in patients with type 2 diabetes. They found no significant correlation between osteocalcin and measures of insulin resistance. They also found that total osteocalcin was an independent related factor of HbA1c levels (a measure of blood glucose levels). Decreased total osteocalcin and undercarboxylated osteocalcin are related to the exacerbation of glucose metabolism disorder.
Woeckel V. J., Bruedigam C., Koedam M., Chiba H., van der Eerden B. C. J., van Leeuwen J. P. T. M. 1α,25-Dihydroxyvitamin D3 and rosiglitazone synergistically enhance osteoblast-mediated mineralization. Gene. 2013;512(2):438–443.
Chen X, Wu Y, Liu L, Tian H, Yu . Osteocalcin is inversely associated with glucose levels in middle –aged Tibetanmen with different degrees of glucose tolerance. Diabetes Metab Res Rev. 2014;30:476-82.
The objective of this study was to investigate the associations of serum total osteocalcin (tOC) and undercarboxylated osteocalcin (ucOC) with glucose and lipid metabolism in Chinese indigenous Tibetans with different degrees of glucose tolerance. In this study, 160 middle-aged Tibetan men were involved, including 46 subjects with normal glucose tolerance (NGT), 52 subjects with impaired glucose regulation (IGR) and 62 subjects with type 2 diabetes. The data support a link between osteocalcin and glucose metabolism in middle-aged Tibetan men. The improved glucose tolerance exerted by tOC may be related to improved insulin sensitivity rather than improved β-cell function.
Confavreux CB, Szulc P, Casey R, Varennes A, Goudable J, Chapurlat RD. Lower serum osteocalcin is associated with more severe metabolic syndrome in elderly men from the MINOS cohort. European J of Endocrinology. 2014;171:275-83.
Bone has emerged as an endocrine organ regulating energy metabolism through secretion of osteocalcin. In epidemiological studies, presence of metabolic syndrome (MetS) was associated with lower osteocalcin level. In this study, they evaluated whether osteocalcin level was associated with MetS severity in men. Thirty percent of the men had MetS. In patients with MetS, the higher the number of MetS traits were present, the lower was the average osteocalcin level. They concluded that in older Caucasian men, total osteocalcin level was associated with MetS severity. Osteocalcin was more strongly associated with MetS severity than other bone turnover markers.
Farr JN, Drake MT, Amin S, Melton LJ 3rd, McCready LK, Khosla S. In Vivo assessment of bone quality in postmenopausal women with type 2 diabetes. J Bone Miner Res. 2014 Apr;29(4):787-95.
A lthough patients with type 2 diabetes (T2D) are at significant risk for well-recognized diabetic complications, including macrovascular disease, retinopathy, nephropathy, and neuropathy, it is also clear that T2D patients are at increased risk for fragility fractures. Furthermore, our results confirm previous studies demonstrating low bone turnover in patients with T2D and highlight the potential detrimental effects of prolonged hyperglycemia on bone quality. Thus, the skeleton needs to be recognized as another important target tissue subject to diabetic complications.
Ferron M, Lacombe J. Regulation of energy metabolism by the skeleton: osteocalcin and beyond. Arch Biochem Biophys. 2014 Nov; 561:137- 46.
The skeleton has recently emerged as an endocrine organ implicated in the regulation of glucose and energy metabolism. This function of bone is mediated, at least in part, by osteocalcin, an osteoblast-derived protein acting as a hormone stimulating insulin sensitivity, insulin secretion and energy expenditure. Osteocalcin secretion and bioactivity is in turn regulated by several hormonal cues including insulin, leptin, the sympathetic nervous system and glucocorticoids. Studies in mice suggest that osteocalcin could represent a viable therapeutic approach for the treatment of obesity and insulin resistance. In this review, we summarize the current knowledge on osteocalcin functions, its various modes of action and the mechanisms implicated in the control of this hormone.
Hill HS, Grams J, Walton RG, Liu DR Moellering DR, Garvey WT. Carboxylated and uncarboxylated forms of osteocalcin directly modulate the glucose transport system and inflammation in adipocytes. Horm Metab Res. 2014;46(05):341-7.
Osteocalcin is secreted by osteoblasts and improves insulin sensitivity in vivo, although mechanisms remain unclear. They tested the hypothesis that osteocalcin directly modulates cell biology in insulin-targeted peripheral tissues. They found that both carboxylated and uncarboxylated osteocalcin directly increase glucose transport in adipocytes and muscle cells, while suppressing proinflammatory cytokine secretion and stimulating interleukin 10 and adiponectin release. Thus, these results provide a mechanism for the insulin-sensitizing effects of osteocalcin and help elucidate the role that bone plays in regulating systemic metabolism.
Giovanni L, Silvia P, Livio L, Giuseppe B. A four-season molecule: osteocalcin. Updates in its physiological Roles. Endocrine. 2015;48:394–404.
Osteocalcin (OC) has a regulatory role in mineralization and it is considered a marker of bone cell metabolism. Recent findings evidenced new extra-skeletal roles for OC, depicting it as a real hormone. OC exists in different forms based on the degree of carboxylation. Indeed, OC has three glutamic acid residues, in position 17, 21, and 24, which are subject to γ-carboxylation, through the action of a vitamin K-dependent γ-glutamyl carboxytransferase. The degree of carboxylation, and thus the negative charge density, determines the affinity for the calcium ions deposited in the extracellular matrix of the bone. The modulation of the carboxylation could, thus, represent the mechanism by which the body controls the circulating levels, and hence the hormonal function, of OC. There are evidences linking OC, and the bone metabolism, with a series of endocrine (glucose metabolism, energy metabolism, fertility) physiological (muscle activity) and pathological functions (ectopic calcification). This study is to gives a full overview of the physiological roles of OC by collecting the newest experimental findings on this intriguing molecule.
Klein GL. Insulin and bone: Recent developments. World J Diabetes. 2014 Feb 15;5(1):14-16.
There is specific evidence that insulin may work to stimulate osteoblast differentiation, which in turn would enhance production of osteocalcin, that can stimulate pancreatic β cell proliferation and skeletal muscle insulin sensitivity. It is uncertain whether insulin stimulates bone directly or indirectly by increasing muscle work and therefore skeletal loading. We raise the question of the sequence of events that occurs with insulin resistance, such as type 2 diabetes. Evidence to date suggests that these patients have lower serum concentrations of osteocalcin, perhaps reduced skeletal loading, and reduced bone strength as evidenced by micro-indentation studies.
Liabeuf S, Bourron O, Olivier B, Vermeer C, Theuwissen E, Magdeleyns E, et al. Vascular calcification in patients with type 2 diabetes: the involvement of matrix Gla protein. Cardiovasc Diabetol. 2014;13(1):85.
Matrix Gla protein (MGP) is an important inhibitor of calcification. The objective of the present study of patients with type 2 diabetes and normal or slightly altered kidney function was to evaluate levels of inactive, dephospho-uncarboxylated MGP(dp-ucMGP) and total uncarboxylated MGP(t-ucMGP) and assess their links with biological and clinical parameters (including peripheral vascular calcification). When the study population was divided according to the median peripheral arterial calcification score, patients with the higher score displayed significantly lower t-ucMGP and significantly higher dp-ucMGP levels. High dp-ucMGP levels were independently associated with below-knee arterial calcification score in patients with type 2 diabetes and normal or slightly altered kidney function.
van de Peppel J, van Leeuwen JPTM. Vitamin D and gene networks in human osteoblasts. Frontiers in Physiology. 2014;5, article 137.
Sai Varsha MKN, Raman T, Manikandan R, Dhanasekaran G. Hypoglycemic action of vitamin K1 protects against earlyâ€onset diabetic nephropathy in streptozotocinâ€induced rats. Nutrition. 2015;31:1284–1292.
Vitamin K is a potent regulator of vascular dynamics and prevents vascular calcification. Vitamin K is increasingly being recognized for its antioxidant and antiinflammatory properties. The aim of this study was to determine whether the hypoglycemic action of vitamin K1 could inhibit early-onset diabetic nephropathy in a streptozotocin-induced rat kidney. They found that treatment of diabetic rats with vitamin K1 resulted in a decrease in blood glucose and prevented microalbuminuria. Vitamin K1 also reduced oxidative stress and protected renal physiology. Vitamin K1 could be an important nutrient based interventional strategy for early onset diabetic nephropathy.
Sai Varsha, M.K.; Raman, T.; Manikandan, R. Inhibition of diabetic-cataract by vitamin K1 involves modulation of hyperglycemia-induced alterations to lens calcium homeostasis. Eye Res.2014, 128, 73–82.
Wei J, Hanna T, Suda N, Karsenty G, Ducy P. Osteocalcin promotes b-cell proliferation during development and adulthood through Gprc6a. Diabetes. 2014 Mar;63(3):1021-31.
Expanding β-cell mass through β-cell proliferation is considered a potential therapeutic approach to treat β-cell failure in diabetic patients. A necessary step toward achieving this goal is to identify signaling pathways that regulate β-cell proliferation in vivo. Here we show that osteocalcin, a bone-derived hormone, regulates β-cell replication in a cyclin D1-dependent manner by signaling through the Gprc6a receptor expressed in these cells. This study extends the endocrine role of osteocalcin to the developmental period and establishes osteocalcin/Gprc6a signaling as a major regulator of β-cell endowment that can become a potential target for β-cell proliferative therapies.
Zanatta LCB, Boguszewski CL, Borba VZC, Kulak CAM. Osteocalcin, energy and glucose metabolism. Arq Bras Endocrinol Metab. 2014 July;58(5):444-51.
Osteocalcin is a bone matrix protein that has been associated with several hormonal actions on energy and glucose metabolism. Animal and experimental models have shown that osteocalcin is released into the bloodstream and exerts biological effects on pancreatic beta cells and adipose tissue. Undercarboxylated osteocalcin is the hormonally active isoform and stimulates insulin secretion and enhances insulin sensitivity in adipose tissue and muscle. Insulin and leptin, in turn, act on bone tissue, modulating the osteocalcin secretion, in a traditional feedback mechanism that places the skeleton as a true endocrine organ. Further studies are required to elucidate the role of osteocalcin in the regulation of glucose and energy metabolism in humans and its potential therapeutic implications in diabetes, obesity and metabolic syndrome.
Brennan-Speranza TC, Conigrave AD. Osteocalcin: An osteoblast-derived polypeptide hormone that modulates whole body energy metabolism. Calcified Tissue International. 2015 Jan;96(1):1-10.
Osteocalcin is a bone-specific protein that is used as a serum marker of bone turnover. Recent evidence indicates that osteocalcin plays a previously unsuspected role in the control of energy metabolism. Thus, osteocalcin-deficient mice have a profoundly deranged metabolic phenotype that includes insulin resistance, glucose intolerance and abnormal fat deposition. Additionally, osteocalcin administration in mice improves insulin sensitivity and decreases fat pad mass and serum triglyceride levels. The role of osteocalcin in human macronutrient metabolism is less clear but recent studies report positive correlations between serum osteocalcin levels and established indices of metabolic health. Herein, we review key physiological functions of osteocalcin, focussing on the roles of osteocalcin in the modulation of macronutrient metabolism, male reproductive function and foetal brain development.
Dam V, Dalmeijer GW, Vermeer C, Drummen NE, Knapen MH, van der Schouw YT, et al. Association between vitamin K and the Metabolic Syndrome: A 10-year follow-up study in adults. J Clin Endocrinol Metabl. 2015 Jun;100(6):2472-79.
The Metabolic Syndrome (MetS) is a cluster of metabolic abnormalities and is associated with increased risk of diabetes and cardiovascular diseases. Phylloquinone, menaquinones, and vitamin K status are associated with several components of MetS, but the association with MetS has hardly been studied to date. This study examined whether the intake and/or status of vitamin K is associated with MetS and its components. The study comprised two cohorts, one of 402 women and one of 400 men (age 40-80 years). At followup, 625 participants were still alive and willing to participate. The study shows that a high intake of menaquinones and a high vitamin K status are associated with lower occurrence of MetS.
Ferron M, Lacombe J, Germain A, Oury F, Karsenty G. GGCS and VKORC1 inhibit osteocalcin endocrine functions. JCB. 2015;208(6):761-76.
Osteocalcin (OCN) is an osteoblast-derived hormone favoring glucose homeostasis, energy expenditure, male fertility, brain development, and cognition. Before being secreted by osteoblasts in the bone extracellular matrix, OCN is γ-carboxylated. This study genetically and biochemically delineates the functions of the enzymes required for OCN modification and demonstrates that it is the uncarboxylated form of OCN that acts as a hormone.
Grober U, Reichrath J, Holick, MF, Kisters, K. Vitamin K: an old vitamin in a new perspective. Dermato-Endocrinology. 2015;6(1): e968490. doi:10.4161/19381972.2014.968490
Vitamin K is known to be important for blood coagulation. Current research increasingly indicates that the antihaemorrhagic vitamin has a considerable benefit in the prevention and treatment of bone and vascular disease. Vitamin K1 (phylloquinone) is more abundant in foods but less bioactive than the vitamin K2 menaquinones (especially MK-7, menaquinone-7). Along with coagulation factors, protein C and protein S, osteocalcin (OC), matrix Gla protein (MGP), periostin, Gas6, and other vitamin K-dependent (VKD) proteins support calcium homeostasis, inhibit vessel wall calcification, support endothelial integrity, facilitate bone mineralization, are involved in tissue renewal and cell growth control, and have numerous other effects.
Jiao H, Xiao E, Graes DT. Diabetes and its effect on bone and fracture healing. Curr Osteoporos Rep. 2015 Oct;13(5):327-35.
Diabetes mellitus is a metabolic disorder that increases fracture risk, interferes with bone formation, and impairs fracture healing. Type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM) both increase fracture risk and have several common features that affect the bone. These factors affect both osteoblasts and osteoclasts leading to increased osteoclasts and reduced numbers of osteoblasts and bone formation. In addition to fracture healing, T1DM and T2DM impair bone formation under conditions of perturbation such as bacteria-induced periodontal bone loss by increasing osteoblast apoptosis and reducing expression of factors that stimulate osteoblasts such as BMPs and growth factors.
Kanazawa I. Osteocalcin as a hormone regulating glucose metabolism. World J Diabetes. 2015 Dec;6(18):1345-54.
The number of patients with osteoporosis and diabetes is rapidly increasing all over the world. Bone has been recently recognized as an endocrine organ. Accumulating evidence has shown that osteocalcin, which is specifically expressed in osteoblasts and secreted into the circulation, regulates glucose homeostasis by stimulating insulin expression in pancreas and adiponectin expression in adipocytes, resulting in improving glucose intolerance. On the other hand, insulin and adiponectin stimulate osteocalcin expression in osteoblasts, suggesting that positive feedforward loops exist among bone, pancreas, and adipose tissue. These findings suggest that bone metabolism and glucose metabolism are associated with each other through the action of osteocalcin. In this review, I describe the role of osteocalcin in the interaction among bone, pancreas, brain, adipose tissue, and muscle.
Lacombe J, Ferron M. Gamma-carboxylation regulates osteocalcin function. Oncotarget. 2015;6(2):19924-25.
Vitamin K (VK) serves as a co-factor for the γ-carboxylation of particular proteins. Carboxylation is critical for the function of many coagulation factors (prothrombin, factor IX, factor VII, etc), but is also implicated in the regulation of Matrix Gla Protein (MGP) that inhibits tissue mineralization and of osteocalcin that regulates glucose metabolism. Osteocalcin improves glucose handling by promoting insulin secretion by beta cells, and by favoring insulin sensitivity. So far the data on osteocalcin endocrine regulation support a model in which osteocalcin produced by osteoblasts is stored as a γ-carboxylated and inactive protein in the bone ECM, before being activated by decarboxylation during bone resorption. In a recent study they provide direct evidence demonstrating that vitamin K-dependent γ-carboxylation negatively regulates both the bioactivity and the bioavailability of osteocalcin and controls glucose metabolism.
Liu DM, Guo XA, Tong HJ, Tao B, Sun LH, Zhao LH, et al. Association between osteocalcin and glucose metabolism: a meta-analysis. Osteoporosis International. 2015 Dec;26(12):2823-33.
This meta-analysis aimed to investigate the associations between osteocalcin (Ocn) and fasting plasma glucose (FPG) and glycated hemoglobin A1c (HbA1c). A search was carried out using the databases of PubMed, ISI Web of Science, and the Cochrane library from 2007 to 2014 to identify related studies. A pooled effect size with 95 % confidence intervals (CI) was derived. This meta-analysis demonstrated that both unOcn and tOcn were similarly and negatively correlated with FPG and HbA1c in humans. The negative correlations between unOcn and glucose metabolism appear to be more pronounced in men than in women.
Magni P, Macchi C, Sirtori CR, Corsi Romanelli MM. Osteocalcin as a potential risk biomarkers for cardiovascular and metabolic diseases. Clin Chem Lab med. 2016 Feb 10; pii: /j/cclm.ahead-of-print/cclm-2015-0953/cclm-2015-0953.
Clear evidence supports a role for osteocalcin (OC) in the pathophysiology of cardiovascular (CV) lesions and CV risk, also in combination with metabolic changes, including type 2 diabetes mellitus (T2DM). Reduced OC levels are associated with greater incidence of pathological CV changes, like arterial and valvular calcification, coronary and carotid atherosclerosis and increased carotid intima-media thickness. Moreover, reduced circulating OC levels have been mostly associated with insulin resistance, metabolic syndrome or T2DM. Based on these observations, this review article will attempt to summarize the current evidence on the potential usefulness of circulating OC as a biomarker for CV and metabolic risk.
Okuyama H, Langsjoen PH, Hamazaki T, Ogushi Y, Hama R, Kobayashi T, Uchino H: Statins stimulate atherosclerosis and heart failure: pharmacological mechanisms. Expert Rev Clin Pharmacol 2015;8:189-199.
Oldknow KJ, MacRae VE, Farquharson C. Endocrine role of bone: recent and emerging perspectives beyond osteocalcin. J Endocrinol. 2015 Apr;225(1):R1-19.
Recent developments in endocrinology, made possible by the combination of mouse genetics, integrative physiology and clinical observations have resulted in rapid and unanticipated advances in the field of skeletal biology. Indeed, the skeleton, classically viewed as a structural scaffold necessary for mobility, and regulator of calcium–phosphorus homoeostasis has now been identified as an important regulator of male fertility and whole-body glucose metabolism, in addition to the classical insulin target tissues. These seminal findings confirm bone to be a true endocrine organ. This review is intended to detail the key events commencing from the elucidation of osteocalcin (OC) in bone metabolism to identification of new and emerging candidates that may regulate energy metabolism independently of OC.
Poon CC, Li RW, Seto SW, Kong SK, Ho HP, Hoi MP, et al. In vitro vitamin K2 and 1α,25-dihydroxyvitamin D3 combination enhances osteoblasts anabolism of diabetic mice. Eur J Pharmacol. 2015 Nov 15;767:30-40.
In this study, we evaluated the anabolic effect and the underlying cellular mechanisms involved of vitamin K2 (10 nM) and vitamin D3 (10 nM), alone and in combination, on primary osteoblasts harvested from the iliac crests of lean and obese/diabetic mice. Co-administration of vitamin K2 (10 nM) and vitamin D3 (10 nM) caused an enhancement of calcium deposits in osteoblasts in both strains of mice. Vitamins K2 and 1,25(OH)2D3 co-administration time-dependently (7, 14 and 21 days) increased the levels of bone anabolic markers and bone formation transcription factors, with a greater magnitude of increase observed in osteoblasts of db/db mice. Their results illustrate that vitamins K2 plus D3 combination could be a novel therapeutic strategy in treating diabetes-associated osteoporosis.
Rasekhi H, Karandish M, Jalali MT, Mohammad-Shahi M, Zarei M, Sarki A, et al. The effect of vitamin K1 supplementation on sensitivity and insulin resistance via osteocalcin in prediabetic women: A double-blind randomized controlled clinical trial. Eur J Clin Nutr. 2015 Aug;69(8): 891-5.
A relationship between osteocalcin (OC) levels and factors associated with energy metabolism and insulin resistance has been reported recently. The aim of this study was to investigate whether modulation of ostecalcin via vitamin K1 supplementation would affect glucose metabolism or insulin sensitivity in prediabetic and premenopause women. Eighty-two prediabetic women consumed vitamin K1 supplement(1000 iu) or placebo for 4 weeks. Phylloquinone supplementation increased the serum levels of cOC and decreased ucOC, compared with placebo. Furthermore, intake of phylloquinone supplement led to significant decreases in %ucOC and 2-h post-oral glucose tolerance test (OGTT) glucose, and 2- h post-OGTT insulin level and increased insulin sensitivity index compared with placebo. This study demonstrated that vitamin K1 supplementation for 4 weeks did not affect insulin resistance in premenopausal and prediabetic women but had beneficial effects on glycemic status and insulin sensitivity.
Varsha MKNS, Thiagarajan R, Manikandan R, Dhanasekaran G. Vitamin K1 alleviates streptozotocin-induced type 1 diabetes by mitigating free radical stress, as well as inhibiting NF- NF-kB activation and iNOS expression in rat pancreas. Nutrition. 2015;31:214-222.
This study looked at the action of vitamin K1 against induced diabetes in mice. They found that vitamin K reduced oxidative stress, enhanced antioxidants, and led to an increase in plasma insulin and normal blood glucose levels.
Vollenweider P, von Eckardstein A, Widmann C. HDLs, diabetes, and metabolic syndrome. In: von Eckardstein A, Kardassis D. High density lipoproteins: from biological understanding to clinical exploitation. Springer Open, Cham, 2015;405–421.
Yano S, Nabika T, Nagai A, Hamano T, Yamasaki M, Isomura M, Shiwaku K, et al. Interrelationship between glucose metabolism and undercarboxylated osteocalcin: a cross-sectional study in a community-dwelling population. Asia Pac J Clin Nutr. 2015;24(3):489-95.
They performed a cross-sectional study to investigate the relationship between ucOC and diabetes mellitus (DM). They included 1,870 subjects aged over 50 from participants of a health examination. The study showed a significant association between ucOC and glucose metabolism after correction with bone turnover in a community-dwelling population both in men and women. A low level of ucOC was significantly associated with the presence of DM in both men and women, indicating that ucOC may play an important role in the pathoge esis of DM through the pathways independent of bone metabolism.
Yeap BB, Alfonso H, Chubb AP, Gauci R, Byrnes E, Beilby JP, et al. Higher serum undercarboxylated osteocalcin and other bone turnover markers are associated with reduced diabetes risk and lower estradiol concentrations in older men. J Clin Endocrinol Metab. 2015 Jan;100(1):63-71.
Higher bone remodeling rates are associated with reduced diabetes risk in older men. Higher ucOC is both a marker of bone remodeling and an independent predictor of reduced diabetes risk. This study showed that uncarboxylated osteocalcin is associated with a lower risk of type 2 diabetes.
Shao J, Wang Z, Yang T, Ying H, Zhang Y, Liu S. Bone regulates glucose metabolism as an endocrine organ through osteocalcin. Int J of Endocrinology. 2015; Article ID 967673, 9 pages, 2015. doi:10.1155/2015/967673.
Evidence indicates that skeleton works not only as a structural scaffold but also as an endocrine organ, which regulates several metabolic processes. Bone can also secret hormones, such as osteocalcin (OCN), which promotes proliferation of β cells, insulin secretion, and insulin sensitivity. Additionally OCN can also regulate the fat cells and male gonad endocrine activity and be regulated by insulin and the neural system. In summary, skeleton has an endocrine function via osteocalcin and plays an important role in energy metabolism, especially in glucose metabolism.
Asemi Z, Raygan F, Bahmani F, Rezavandi Z, Talari HR, Rafiee M, et al. The effects of vitamin D, K and calcium co-supplementation on carotid intima-media thickness and metabolic status in overweight type 2 diabetic patients with CHD. Bri J Nutr. 2016 Jul;116(2):286-93.
This study showed that vitamin D, K and calcium co-supplementation for 12 weeks among diabetic patients with CHD had beneficial effects on maximum levels of left Carotic intima media thickness (CIMT) and metabolic status.
Bador KM, Wee LD, Halim SA, Fadi MF, Santhiran P, Rosli NF, et al. Serum osteocalcin in subjects with metabolic syndrome and central obesity. Diabetes Metab Syndr. 2016 Jan-Mar;10(1 Suppl):S42-5.
The aim of this study was to determine if osteocalcin is related to adiposity (fat) and hyperglycaemia in metabolic syndrome irrespective of the presence of diabetes mellitus. Based on medical history 50 out of 90 patients had a diabetes. In this cross-sectional study of subjects with metabolic syndrome and central obesity, low osteocalcin was associated with diabetes but not adiposity.
Brault M, Ray J, Gomez YH, Mantzoros CS, Daskalopoulou SS: Statin treatment and new-onset diabetes: a review of proposed mechanisms. Metabolism 2014;63:735-745.
Chawla A, Chawla R, Jaggi S. Microvasular and macrovascular complications in diabetes mellitus: Distinct or continuum? Indian J Endocrinol Metabol. 2016;20:546–551.
Li J, Zhang H, Yang C, Li Y, Dai Z. An overview of osteocalcin progress. J Bone Miner Metab. 2016 Jul;34(4):367-79.
An increasing amount of data indicate that osteocalcin is an endocrine hormone which regulates energy metabolism, male fertility and brain development. In the present review, we summarize the progress of osteocalcin studies over the past 40 years, focusing on the structure of carboxylated (by vitamin K) and undercarboxylated osteocalcin, new functions and putative receptors, the role of osteocalcin in bone remodeling, specific expression and regulation in osteoblasts. The complexity of osteocalcin in completely, uncompletely and non-carboxylated forms may account for the discrepancies in its tertiary structure and clinical results. There are new physiological functions and mechanisms of action of osteocalcin to be explored and comprehensive investigations are required.
Liabeuf S, Bourron O, Olivier B, Vemeer C, Theuwissen E, Magdeleyns E, et al. Vascular calcification in patients with type 2 diabetes: the involvement of matrix Gla protein. Cardiovasc Diabetol. 2014 Apr 24;13:85.
Matrix Gla protein (MGP) is an important inhibitor of calcification. This study looked at patients with type 2 diabetes and normal or slightly altered kidney function and evaluated levels of inactive, dephospho-uncarboxylated MGP(dp-ucMGP) and total uncarboxylated MGP(t-ucMGP) related to peripheral vascular calcification). High dp-ucMGP levels were independently associated with below-knee arterial calcification score in patients with type 2 diabetes and normal or slightly altered kidney function. Supplementing with vitamin K and raising dp-cMGP would be an effective treatment.
Liang Y, Tan A, Liang D et al. Low osteocalcin level is a risk factor for impaired glucose metabolism in a Chinese male population. J Disabetes Investig. 2016;7(4):522-8.
Manna P, Kalita J. Beneficial role of vitamin K supplementation on insulin sensitivity, glucose metabolism, and the reduced risk of type 2 diabetes: A review. Nutrition. 2016 Jul-aug;32(7-8):732-9.
Micronutritients are gaining acceptance as an important nutritional therapy for the prevention or management of diabetes and its associated health risks. Moderate micronutrient deficiencies can lead to serious health issues. Several human studies reported the beneficial role of vitamin K supplementation in improving insulin sensitivity and glucose tolerance, preventing insulin resistance, and reducing the risk of type 2 diabetes. This review provides an overview of the preclinical and clinical evidences on the effect of vitamin K supplementation in the management of insulin sensitivity and glucose tolerance, and improve the lives of diabetic patients.
Okuyama H, Langsjoen PH, Ohara N, Hashimoto Y, Hamazaki T, Yoshida S, et al. Medicines and vegetable oils as hidden causes of cardiovascular disease and diabetes. Pharmacology. 2016;98:134-170.
These vegetable oils and medicines such as statin and warfarin share, in part, a common mechanism to inhibit vitamin K2-dependent processes, which was interpreted to lead to increased onset of CVD, DM, chronic kidney disease, bone fracture and even mental disorder. Impaired vitamin K2-dependent processes by some types of vegetable oils and medicines, but not plasma high low density lipoprotein cholesterol, were proposed as the cause of CVD, DM and other lifestyle-related diseases. High n-6/n-3 fatty acid ratio of ingested foods, but not animal fats, was emphasized to be another risk factor for many of the diseases described above.
Prasenjit M, Jatin K. Beneficial role of vitamin K supplementation on insulin sensitivity, glucose metabolism, and the reduced risk of type 2 diabetes: A review. Nutrition. 2016;32:732-9.
Micronutrients are gaining acceptance as an important nutritional therapy for the prevention and/or management of diabetes and its associated health risks. Impaired insulin sensitivity and glucose intolerance play a major role in the development of diabetic pathophysiology. Several human studies reported the beneficial role of vitamin K supplementation in improving insulin sensitivity and glucose tolerance, preventing insulin resistance, and reducing the risk of type 2 diabetes (T2 D). This review for the first time provides an overview of the currently available preclinical and clinical evidences on the effect of vitamin K supplementation in the management of insulin sensitivity and glucose tolerance, and will increase understanding for the development of a novel adjuvant therapy to achieve better control of glycemia and improve the lives of diabetic patients.
Zoch ML, Clemens TL, Riddle RC. New insights into the biology of osteocalcin. Bone. 2016 Jan;82:42-9.
Osteocalcin is among the most abundant proteins in bone and is produced exclusively by osteoblasts. Recent studies suggest a broader role for osteocalcin that extends to the regulation of whole body metabolism, reproduction, and cognition. Circulating undercarboxylated osteocalcin, which is regulated by insulin, acts in a feed-forward loop to increase β -cell proliferation as well as insulin production and secretion, while skeletal muscle and adipose tissue respond to osteocalcin by increasing their sensitivity to insulin. Osteocalcin also acts in the brain to increase neurotransmitter production and in the testes to stimulate testosterone production. In this review, we summarize these new discoveries, which suggest that the ability of osteocalcin to function both in bone and as a hormone depends on a novel post-translational mechanism, activated by vitamin K.
Huang L, et al, Osteocalcin improves metabolic profiles, body composition and arterial stiffening in an induced diabetic rat model. Exp Clin Endocrinol Diabetes. 2017;125(4):234-240.
Recent studies have demonstrated the benefits of osteocalcin (OCN) on glucose homeostasis and metabolic dysregulation. However, its role in body composition and vascular function remains unknown. This study was designed to examine changes in metabolic parameters and body composition as well as arterial stiffness after OCN treatment in type 2 diabetic rats. Adult male Sprague Dawley (SD) rats were fed chow or high fat diet (HFD) for 8 weeks, and then diabetes was induced with an injection of low-dose streptozotocin (STZ) and treated daily with intraperitoneal injections of OCN for 12 weeks. Our data showed that OCN treatment improved glucose homeostasis and lipid metabolism. Further analysis revealed that OCN treatment resulted in increased insulin sensitivity. In addition, untreated diabetic rats experienced significant weight loss, whereas OCN-treated rats better maintained body weight. OCN also changed body composition, as evidenced by reduced body fat mass, specifically abdominal fat mass. OCN-treated diabetic rats also demonstrated decreased pulse-wave velocity, indicating of improved arterial stiffness. Taken together, our findings in the current study revealed that OCN therapy prevents arteriosclerosis in an induced diabetic rat model by exerting beneficial effects on glucose levels, insulin sensitivity, lipid metabolites, and body composition changes.
Levinger I, Brennan-Speranza TC, Zulli A, Parker L, Lin X, Lewis JR, et al. Multifaceted interaction of bone, muscle, lifestyle interventions and metabolic and cardiovascular disease: Role of osteocalcin. Osteoporos Int. 2017 Mar;epublished ahead of print. doi:10.1007/s00198-017-3994.
This review looked at the evidence associating osteocalcin and uncarboxylated osteocalcin with metabolic risk and cardiovascular disease. They concluded that current observational and indirect interventional evidence appears to support a relationship between ucOC with metabolic and cardiovascular disease, indicating that low levels of vitamin K are associated with those diseases as well.
Niqwekar S, Bloch DB, Nazarian RM, Vermeer C, Booth SL, Xu D, et al. Vitamin K-dependent carboxylation of matrix gla protein influences the risk of calciphylaxis. J Am Soc Nephrol. 2017 Jan 3;pii:ASN.2016060651. Epub ahead of print.
Matrix Gla protein is a potent inhibitor of vascular calcification. This study investigated how carboxylation influences the risk of calciphylaxis in adult patients on dialysis, and the effects of vitamin K deficiency. Calciphylaxis is a syndrome of calcification of blood vessels, blood clots and skin necrosis, usually seen in patients with chronic kidney disease. They found that each 0.1 unit reduction in carboxylated MGP was associated with more than two-fold increase in calciphylaxis risk. Supplementing with vitamin K to prevent and/or treat calciphylaxis should be explored.
O’Connor EM, Durack E. Osteocalcin: The extra0skeletal role of a vitamin K-dependent protein in glucose metabolism. J Nutr & Intermed Metabolism. 2017;7(C):8-13.
The role of vitamin K in the body has long been associated with blood clotting and coagulation. In more recent times, its role in a range of physiological processes has been described including the regulation of bone and soft tissue calcification, cell growth and proliferation, cognition, inflammation, various oxidative processes and fertility. Vitamin K dependent proteins (VKDP) are present both hepatically and extrahepatically. The role of bone-derived osteocalcin has many physiological roles including, maintenance of bone mass with more recent links to energy metabolism due to the role of the skeleton as an endocrine organ. It has been proposed that insulin binds to bone forming cells (osteoblasts) promoting osteocalcin production which in turn promotes β-cell proliferation, insulin secretion and glucose control. However much of this research has been conducted in animal models with equivocal findings in human studies. This review will discuss the role of osteocalcin in relation to its role in human health, focusing specifically on glucose metabolism.
Razny U, Fedak D, Kiec-Wilk B, Goralska J, Gruca A, Zdzienicka A, et al. Carboxylated and undercarboxylated osteocalcin in metabolic complications of human obesity and prediabetes. Diabetes-metabolism research and reviews. 2017;33(3):e2862.
This study found a significantly lower concentration of carboxylated osteocalcin (Gla-OC) in obese patients when compared with the nonobese control group, although osteocalcin levels were similar in both groups. Their findings confirmed osteocalcin’s role in bone restructuring, metabolism regulation, in addition to possessing anti-inflammatory properties. They suggested that reduced blood levels of Glu-OC may be an early symptom of insulin resistance in obese patients, while the decreased concentration of Gla-OC likes to be connected with appearing of early biomarkers of low-grade inflammation accompanying obesity.
Roumeliotis, S.; Roumeliotis, A.; Panagoutsos, S.; Giannakopoulou, E.; Papanas, N.; Manolopoulos, V.G.; Passadakis, P.; Tavridou, A. Matrix Gla protein T-138C polymorphism is associated with carotid intima media thickness and predicts mortality in patients with diabetic nephropathy. J. Diabetes Complicat. 2017, 31, 1527–1532
Sardana M, Vasim I, Varakantam S, Kewan U, Tariq A, Koppula MR, et al. Inactive matrix Gla-protein and arterial stiffness in type 2 diabetes mellitus. Am J Hypertens. 2017;30:196–201.
Large artery stiffness is increased in diabetes and causes an excessive pulsatile load to the heart. Matrix Gla-Protein (MGP) is an inhibitor of vascular calcification. This study found that circulating dp-ucMGP was independently associated with CF-PWC (carotid-femoral-pulse wave velocity) in type 2 diabetes. This suggests that deficient vitamin K-dependent activation of MGP may lead to artery stiffening and that vitamin K supplementation could be an effective intervention for patients with diabetes.
Schwalfenberg GK. Vitamins K1 and K2: The emerging group of vitamins required for human health. Journal of Nutrition and Metabolism. 2017;2017:6.
Vitamin K supplementation may be useful for a number of chronic conditions that are afflicting North Americans as the population ages, and appears promising in the areas of diabetes, cancer, and osteoarthritis.
Bilotta FL, Arcidiacono B, Messineo S, Greco M, Chiefari E, Britti D, et al. Insulin and osteocalcin: Further evidence for a mutual cross-talk. Endocrine. 2018;59(3):622-32.
Bone has been recognized an as endocrine organism that modulates glucose metabolism by the secretion of osteocalcin, which influences fat deposition and blood sugar levels. Osteocalcin is vitamin K dependent. Using in vitro models of insulin resistance to study osteocalcin gene expression, osteogenic differentiation and insulin secretion, they found a significant correlation between poor glycemic control and reduced levels of serum osteocalcin. Also insulin and low glucose increased osteocalcin gene expression.
Dihingia A, Ozah D, Ghosh S, et al. Vitamin K1 inversely correlates with glycemia and insulin resistance in patients with type 2 diabetes (T2D) and positively regulates SIRT1/AMPK pathway of glucose metabolism in liver of T2D mice and hepatocytes cultured in high glucose. J Nutr Biochem. 2018;52:103–114.
This study examined the relationship between circulating vitamin K1 (VK1) with glycemic status in type 2 diabetes (T2D). This study for the first time demonstrated that circulating VK1 was significantly lower in T2D patients compared to age-matched control subjects, and VK1 levels in T2D were significantly and inversely associated with fasting glucose and insulin resistance. These results suggest that boosting plasma VK1 may reduce the fasting glucose and insulin resistance in T2D patients. Using high-fat-diet-fed T2D animal model, this study further investigated the positive effect of VK1 supplementation on glucose metabolism and examined the underlying molecular mechanism. The results demonstrated that circulating VK1 has a positive effect on lowering fasting glucose and insulin resistance in T2D via regulating SIRT1/AMPK signaling pathway.
Dihingia A, Ozah D, Baruah PK, Kalita J, Manna P. Prophylactic role of vitamin K supplementation on vascular inflammation in type 2 diabetes by regulating the NFâ€κB/Nrf2 pathway: Via activating Gla proteins. Food Func. 2018;9:450–462.
There is no previous study that has examined the relationship between circulating vitamin K1 (VK1) and vascular inflammation in type 2 diabetes (T2D). This study aims to examine the hypothesis that circulating VK1 deficiency may be associated with higher inflammation and insulin resistance in T2D patients and that VK1 supplementation regulates the NF-κB/Nrf2 pathway via activating VK-dependent Gla proteins and reduces vascular inflammation. Using a high fat diet-fed T2D mice model this study further demonstrated that VK1 supplementation (1, 3, 5 μg per kg BW, 8 weeks) dose-dependently decreased the body weight gain, glucose intolerance, fasting glucose, glycated hemoglobin, HOMA-IR, and cytokine secretion (MCP-1 and IL-6) in T2D mice. In conclusion, this study suggests that circulating VK1 has a positive effect in lowering vascular inflammation in T2D by regulating NF-κB/Nrf2 transcription factors via activating VK-dependent Gla proteins.
Guedes JAC, Esteves J, Morais M, Zorn T, Furuya D. Osteocalcin improves insulin resistance and inflammation in obese mice: participation of white adipose tissue and bone. Bone. 2018;115:68-82.
This study determined that osteocalcin improves insulin resistance by decreasing inflammation, and increasing insulin signaling, and in bone, osteocalcin increases the secretion of uncarboxylated osteocalcin by improving insulin resistance in mice.
Puzantian H, Akers SR, Oldland G, Javaid K, Miller R, Ge Y, Ansari B, Lee J, Suri A, Hasmath Z, Townsend R, Chirinos JA. Circulating dephospho-uncarboxylated matrix Gla-protein is associated with kidney dysfunction and arterial stiffness. Am J Hypertens. 2018;31:988–994.
Large artery stiffening is increased in advanced chronic kidney disease (CKD) but likely develops progressively in earlier stages of CKD. Active matrix Gla-protein (MGP) is a potent vitamin K-dependent inhibitor of vascular calcification. This study showed that CKD is associated with increased (inactive) dp-ucMGP, a vitamin K-dependent inhibitor of vascular calcification, which correlates with large artery stiffness. Further studies are needed to assess whether vitamin K2 supplementation represents a suitable therapeutic strategy to prevent or reduce arterial stiffening in CKD.
Urano T, Shiraki M, Kuroda T, Tanaka S, Urano F, Uenishi K, Inoue S. Low serum osteocalcin concentration is associated with incident type 2 diabetes mellitus in Japanese women. J Bone Miner Metab. 2018;36:470-77.
This study investigated whether serum osteocalcin levels are associated with a risk of type 2 diabetes. The results indicated that a decrease in serum osteocalcin levels is associated with future development of Type 2 diabetes, independent of conventional risk factors in Japanese postmenopausal women.
Dumitru N, Carsote M, Cocolos A, Petrova E, Olaru M, Dumitrache C. The link between bone osteocalcin and energy metabolism in a group of postmenopausal women. Current Health Sci J. 2019;45(1):47-51.
There is a dual relationship between bone and tissues involved in energy metabolism. Bone remodeling is an energy consuming process. This study investigated the dual relationship between bones and energy. They found significant correlations between serum osteocalcin and glycemic and lipid metabolism, independent of having diabetes.
Ho H-J, Shirakawa H, Hirahara K, Sone H, Kamiyama S, Komai M. Menaquione-4 amplified glucose-stimulated insulin secretion in isolated mouse pancreatic islets and INS-1 rat insulinoma cells. Int J Mol Sci. 2019 Apr 23;20(8):ijma20081995.
Incretins modulate insulin signaling to regulate energy balance and glucose homeostasis between the fasting state and the fed state. Evidence suggests that the incretin effect is blunted in T2DM patients, most likely as a consequence of the diabetic state, and the disruption of the insulinotropic effect of incretins particularly occurs in glucose homeostatic dysregulation. Vitamin K2 is indispensable for blood coagulation and bone metabolism. Menaquinone-4 (MK-4) is the predominant homolog of vitamin K2, which is present in large amounts in the pancreas, although its function is unclear. Meanwhile, β-cell dysfunction following insulin secretion has been found to decrease in patients with type 2 diabetes mellitus. To elucidate the physiological function of MK-4 in pancreatic β-cells, we studied the effects of MK-4 treatment on isolated mouse pancreatic islets and rat INS-1 cells. Glucose-stimulated insulin secretion significantly increased in isolated islets and INS-1 cells treated with MK-4. It was further clarified that MK-4 enhanced cAMP levels, accompanied by the regulation of the exchange protein directly activated by the cAMP 2 (Epac2)-dependent pathway but not the protein kinase A (PKA)-dependent pathway. A novel function of MK-4 on glucose-stimulated insulin secretion was found, suggesting that MK-4 might act as a potent amplifier of the incretin effect. This study therefore presents a novel potential therapeutic approach for impaired insulinotropic effects.
Hussein AG, Mohamed RH, Shalaby SM, Abd El Motteleb DM. Vitamin K2 alleviates type 2 diabetes in rats by induction of osteocalcin gene expression. Nutrition. 2018 Mar;47:33-8.
Vitamin K is a multifunctional nutrient and various tissues function differently, due to proteins that depend on the presence of vitamin K. Osteocalcin is a bone derived hormone important to the regulation of glucose homeostasis and energy. It is also a protein that depends on vitamin K to function fully. This study looked at the doses of vitamin K that would affect glucose and energy metabolism in rats with Type 2 diabetes. They gave three dose levels for eight weeks. The K2 significantly improved the glycemic status in type 2 diabetic rats, specifically inducing osteocalcin gene expression, which can improve beta cell growth, and other aspects of diabetes. Vitamin K could have therapeutic potential for patients with diabetes.
Li Y, Chen JP, Duan L, Li S. Effect of vitamin K2 on type 2 diabetes mellitus: A review. Diabetes Res Clin Pract. 2018 Feb;136:39-51.
Type 2 diabetes is a major public health problem around the world that frequently presents with microvascular and macrovascular complications. Evidence from observational and clinical trials has shown that supplementing with vitamin K2 reduces the risk for Type 2 diabetes. This review proposes that K2 improves insulin sensitivity through osteocalcin. Vitamin K2 had a better effect than vitamin K1. This would be an important therapeutic strategy.
Lin X, Brennan-Speranza TC, Levinger I, Yeap BB. Undercarboxylated osteocalcin: Experimental and human evidence for a role in glucose homeostasis and muscle regulation of insulin sensitivity. Nutrients. 2018 Jun 29;10(7):847.
This review highlights the role of undercarboxylated osteocalcin, as a hormone that regulates glucose homeostasis and cardiometabolic risk. Emerging evidence implicates undercarboxylated osteocalcin in muscle function and glucose uptake and its therapeutic potential for cardiometabolic diseases. Osteocalcin is a marker of bone turnover and vitamin K intake. Dedicated interventional studies are essential to determine which form of osteocalcin, circulating uncarboxylated OC or the ratio of uncarboxylated OC to total OC would improve insulin sensitivity and thus reduce the risk of Type 2 diabetes in humans.
Mounasree M, Lakshmi MV, Bhavana M, Saaduddin S, Begum Z, Rao AS. A prospective observational study on prevalence of chronic kidney disease in diabetes mellitus. World J Pharm Pharmaceutic Sci. 2018;7(10):1307–1322.
Wei FF, Huang QF, Zhang ZY, Van Keer K, Thijs L, Trenson S, Yang WY. et al. Inactive matrix Gla protein is a novel circulating biomarker predicting retinal arteriolar narrowing in humans. Sci. Rep. 2018;8:15088.
Active matrix Gla protein (MGP), a potent inhibitor of calcification in large arteries, protects against macrovascular complications. Recent studies suggested that active MGP helps maintain the integrity of the renal and myocardial microcirculation, but its role in preserving the retinal microcirculation remains unknown. In 935 randomly recruited Flemish participants they measured plasma desphospho-uncarboxylated MGP (dp–ucMGP), a marker of poor vitamin K status. They found that circulating inactive dp–ucMGP is a long-term predictor of smaller retinal arteriolar diameter in the general population. Our observations highlight the possibility that vitamin K supplementation might promote retinal health.
Thiagarajan R, Varsha M, Srinivasan V, Ravichandran R, Saraboji K. Vitamin K1 prevents diabetic cataract by inhibiting lens aldose reductase 2 (ALR2) activity. Sci. Rep. 2019;9:14684.
Zwakenberg SR, de Jong PA, Bartstra JW, van Asperen R, Westerink J, de Valk H, et al. The effect of Menaquinone-7 supplementation on vascular calcification in patients with diabetes: a randomized, double-blind, placebo-controlled trial. Am J Clin Nutr. 2019;110:883-90.
Zwakenberg SR, Remmelzwaal S, Beulens JWJ, Booth SL, Burgess S, Dashti HSS, et al. Circulating Phylloquinone Concentrations and Risk of Type 2 Diabetes: A Mendelian Randomization Study. Diabetes. 2019;68(1):220–5.
This study investigated the causal relation between circulating phylloquinone (vitamin K1) concentrations and type 2 diabetes. They data from three studies: the European Prospective Investigation into Cancer and Nutrition (EPIC)-InterAct case-cohort study, Diabetes Genetics Replication and Meta-analysis (DIAGRAM), and the UK Biobank, resulting in 69,647 subjects with type 2 diabetes. We calculated a weighted genetic risk score including four genetic variants previously found to be associated with circulating phylloquinone concentrations. Inverse-variance weighted analysis was used to obtain a risk ratio (RR) for the causal relation between circulating phylloquinone concentrations and risk of type 2 diabetes. In conclusion, our study supports that higher circulating phylloquinone may be causally related with lower risk of type 2 diabetes, highlighting the importance of sufficient phylloquinone in the human diet.
Al-Suhaimi EA, Al-Jafary MA. Endocrine roles of vitamin K-dependent-osteocalcin in the correlation between bone metabolism and metabolic disorders. Revs in Endo and Metab Dis. 2020;21:117-125.
Obesity and diabetes are important metabolic diseases and a major public health problem among the world. Studies reported that vitamin K supplementation reduces oxidative stress and metabolic risk biomarkers for diabetes, as well as reduces progression of insulin resistance. Vitamin K-dependent-protein osteocalcin (bone derived hormone) plays crucial roles in energy metabolism. There is a clear association between circulating vitamin k and dependent-osteocalcin concentrations with obesity and risk of Type 2 diabetes. Osteocalcin through molecular mechanisms improves insulin resistance, lipid and glucose profile, and mediate vitamin K positive effects. Insulin also signals osteocalcin to regulate bone mineralization. A missing relationship between bone, glucose and fat metabolism could clarify and manage many metabolic mechanisms. This review focuses on the physiological relationship between vitamin K-dependent-osteocalcin, metabolic and cardiovascular diseases. A better understanding of the mechanism of action of osteocalcin modulated by vitamin K could help in implementing therapeutic drugs to cure metabolic diseases.
Baspinar B, Ayhan NY. Possible beneficial effects of vitamin K and osteocalcin on glucose metabolism. Turkish Med Stud J. 2020;7(2):106-13.
The role of vitamin K in glucose metabolism is thought to be partly due to the modulation of diabetes related cytokines and other metabolic risk markers, as inflammation lies at the bottom of chronic metabolic disease. This review aimed to explain the effect of vitamin and osteocalcin on glucose metabolism and its possible mechanisms of action.
Ho H-J, Komai M, Shirakawa H. Beneficial effects of vitamin K status on glycemic regulation and diabetes Mellitus: A mini-review. Nutrients. 2020 Aug 18;12(8):2485.
This mini-review summarizes the recent insights into the beneficial effects of vitamin K and its possible mechanism of action on insulin sensitivity and glycemic status, thereby suppressing the progression of diabetes mellitus.
Jeannin A-C, Salem J-E, Massy Z, Aubert CE, Vermeer C, Amouyal, et al. Inactive matrix gla protein plasma levels are associated with peripheral neuropathy in Type 2 diabetes. Plos One. 2020;15(5):e0232996.
Diabetic peripheral neuropathy is a frequent and severe complication of diabetes. As Matrix-gla-protein (MGP) is expressed in several components of the nervous system and is involved in some neurological disease, MGP could play a role in peripheral nervous system homeostasis. The aim of this study was to evaluate factors associated with sensitive diabetic neuropathy in Type 2 Diabetes, and, in particular, dephospho-uncarboxylated MGP (dp-ucMGP), the inactive form of MGP. They found an association between diabetic neuropathy and the inactive form of MGP. Since dp-ucMGP is a marker of poor vitamin K status, clinical studies are warranted to explore the potential protective effect of high vitamin K intake on diabetic peripheral neuropathy.
Karamzad N, Faraji E, Adeli S, Carson-Chahhoud K, Zaiai S, Gargari BP. Effects of MK-7 supplementation on glycemic status, anthropometric indices and lipid profile in patient swith Type 2 diabetes: a randomized controlled trial. Diabetes Metab Syndr Obes. 2020;13:2239-49.
This study assessed the effects of MK7 supplementation on glycemic indices, anthropometric indices and lipid profiles among patients with type 2 diabetes. They found that the MK7 significantly improved glycemic indices.
Karamzad N, Maleki V, Carson-Chahhoud K, Azizi S, Sahebkar A, Gargara BP. A systematic review on the mechanisms of vitamin K effects on the complications of diabetes and pre-diabetes. Biofactors. 2020 Jan/Feb;26(1):21-37.
Diabetes mellitus and preâ€diabetes are prevalent endocrine disorders associated with substantial morbidity and premature mortality. Vitamin K is known to have several beneficial effects on complications of diabetes and preâ€diabetes. A systematic search in PubMed, Scopus, Embase, ProQuest, and Google Scholar databases was undertaken to evaluate functional roles of different forms of vitamin K on diabetes and preâ€diabetes. Vitamin K supplementation was found to be associated with significant reductions in blood glucose, increased fasting serum insulin. (reduced hemoglobin A1c, reduced homeostatic model assessmentâ€insulin resistance index (HOMAâ€IR), and increased ßâ€cell function in diabetic animal studies. In conclusion, clinical trials and animal studies confirm that vitamin K supplementation may improve both clinical features and complications of diabetes and preâ€diabetes.
Lin X, Onda D-A, Yang C-H, Lewis JR, Levinger I, Loh K. Roles of bone-derived hormones in type 2 diabetes and cardiovascular pathophysiology. Mol Metab. 2020 Jun 13;40:101040.
This review provides a detailed overview of the physiological and pathological roles of osteocalcin, lipocalin 2, and sclerostin in cardiometabolic health regulation and disease development, with a focus on chronic inflammation.
Riquelme-Gallego B, Garcia-Molina L, Cano'Ibanez N, Sanchez-Delgado G, Andujar-Vera F, et al. Circulating undercarboxylated osteocalcin as estimator of cardiovascular and Type 2 diabetes risk in Metabolic Syndrome patients. Sci Rep. 2020 Feb 4;10(1):1840.
This study looked at the association between serum levels of ucOC and cardiovascular risk in patients with metaboilc syndrome. They found an inverse association between ucOC levels and cardiovascular risk in patients with metabolic syndrome but not yet type 2 diabetes. It appears that ucOC could be a useful tool to identify increased cardiovascular and type 2 diabetes risk in MetS patients.
Sakak FR, Moslehi N, Niroomand M, Mirmiran P. Glycemic control improvement in individuals with type 2 diabetes with vitamin k2 supplementation: a randomized controlled trial. Eur J of Nutr. 2020;https://doi.org/10.1007/s00394-020-02419-6.
This study aimed to investigate the effects of vitamin K2 supplementation in the form of menaquinone-7 (MK-7) on glucose, insulin, and lipid metabolism in patients with type 2 diabetes mellitus (T2DM). The number of participants achieved the target levels of glycemic control based on FPG, and HbA1c concentrations were significantly higher in the vitamin K2 group compared to the placebo group. Daily intake of 360 µg Vitamin K2 in the form of MK-7 for 12-weeks reduces FPG and HbA1c in patients with T2DM but does not have a lipid-lowering effect.
Tsugawa N, Shiraki M. Vitamin K nutrition and bone health. Nutrients. 2020;12(7):1909.
This review discusses the assessment of vitamin K sufficiency and the role of vitamin K in bone health. Vitamin K supplementation address deficiencies and is believed to promote bone health, and future work on fracture risk reduction are warranted.
Written by RPT 1/2/13















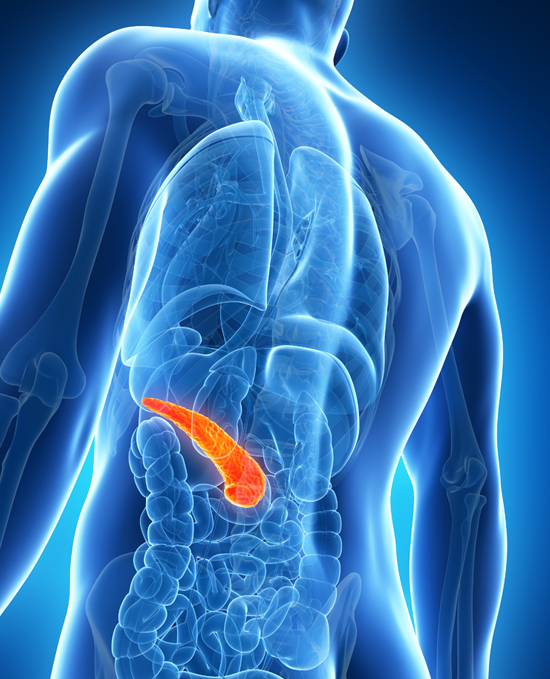
 Web Design: www.superiorweb.net
Web Design: www.superiorweb.net